Back to Journals » Clinical Interventions in Aging » Volume 17
A Comparison of Cerebrospinal Fluid Beta-Amyloid and Tau in Idiopathic Normal Pressure Hydrocephalus and Neurodegenerative Dementias
Authors Said HM, Kaya D , Yavuz I , Dost FS , Altun ZS, Isik AT
Received 1 February 2022
Accepted for publication 2 April 2022
Published 11 April 2022 Volume 2022:17 Pages 467—477
DOI https://doi.org/10.2147/CIA.S360736
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Maddalena Illario
Harun Muayad Said,1 Derya Kaya,2,3 Idil Yavuz,4 Fatma Sena Dost,2,3 Zekiye Sultan Altun,5 Ahmet Turan Isik2,3
1Department of Molecular Medicine, Graduate School of Health Sciences, Dokuz Eylul University, Izmir, Turkey; 2Unit for Brain Aging and Dementia, Department of Geriatric Medicine, Faculty of Medicine, Dokuz Eylul University, Izmir, Turkey; 3Geriatric Science Association, Izmir, Turkey; 4Department of Statistics, Dokuz Eylul University, Faculty of Science, Izmir, Turkey; 5Department of Basic Oncology, Oncology Institute, Faculty of Medicine, Dokuz Eylul University, Izmir, Turkey
Correspondence: Ahmet Turan Isik, Unit for Brain Aging and Dementia, Department of Geriatric Medicine, Faculty of Medicine, Dokuz Eylul University, Izmir, Turkey, Tel +90 232 412 43 41, Fax +90 232 412 43 49, Email [email protected]
Purpose: Idiopathic normal pressure hydrocephalus (iNPH) is the leading reversible cause of cognitive impairment and gait disturbance that has similar clinical manifestations and accompanies to major neurodegenerative disorders in older adults. We aimed to investigate whether cerebrospinal fluid (CSF) biomarker for Alzheimer’s disease (AD) may be useful in the differential diagnosis of iNPH.
Patients and Methods: Amyloid-beta (Aß) 42 and 40, total tau (t-tau), phosphorylated tau (p-tau) were measured via ELISA in 192 consecutive CSF samples of patients with iNPH (n=80), AD (n=48), frontotemporal dementia (FTD) (n=34), Lewy body diseases (LBDs) (n=30) consisting of Parkinson’s disease dementia and dementia with Lewy bodies.
Results: The mean age of the study population was 75.6± 7.7 years, and 54.2% were female. CSF Aβ42 levels were significantly higher, and p-tau and t-tau levels were lower in iNPH patients than in those with AD and LBDs patients. Additionally, iNPH patients had significantly higher levels of t-tau than those with FTD. Age and sex-adjusted multi-nominal regression analysis revealed that the odds of having AD relative to iNPH decreased by 37% when the Aβ42 level increased by one standard deviation (SD), and the odds of having LBDs relative to iNPH decreased by 47%. The odds of having LBDs relative to iNPH increased 76% when the p-tau level increased 1SD. It is 2.5 times more likely for a patient to have LBD relative to NPH and 2.1 times more likely to have AD relative to iNPH when the t-tau value increased 1SD.
Conclusion: Our results suggest that levels of CSF Aβ42, p-tau, and t-tau, in particularly decreased t-tau, are of potential value in differentiating iNPH from LBDs and also confirm previous studies reporting t-tau level is lower and Aβ42 level is higher in iNPH than in AD.
Keywords: Alzheimer’s disease, beta-amyloid 42, phosphorylated tau, Tau, frontotemporal dementia, Lewy body diseases, cerebrospinal fluid, biomarker, Parkinson’s disease dementia, dementia with Lewy body, differential diagnosis
Introduction
Idiopathic normal pressure hydrocephalus (iNPH) is a progressive neurodegenerative disorder with no identifiable cause characterized by a triad composed of gait, memory, urinary complaints, and enlarged cerebral ventricles on the brain imaging.1,2 Its frequency increases with age rising to 6% or 8.9% of prevalence after the age of 80 years in the population-based studies.2,3 Moreover, the prevalence of iNPH in Asia, particularly in Japan, is higher than in Europe or North America.4 The primary treatment of the disorder is shunt surgery in which cerebrospinal fluid (CSF) is diverted into the peritoneal or atrial cavity4–8, and between 60% to 80% of patients improve following this disease-specific treatment.7 Studies also showed that increasing age did not decrease the chance of shunting being successful, with an 83% chance of improvement on the timed-walk test at six months.8 Even there is a practical approach via serial cerebrospinal fluid removal procedure for those older iNPH patients who refuse or have a contraindication to the surgery. The deterioration of gait disturbance was improved, and cognitive decline was stabilized by applying recurrent CSF removal in those unshunted patients with iNPH.9 Yet, unfortunately, the vast majority of patients with iNPH are underrecognized or misdiagnosed even though it is a leading cause of a treatable form of dementia, poor gait, and urinary dysfunction in older adults.
One of the most remarkable reasons for this discrepancy between the diagnosis and treatment success rates is a diagnostic challenge in iNPH.8,10 Despite the well-known characteristics of the disease, sometimes it may be difficult to distinguish it from other neurodegenerative ones commonly seen in older patients with other co-occurring comorbidities. Alzheimer’s disease (AD) is one of those illnesses, and iNPH and AD share common features in clinical appearance, laboratory, and imaging, such as executive dysfunction, impairment in attention and short-term memory, low amyloid-beta 42 (Aß42) levels in CSF, and ventriculomegaly.10,11 Functional neuroimaging studies revealed alterations related to the default mode network (DMN) connectivity network dynamics in the pathophysiology of these diseases.12 Also, cognitive symptoms of iNPH overlap with those of frontotemporal dementias, including psychomotor slowing, difficulty with problem-solving, decreased fine motor speed or accuracy, behavioral or personality changes.7,13 This fact may be attributed to a characteristic pattern of regional cerebral blood flow reduction with frontal lobe hypoperfusion in iNPH.14 Apart from AD and FTD, some features in iNPH resemble those observed in Parkinson’s disease dementia (PDD) or dementia with Lewy bodies (DLB), such as difficulty in gait initiation, shuffling, festination, en bloc turning, falling, retropulsion, or retropulsion together with impaired cognition and urinary urgency/incontinence. Furthermore, patients with iNPH were reported to have visuospatial and visuoperceptual deficits in the neuropsychological assessments, which extend beyond frontal-executive dysfunction,15,16 and is similar to those seen in DLB and PDD.
On the other hand, considering that iNPH can frequently accompany these neurodegenerative diseases,7,17 (differential) diagnostic workup is of paramount importance to confirm iNPH regardless of the presence of these comorbidities, which means that such patients have a chance to relieve iNPH related symptoms even at least in geriatrics practice.18
For this purpose, CSF biomarkers for AD pathology may be helpful because previous studies showed that Aß42, Aß40, phosphorylated tau (p-tau), and total tau (t-tau) proteins seem to separate iNPH, which may have individual CSF composition changes, from patients with some of those diseases.10,19–21 Therefore, in this study, as a geriatric memory referral center in a university hospital, we aimed to report our experience on CSF biomarker for AD pathology analysis in patients with iNPH and other common confusing causes of gait, memory, and urinary disturbances including AD, FTD and Lewy body diseases (LBDs).
Materials and Methods
Participants
One hundred ninety-two patients over 60 years of age with an existing cerebrospinal fluid (CSF) biochemical analysis as part of their clinical diagnostic investigation between January 2016 and January 2019, at the Department of Geriatrics, Dokuz Eylul University, Izmir, Turkey, were included in this retrospective study. Mixed subjects were excluded. There were 80 patients with probable iNPH, 48 with AD, 34 with FTDs, and 30 with PDD and DLB together denoted LBDs. The study was approved by the ethics committee of Dokuz Eylul University Faculty of Medicine (2014/38-33), and participants provided written consent by the principles of the Declaration of Helsinki.
Probable INPH was diagnosed according to the international INPH guidelines.6 The diagnostic criteria were (a) gait or balance disturbance, cognitive disturbance, or impaired urinary continence, with an insidious onset of symptoms over at least three months or more (b) enlarged ventricles on cranial imaging with Evans’ index >0.3 and at least one of the four supporting features reported as temporal horn enlargement, periventricular signal changes, periventricular edema, or an aqueductal/fourth ventricular flow void; (c) lumbar CSF opening pressure below 18 mmHg. Additionally, the tap test was performed in all iNPH cases since it is our routine practice for the patients to confirm the diagnosis, which is one of the most disseminated worldwide, for it is easily performed and cost-effective.22 The diagnosis of probable AD was made according to the National Institute on Aging-Alzheimer’s Association workgroup’s criteria.23 FTD patients included those with behavioral variant FTD (bvFTD), progressive supranuclear palsy (PSP), and corticobasal degeneration (CBD) and were diagnosed as follows: the diagnosis of bvFTD was based on clinical, neuropsychological, and neuroimaging findings,24 probable or definite (PSP) according to the National Institute of Neurological Disorders and Stroke and Society for Progressive Supranuclear Palsy, clinical criteria,25 and probable CBD according to Armstrong et al.26 PDD was diagnosed by Movement Disorder Society Task Force’s clinical diagnostic criteria, and practical recommendations27,28 and probable DLB was made according to the fourth consortium of DLB consensus.29 All patients had neuroimaging, and demographic characteristics and clinical including age, gender, and mini mental state examination (MMSE) scores were collected.
CSF Biochemical Evaluation
CSF concentrations of total Aß42, Aß40, p-tau, and t-tau proteins were analyzed. Briefly, CSF samples were collected in sterile polypropylene tubes, immediately centrifuged at 2000 g for 10 min at four °C, aliquoted into polypropylene tubes, and stored at −80 degrees until analysis. CSF Aß42, Aß40, and t-tau were measured using the manufacturer’s commercially available Euroimmun ELISA kits (Euroimmun, Lubeck, Germany). All samples were measured in duplicates. The mean intra-assay and inter-assay coefficients of variation (CVs) of the assay ranges for t-tau were 3.9–6.5% and 6.6–9.3%, respectively. The reference detection limit of the test kit for Aß40 was 41 pg/mL, and Aß42 was 6.5 pg/mL. According to the manufacturer’s instructions, the level of p-tau was analyzed using commercially available ELISA kits (INNOTEST phosphorylated-Tau181; Fujirebio, Ghent, Belgium). The assay’s mean intra-assay and inter-assay coefficients of variation (CVs) were 2.5% and 5.4%. The ratio of Aβ1–42/Total tau and Aβ1–42 /Aβ1–40 were also calculated. Cerebrospinal fluid Aß42 concentration under 550 pg/mL, CSF t-tau above 452 pg/mL, and CSF-p-tau above 61 pg/mL were considered pathological for AD profile. The results were analyzed blinded to the diagnosis of the patients.
Statistical Analysis
Statistical analysis of the data was performed with IBM SPSS Statistics for Windows, Version 24.0. Amork, NY: IBM Corp. Descriptive statistics were used to explore the sample characteristics. Continuous data were expressed as the median (range) and as mean± standard deviation when they were not normally distributed and normally distributed, respectively. The CSF levels of the related proteins among disease groups were compared using the Kruskal Wallis test, and followed by post hoc Mann Whitney U-tests. Gender distribution was analyzed by the Pearson Chi-Square test. Unadjusted and age and sex-adjusted multinomial logistic regression models were built to investigate the relationship between the standardized independent variables and disease groups expressed as a categorical variable. In all analyses, p< 0.05 was considered statistically significant, and interval estimators were provided with 95% confidence.
Results
Demographic and Clinical Variables
A total of 48 patients with AD, 80 patients with iNPH, 34 patients with FTD (20 bvFTD, 8 PSP, and 6 CBD), and 30 patients with LBDs (17 DLB and 13 PDD) were included in this study. The mean age of the study population was 75.6±7.7 years, and 54.2% (n=104) were female. There was a significant difference among patients regarding age and gender distribution (p<0.001 and p=0.002, respectively, with One-Way-ANOVA). The mean age was significantly lower in patients with FTD than in those with iNPH (p<0.001) and LBDs (p=0.005) in the post hoc analysis. It was also revealed that the female gender was significantly higher in patients with AD than in those with iNPH (p=0.004), FTD (p=0.001), LBDs (p=0.001).
The demographic and clinical features of the participants were shown in Table 1, and Figure 1 and Table 2 shows the demographic, clinical and neuropsychological features of the patients with iNPH.
 |
Table 1 Demographic and CSF Biomarker Data in the Diagnostic Groups |
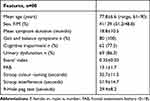 |
Table 2 Demographic, Clinical and Neuropsychological Characteristics of Patients with Idiopathic Normal Pressure Hydrocephalus |
MMSE scores differed among groups p<0.001 (One-Way ANOVA), which were significantly higher in patients with iNPH than in those with AD (p= 0.019), with FTD (p=0.029), and with LBDs (p<0.001).
CSF AD Biomarker Levels
Table 1 and Figure 1 show the details of the AD biomarker levels in each patient group. In summary, CSF Aβ42 levels differed significantly in iNPH patients from the other non-iNPH patients, and the levels were higher in iNPH patients than those of AD and LBDs patients. CSF p-tau and t-tau levels were found to be significantly lower in patients with iNPH when compared to those with AD and LBDs. Additionally, iNPH patients had significantly lower levels of t-tau than those with FTD. And the ratio of Aβ42/t-tau was higher in patients with iNPH than in each of the other non-iNPH patient groups.
Multinomial Logistic Regression Model Analysis
Unadjusted analysis results revealed that the odds of having AD relative to iNPH decreases by 32% when the Aβ42 value increases one standard deviation (SD). The odds of having LBD relative to iNPH increases by 73% when the p-tau181 value increases one SD. It is 2.4 times more likely for a patient to have LBD relative to iNPH when the t-tau value increases one SD (Table 3).
 |
Table 3 Multi-Nominal Logistic Regression Results for Idiopathic Normal Pressure Hydrocephalus |
Age and sex-adjusted analysis revealed that the odds of having AD relative to iNPH decreases by 37% when the Aβ42 value increases one SD, and the odds of having LBDs relative to iNPH decrease by 47%. The odds of having LBDs relative to iNPH increases by 76% when the p-tau181 value increases one SD. It is 2.5 times more likely for a patient to have LBD relative to iNPH and 2.1 times more likely to have AD relative to iNPH when the t-tau value increases one SD (Table 4).
 |
Table 4 Age and Gender Adjusted Multi-Nominal Logistic Regression Results for Idiopathic Normal Pressure Hydrocephalus |
Discussion
The current study demonstrated that CSF Aβ42, p-tau, and t-tau levels may help distinguish patients with iNPH from those with LBDs and confirmed that patients with iNPH had higher Aβ42 levels and lower t-tau levels when compared to those with AD.
Clinical findings similar to AD, LBDs, and FTD can be observed in iNPH, which is one of the causes of reversible cognitive dysfunction and gait disturbance. Namely, it may show clinical presentations similar to FTD due to frontal-type cognitive impairment, AD due to general memory impairment symptoms, and PDD or DLB due to gait apraxia and psychomotor slowing. Although the basis of the relationship between cognitive impairment, brain shrinkage, and excess of fluid (ventriculomegaly) dates back to the times of Hippocrates, iNPH in mixed cases appears to be overshadowed by primary neurodegeneration. Considering that there is no definitive treatment for these three progressive diseases, which are the most common causes of irreversible cognitive dysfunction, it is essential to eliminate the clinical worsening of iNPH in the current clinical picture, both for patients and their caregivers.
In cases where the clinic is not very distinctive, CSF biomarkers may play an essential role in the differential diagnosis. For AD, there is an established pattern using decreased Aβ42, elevated p-tau, and t-tau levels.30,31 The biomarkers for AD increase the diagnostic confidence up to 86% and lead to diagnostic (32.5%) and treatment changes (32.5%).32 A recent meta-analysis,21 as in our results, found that CSF Aβ42 levels were higher in patients with iNPH than in AD patients. Indeed, low levels of CSF Aβ42 are thought to occur due to the accumulation of these least soluble Aβ peptides into insoluble plaques in the AD brain.33 However, prior studies reported that low Aβ42 levels in iNPH could be related to the impaired elimination of Aβ42 from the brain to the CSF compartment as a final consequence of retrograde CSF flow dynamics in the disease pathophysiology.34,35 On the other hand, biopsy studies from iNPH brains revealed that some patients had AD-related neuropathological findings.36–38 Recent data suggest an association between CSF changes typical of AD and NPH changes, suggesting a marked coincidence of AD and NPH. Furthermore, fortunately, those iNPH patients with CSF biomarker signature typical for AD were reported to have improved upon a spinal tap, in contrast to those with no such CSF changes.39 Indeed, it is not yet well understood why some iNPH patients have CSF biomarker profile or pathology typical of AD, but some do not. A previous study suggested that the APOE ε4 carrier status independently predicted the presence of cortical Aβ in patients with iNPH.38 From this perspective, for those patients, it may be speculated that the reason for the AD-specific increase in CSF t-tau and p-tau concentrations is that neuronal CSF tau protein secretion may be induced by alzheimerogenic factors such as A β42,40,41 and, from a preclinical point of view, Aβ may appear to function as a p-tau pathology accelerator via prion protein spreading,42 which might also be the case in those iNPH patients.
Therefore, to discriminate iNPH from AD, we think a combination analysis would be more informative than those with Aβ42 only. Accordingly, in a recent study, a CSF pattern of a combination of t-tau, Aβ40, and an astroglia marker for iNPH was reported to have good diagnostic predictivity for discriminating from non-iNPH disorders, including AD, FTD, and vascular dementia (VAD).19 Apart from the biomarkers in this study, some other biomarkers in CSF, such as leucine-serine-lysine-leucine peptide, myelin basic protein, neurofilament light protein, protein tyrosine phosphatase receptor type Q, are being investigated to enhance the accuracy of diagnosis and to predict shunt surgery outcomes in patients with iNPH.11,20,43 Meanwhile, the exploration of more effective therapies has become the focus for many researchers to provide new orientations for animal research and clinical practice.44 For instance, the TGF-β pathway was tried to be interfered with as a means to treat hydrocephalus in animal models.45 Similar efforts are also in question for AD, as a very recent study provided a potential therapeutic strategy for synaptic and memory deficits via a pathway in Aβ-induced pathological alterations in AD.46
Our results were consistent with the finding that patients with AD and FTD had higher tau proteins than those with iNPH. Meanwhile, as FTD is regarded as non-AD tauopathies, increased CSF level of t-tau protein in FTD is an expected finding compared to iNPH. Nevertheless, increased CSF levels of p-tau and t-tau are not direct markers of these non-AD tauopathies since they are characterized with tau protein aggregates in neurons and glial cells, without this being reflected in the extracellular fluid, but, with keeping in mind which phospho-form of tau, a complex molecule, to measure is of importance.40,41
Furthermore, it is observed that our patients with synucleinopathies, LBDs, also had elevated tau levels. It was 2.5 times more likely for a patient to have LBDs than iNPH when the t-tau level increased one SD. Additionally, the odds of having LBDs relative to iNPH increased by 76% when the p-tau level increased one SD. Increased tau levels in CSF are believed to result from its release from damaged and dying neurons.47 The low tau proteins in iNPH might be due to its dilution in CSF35 or reduced periventricular zone metabolism and decreased elimination of the protein from the extracellular fluid due to reduced centripetal flow of extracellular fluid caused by the retrograde CSF dynamic in iNPH.36,48 Apart from the rather known biochemical relationship between tau proteins and iNPH, the role of tau pathology remains largely an unresolved issue in LBDs.49 Yet, it was reported that there was an interaction between tau fibrillation and insoluble α-synuclein protein deposits in brains with LBDs. Tau pathology was accelerated with different additional cofactors as α-synuclein promotes its fibrillization and deposition.50 The interaction probably ended with a final common pathway for neurodegeneration which means that the increased levels in CSF total tau in LBDs probably reflects neuronal damage.50,51
Our study has several strengths: To begin with, it is the first to evaluate the biomarkers in patients with PDD, LBD, and iNPH to provide any additional information for discriminating these diseases from each other. To the best of our knowledge, our study is the first to show that CSF Aβ42, p-tau, and t-tau levels are highly useful as complementary examinations during the differential diagnosis of iNPH and LBDs, even though they are not specific indicators of iNPH. In addition, we included only older adults in contrast to the prior studies that also had younger patients.19 We thought that age is an essential contributing factor in all these diseases’ pathophysiology. On the other hand, the study has limitations to consider: First, the pathological verification of the clinical diagnoses was unavailable; thus, although we paid particular attention to the inclusion of samples from “pure” cases, it is known that co-pathology is not uncommon in iNPH.35 Second, since our unit is a geriatric memory referral center in a university hospital, our results may not be generalized and need to be confirmed in larger CSF samples from patients with LBDs. Additionally, a lack of healthy controls is another limitation.
In conclusion, our results indicate that CSF biomarkers typical for AD may help improve the identification of iNPH in the differential diagnosis, particularly with the patients having LBDs, with the latter having more than twice folds CSF t-tau compared to the latter to iNPH patients. Additionally, our findings confirm the studies that reported that iNPH patients had higher levels of CSF Aβ42 protein than in those patients with AD and lower levels of tau-related proteins than in those patients with AD and FTD.
Acknowledgments
The authors would like to acknowledge Feyza Mutlay and Ayse Fadiloglu for their assistance in recruiting patients’ data for this research study. The authors would also like to thank all participants for their involvement and participation in the study.
Funding
This work was supported by the scientific investigations support unit of Dokuz Eylül University Izmir, Turkey (Project no: 2016.KB.SAG.009).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hakim S, Venegas JG, Burton JD. The physics of the cranial cavity, hydrocephalus, and normal pressure hydrocephalus: mechanical interpretation and mathematical model. Surg Neurol. 1976;5:187–210.
2. Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelsø C. Prevalence of idiopathic normal-pressure hydrocephalus. Neurology. 2014;82(16):1449–1454. doi:10.1212/WNL.0000000000000342
3. Andersson J, Rosell M, Kockum K, Lilja-Lund O, Söderström L, Laurell K. Prevalence of idiopathic normal pressure hydrocephalus: a prospective, population-based study. PLoS One. 2019;14(5):e0217705. doi:10.1371/journal.pone.0217705
4. Nakajima M, Yamada S, Miyajima M, et al. Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus (Third Edition): endorsed by the Japanese Society of Normal Pressure Hydrocephalus. Neurol Med Chir (Tokyo). 2021;61(2):63–97. doi:10.2176/nmc.st.2020-0292
5. Toma AK, Papadopoulos MC, Stapleton S, Kitchen ND, Watkins LD. Systematic review of the outcome of shunt surgery in idiopathic normal-pressure hydrocephalus. Acta Neurochir. 2013;155(10):1977–1980. doi:10.1007/s00701-013-1835-5
6. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57(3 Suppl):S4–v. doi:10.1227/01.neu.0000168185.29659.c5
7. Williams MA, Malm J. Diagnosis and treatment of idiopathic normal pressure hydrocephalus. Continuum. 2016;22(2Dementia):579–599. doi:10.1212/CON.0000000000000305
8. Halperin JJ, Kurlan R, Schwalb JM, Cusimano MD, Gronseth G, Gloss D. Practice guideline: idiopathic normal pressure hydrocephalus: response to shunting and predictors of response: report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2015;85(23):2063–2071. Erratum in: Neurology. 2016;86(8):793. doi:10.1212/WNL.0000000000002193
9. Isik AT, Kaya D, Ates Bulut E, Dokuzlar O, Soysal P. The outcomes of serial cerebrospinal fluid removal in elderly patients with idiopathic normal pressure hydrocephalus. Clin Interv Aging. 2019;14:2063–2069. doi:10.2147/CIA.S228257
10. Manniche C, Hejl AM, Hasselbalch SG, Simonsen AH. Cerebrospinal fluid biomarkers in idiopathic normal pressure hydrocephalus versus Alzheimer’s disease and subcortical ischemic vascular disease: a systematic review. J Alzheimers Dis. 2019;68(1):267–279. doi:10.3233/JAD-180816
11. Schirinzi T, Sancesario GM, Di Lazzaro G, et al. Cerebrospinal fluid biomarkers profile of idiopathic normal pressure hydrocephalus. J Neural Transm. 2018;125(4):673–679. doi:10.1007/s00702-018-1842-z
12. Griffa A, Bommarito G, Assal F, Herrmann FR, Van De Ville D, Allali G. Dynamic functional networks in idiopathic normal pressure hydrocephalus: alterations and reversibility by CSF tap test. Hum Brain Mapp. 2021;42(5):1485–1502. doi:10.1002/hbm.25308
13. Kaya D, Erken N, Ontan MS, Altun ZS, Isik AT. The applause sign in elderly patients with idiopathic normal pressure hydrocephalus [published online ahead of print, 2020 Sep 10]. Appl Neuropsychol Adult. 2020;1–6. doi:10.1080/23279095.2020.1818563
14. Sasaki H, Ishii K, Kono AK, et al. Cerebral perfusion pattern of idiopathic normal pressure hydrocephalus studied by SPECT and statistical brain mapping. Ann Nucl Med. 2007;21:39. doi:10.1007/BF03033998
15. Bugalho P, Alves L, Miguel R, Ribeiro O. Profile of cognitive dysfunction and relation with gait disturbance in normal pressure hydrocephalus. Clin Neurol Neurosurg. 2014;118:83–88. doi:10.1016/j.clineuro.2014.01.006
16. Saito M, Nishio Y, Kanno S, et al. Cognitive profile of idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Dis Extra. 2011;1(1):202–211. doi:10.1159/000328924
17. Kaya D, Isik AT. The significance of cerebral comorbidities in idiopathic normal pressure hydrocephalus. Biomed J Sci Tech Res. 2018;6(3):5207–5209. doi:10.26717/BJSTR.2018.06.001340
18. Kanemoto H, Mori E, Tanaka T, et al. Cerebrospinal fluid amyloid beta and response of cognition to a tap test in idiopathic normal pressure hydrocephalus: a case-control study [published online ahead of print, 2021 Aug 17]. Int Psychogeriatr. 2021:1–9. doi:10.1017/S1041610221000661
19. Jeppsson A, Wikkelsö C, Blennow K, et al. CSF biomarkers distinguish idiopathic normal pressure hydrocephalus from its mimics. J Neurol Neurosurg Psychiatry. 2019;90(10):1117–1123. doi:10.1136/jnnp-2019-320826
20. Tan C, Wang X, Wang Y, et al. The pathogenesis based on the glymphatic system, diagnosis, and treatment of idiopathic normal pressure hydrocephalus. Clin Interv Aging. 2021;16:139–153. doi:10.2147/CIA.S290709
21. Chen Z, Liu C, Zhang J, Relkin N, Xing Y, Li Y. Cerebrospinal fluid Aβ42, t-tau, and p-tau levels in the differential diagnosis of idiopathic normal-pressure hydrocephalus: a systematic review and meta-analysis. Fluids Barriers CNS. 2017;14(1):13. doi:10.1186/s12987-017-0062-5
22. Oliveira LM, Nitrini R, Román GC. Normal-pressure hydrocephalus: a critical review [published correction appears in Dement Neuropsychol. 2019 Jul Sep;13(3):361]. Dement Neuropsychol. 2019;13(2):133–143. doi:10.1590/1980
23. McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–269. doi:10.1016/j.jalz.2011.03.005
24. Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–2477. doi:10.1093/brain/awr179
25. Litvan I, Bhatia KP, Burn DJ, et al. Movement Disorders Society Scientific Issues Committee report: SIC task force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord. 2003;18(5):467–486. doi:10.1002/mds.10459
26. Armstrong MJ, Litvan I, Lang AE, et al. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013;80(5):496–503. doi:10.1212/WNL.0b013e31827f0fd1
27. Emre M, Aarsland D, Brown R, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007;22(12):1689–1837. doi:10.1002/mds.21507
28. Dubois B, Burn D, Goetz C, et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the movement disorder society task force. Mov Disord. 2007;22(16):2314–2324. doi:10.1002/mds.21844
29. McKeith IG, Boeve BF, Dickson DW, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB Consortium. Neurology. 2017;89(1):88–100.19. doi:10.1212/WNL.0000000000004058
30. Consensus report of the Working Group on: Biological Markers of Alzheimer’s Disease. The Ronald and Nancy Reagan research institute of the Alzheimer’s association and the national institute on aging working group. Neurobiol Aging. 1998;19:109–116.
31. Frank RA, Galasko D, Hampel H, et al. Biological markers for therapeutic trials in Alzheimer’s disease—proceedings of the Biological Measures Working Group: NIA initiative on neuroimaging in Alzheimer’s Disease. Neurobiol Aging. 2003;24:521–536. doi:10.1016/S0197-4580(03)00002-2
32. Falgàs N, Tort-Merino A, Balasa M, et al. Clinical applicability of diagnostic biomarkers in early-onset cognitive impairment. Eur J Neurol. 2019;26(8):1098–1104. doi:10.1111/ene.13945
33. Jack CR Jr, Bennett DA, Blennow K, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539–547. doi:10.1212/WNL.0000000000002923
34. Graff-Radford NR. Alzheimer CSF biomarkers may be misleading in normal-pressure hydrocephalus. Neurology. 2014;83(17):1573–1575. doi:10.1212/WNL.0000000000000916
35. Jeppsson A, Zetterberg H, Blennow K, Wikkelsø C. Idiopathic normal-pressure hydrocephalus: pathophysiology and diagnosis by CSF biomarkers. Neurology. 2013;80(15):1385–1392. doi:10.1212/WNL.0b013e31828c2fda
36. Leinonen V, Koivisto AM, Savolainen S, et al. Post-mortem findings in 10 patients with presumed normal-pressure hydrocephalus and review of the literature. Neuropathol Appl Neurobiol. 2012;38(1):72–86. doi:10.1111/j.1365-2990.2011.01195.x
37. Elobeid A, Laurell K, Cesarini KG, Alafuzoff I. Correlations between mini-mental state examination score, cerebrospinal fluid biomarkers, and pathology observed in brain biopsies of patients with normal-pressure hydrocephalus. J Neuropathol Exp Neurol. 2015;74(5):470–479. doi:10.1097/NEN.0000000000000191
38. Seppälä TT, Nerg O, Koivisto AM, et al. CSF biomarkers for Alzheimer disease correlate with cortical brain biopsy findings. Neurology. 2012;78(20):1568–1575. doi:10.1212/WNL.0b013e3182563bd0
39. Müller-Schmitz K, Krasavina-Loka N, Yardimci T, et al. Normal pressure hydrocephalus associated with Alzheimer’s disease. Ann Neurol. 2020;88(4):703–711. doi:10.1002/ana.25847
40. Zetterberg H. Review: tau in biofluids - relation to pathology, imaging and clinical features. Neuropathol Appl Neurobiol. 2017;43(3):194–199. doi:10.1111/nan.12378
41. Zetterberg H, Blennow K. Moving fluid biomarkers for Alzheimer’s disease from research tools to routine clinical diagnostics. Mol Neurodegener. 2021;16(1):10. doi:10.1186/s13024-021-00430-x
42. Gomes LA, Hipp SA, Rijal Upadhaya A, et al. Aβ-induced acceleration of Alzheimer-related τ-pathology spreading and its association with prion protein. Acta Neuropathol. 2019;138(6):913–941. doi:10.1007/s00401-019-02053-5
43. Nakajima M, Rauramaa T, Mäkinen PM, et al. Protein tyrosine phosphatase receptor type Q in cerebrospinal fluid reflects ependymal cell dysfunction and is a potential biomarker for adult chronic hydrocephalus. Eur J Neurol. 2021;28(2):389–400. doi:10.1111/ene.14575
44. Wang C, Wang X, Tan C, et al. Novel therapeutics for hydrocephalus: insights from animal models. CNS Neurosci Ther. 2021;27(9):1012–1022. doi:10.1111/cns.13695
45. Zhan C, Xiao G, Zhang X, Chen X, Zhang Z, Liu J. Decreased MiR-30a promotes TGF-β1-mediated arachnoid fibrosis in posthemorrhagic hydrocephalus. Transl Neurosci. 2020;11(1):60–74. doi:10.1515/tnsci-2020-0010
46. Xiao G, Chen Q, Zhang X. MicroRNA-455-5p/CPEB1 pathway mediates Aβ-related learning and memory deficits in a mouse model of Alzheimer’s disease. Brain Res Bull. 2021;177:282–294. doi:10.1016/j.brainresbull.2021.10.008
47. Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009;65(4):403–413. doi:10.1002/ana.21610
48. Larsson A, Arlig A, Bergh AC, et al. Quantitative SPECT cisternography in normal pressure hydrocephalus. Acta Neurol Scand. 1994;90(3):190–196. doi:10.1111/j.1600-0404.1994.tb02704.x
49. Abdelnour C, van Steenoven I, Londos E, et al. Alzheimer’s disease cerebrospinal fluid biomarkers predict cognitive decline in Lewy body dementia [published correction appears in Mov Disord. 2019 Apr;34(4):593]. Mov Disord. 2016;31(8):1203–1208. doi:10.1002/mds.26668
50. Wenning GK, Jellinger KA. The role of alpha-synuclein and tau in neurodegenerative movement disorders. Curr Opin Neurol. 2005;18(4):357–362. doi:10.1097/01.wco.0000168241.53853.32
51. Parnetti L, Tiraboschi P, Lanari A, et al. Cerebrospinal fluid biomarkers in Parkinson’s disease with dementia and dementia with Lewy bodies. Biol Psychiatry. 2008;64(10):850–855. doi:10.1016/j.biopsych.2008.02.016
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

