Back to Journals » International Journal of Women's Health » Volume 15
A Cohort Study of Mental Health Services Utilization Following a First Pregnancy Abortion or Birth
Authors Studnicki J , Longbons T , Fisher J, Reardon DC, Skop I, Cirucci CA , Harrison DJ, Craver C, Tsulukidze M, Ras Z
Received 17 March 2023
Accepted for publication 26 May 2023
Published 15 June 2023 Volume 2023:15 Pages 955—963
DOI https://doi.org/10.2147/IJWH.S410798
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
James Studnicki,1 Tessa Longbons,1 John Fisher,1 David C Reardon,2 Ingrid Skop,1 Christina A Cirucci,1 Donna J Harrison,3 Christopher Craver,1 Maka Tsulukidze,4 Zbigniew Ras5
1Charlotte Lozier Institute, Arlington, VA, USA; 2Elliot Institute, Springfield, IL, USA; 3American Association of Pro-Life Obstetricians and Gynecologists, Eau Claire, MI, USA; 4Department of Health Sciences, Florida Gulf Coast University, Fort Myers, FL, USA; 5Computer Science Department, University of North Carolina at Charlotte, Charlotte, NC, USA
Correspondence: Tessa Longbons, Charlotte Lozier Institute, 2776 S. Arlington Mill Drive, PO Box 803, Arlington, VA, 22206, USA, Tel +1 202 223 8073, Email [email protected]
Objective: To determine whether exposure to a first pregnancy outcome of induced abortion, compared to a live birth, is associated with an increased risk and likelihood of mental health morbidity.
Materials and methods: Participants were continuously eligible Medicaid beneficiaries age 16 in 1999, and assigned to either of two cohorts based upon the first pregnancy outcome, abortion (n = 1331) or birth (n = 3517), and followed through to 2015. Outcomes were mental health outpatient visits, inpatient hospital admissions, and hospital days of stay. Exposure periods before and after the first pregnancy outcome, a total of 17 years, were determined for each cohort.
Findings: Women with first pregnancy abortions, compared to women with births, had higher risk and likelihood of experiencing all three mental health outcome events in the transition from pre- to post-pregnancy outcome periods: outpatient visits (RR 2.10, CL 2.08– 2.12 and OR 3.36, CL 3.29– 3.42); hospital inpatient admissions (RR 2.75, CL 2.38– 3.18 and OR 5.67, CL 4.39– 7.32); hospital inpatient days of stay (RR 7.38, CL 6.83– 7.97 and OR 19.64, CL 17.70– 21.78). On average, abortion cohort women experienced shorter exposure time before (6.43 versus 7.80 years), and longer exposure time after (10.57 versus 9.20 years) the first pregnancy outcome than birth cohort women. Utilization rates before the first pregnancy outcome, for all three utilization events, were higher for the birth cohort than for the abortion cohort.
Conclusion: A first pregnancy abortion, compared to a birth, is associated with significantly higher subsequent mental health services utilization following the first pregnancy outcome. The risk attributable to abortion is notably higher for inpatient than outpatient mental health services. Higher mental health utilization before the first pregnancy outcome for birth cohort women challenges the explanation that pre-existing mental health history explains mental health problems following abortion, rather than the abortion itself.
Keywords: abortion, mental health, inpatient mental health utilization, outpatient mental health utilization, repeat abortion
Plain Language Summary
The influence of an induced abortion on women’s mental health is a highly contested topic in the literature. In order to address important methodological issues, Dr. Studnicki’s team utilized claims payment data to avoid the limitations of patient surveys; an extended 17-year observation period with long pre- and post-pregnancy outcome periods to address the role of pre-existing mental illness; and, a broad range of mental health conditions applied to both outpatient and inpatient services to provide a comprehensive view of mental health morbidity.
Abortion, compared to live birth, is associated with a higher risk and likelihood of mental health morbidity during the reproductive years. The differences are larger for inpatient treatment than outpatient, and women with first pregnancy births have more, not less, mental health problems before the first pregnancy.
Abortion is associated with a greater incidence of subsequent mental illness than birth, and the difference is not explainable by prior medical history.
Introduction
There is an extensive international research literature which links induced abortion to an elevated risk for a range of mental health problems. A German case-control study by Jacob et al concluded that abortion was positively associated with an increased risk of psychiatric conditions.1 A companion study by Jacob et al compared groups of women with first abortion births and abortions and found abortions to be predictive of depression, adjustment disorder and somatoform disorder.2 Studies from Finland, Italy and China found an increased risk of suicide and suicidal ideation following induced abortion. Gissler et al found a two-fold risk of suicide in spite of new guidelines implemented in Finland to monitor for post-abortion mental health.3 Lega et al studied women in ten Italian regions and found that an abortion was significantly more likely than a live birth to be followed by suicide.4 Luo et al found that unmarried females from three Chinese cities had double the odds of suicidal ideation following abortion, while controlling for numerous demographic, behavioral and attitudinal factors.5 The dose–response relationship for women who have more than a single abortion has also been addressed in terms of mental health consequences. McCarthy et al concluded that women with two prior abortions experienced more perceived stress and depression at 15 weeks gestation than did women with only a single prior abortion.6 A Korean study by Wie et al concluded that women with three abortions experienced an elevated risk for suicidal ideation even while controlling for depression.7 In a US study that extensively controlled for demographic variables and other pregnancy outcomes, Sullins found that induced abortion was associated with an overall elevated risk of mental health problems, and that 8.7% of the prevalence of mental disorders was attributed to abortion.8
Despite these recent persuasive findings, diverging results from previous analyses and important methodological challenges remain. Research into the abortion–mental health connection utilizing survey data has been subject to problems with low response rates, high attrition rates in follow-up data collection, recall bias, uncertainty or lack of precision in defining both the exposure period and outcome indicators, and concealment of past abortions.9–13 Important methodological challenges, however, must also be confronted for records-based research in this domain.
The mental health status of women before the pregnancy outcome (abortion or birth) must be considered. Munk-Olsen et al concluded that women with a first trimester abortion were more likely than women with a first pregnancy childbirth to have subsequent first-time psychiatric contact. However, the pre- to post-abortion psychiatric contact rates were not significantly different, suggesting that abortion may not be a contributing factor to the mental health issue.14 Steinberg et al demonstrated similar findings with first abortions and first non-fatal suicide attempts.15 These findings are congruent with the pattern of other previous research that suggests that women who have abortions may be mentally or emotionally troubled before the abortion itself. This raises the issue of how long the “before” monitoring period should be (Munk-Olsen used only nine months), and whether or not and how the mental health problem is discernable or identified. This problem also suggests that the analysis and study design must consider all women exposed to the risk of a mental health problem, both women who had pre- and/or post-pregnancy outcome mental health problems and those who did not.
Similarly, the design and methodology must consider which pregnancy outcome(s) is considered to be the exposure “agent”. Most of the studies consider a single abortion as the focus of the analysis, usually the first pregnancy outcome. However, mental health threats related to a woman’s reproductive history may occur at any time following the first pregnancy. Absent from the literature, at this point, is any study which characterizes a woman’s entire reproductive history, from first pregnancy to last pregnancy, in terms of its association with mental health issues or disorders.
The range of possible examples of mental health problems or issues and the means by which they can be operationalized or measured are extensive. Just a few examples to illustrate the diversity: depression scores from a questionnaire;16 bipolar disorder and unplanned or interrupted pregnancies;17 past adverse pregnancy outcome (stillbirth, abortion, or a child’s death) associated with depression;18 insomnia, anorexia and severe depression requiring hospitalization following therapeutic abortion;19 clinical psychologist assessment of depression within one week of chemical or surgical abortion;20 alcohol, tranquilizer and other substance abuse related to abortion;21 substance abuse and suicide rates following termination of unwanted versus wanted pregnancies;22 National Comorbidity Survey, history of abortion and substance abuse disorder;23 detoxification center patients and prior abortions;24 history of abortion and smoking and drinking during pregnancy;25 and drug overdose both before and after abortion.26 This very small sample of studies suggests the need for some more comprehensive measure of overall mental health service utilization which can be applied to population denominators. Such an outcome measure(s) applied over an extended period of time would enable a more comprehensive view of the association between pregnancy outcomes and their mental health effects.
In a previous longitudinal cohort study, we followed Medicaid eligible women who were or turned 16 in 1999 for the next 16 years, recording each subsequent pregnancy outcome.27 Women with a first pregnancy ending in abortion were always more likely to have another abortion at every successive pregnancy. Compared to women whose first pregnancy led to a live birth, first pregnancy abortion women had more pregnancies but about half the births and more than four times the number of abortions. Prior research has suggested that women having repeated abortions are at an increased risk of adverse medical and psychological outcomes and an increased risk of death from all causes.28,29 We determined that further post hoc testing of these two cohorts would enable us to address the long-term mental health consequences of having an abortion or birth as the terminus of a first pregnancy. Further, the characteristics of the dataset and research design would enable the study to: utilize confirmed, objective events thus avoiding the many problems inherent in survey research; provide precise measurement of the duration of the exposure to mental health problems before and after the first pregnancy; provide an analysis of the mental health consequences of two vastly different reproductive lifetime experiences, not just a first or index pregnancy outcome event; and utilize a range of specific reasons for treatment that together provide a comprehensive, composite overall view of all mental health morbidity rather than a narrowly defined, single adverse event.
Methods
Data were drawn from the enrollee-level Medicaid Analytic eXtract (MAX) files, which are licensed through the Centers for Medicare and Medicaid Services (CMS) Chronic Condition Data Warehouse (CCW). The total analytic dataset is composed of Medicaid-eligible women who were at least 13 years old with a minimum of one pregnancy from the 17 states where state funding was available for induced abortions not eligible for coverage by federal Medicaid. For this particular analysis, we restricted the study population to those seven states which continually submitted their full Medicaid claims data for all years of the study observation period (1999–2015): Connecticut, New Jersey, New Mexico, New York, Oregon, Vermont, and West Virginia. Additionally, each woman included in the study population was eligible for Medicaid for at least one month in all 17 years of the study period. This ensured that no pregnancies would be missing from the dataset due to non-reporting by the states or gaps in eligibility among women. The study cohorts were created from all women who were or turned 16 years of age in 1999. In a similarly defined population of women who were 15 years old in 1999, less than 0.47% had a pregnancy, allowing high confidence that the women in this study were assigned to cohorts based on the outcome of their first pregnancies. Women were assigned to one of two cohorts dependent upon the first pregnancy outcome: abortion or birth. We identified all unique pregnancy outcomes using International Classification of Diseases, Ninth Revision (ICD9) and Tenth Revision (ICD10) codes. Pregnancy outcomes were confirmed using Current Procedural Terminology, Fourth Edition (CPT4) and Healthcare Common Procedure Coding System (HCPCS) codes.
The following codes were used to group pregnancy outcomes into two categories: live birth (ICD9 V27.0, V27.2, V27.5 and ICD10 Z370, Z372, V375) and induced abortion (ICD9 635.xx, ICD10 O04, CPT4: 59840, 59841, 59850, 59851, 59852, 59855, 59856, 59857, and HCPCS: S0199, S2260, S2265, S2266, S2267, X7724, X7726, S0190, S0191). Multiple codes occurring within 30 days of an induced abortion were collapsed into a single pregnancy outcome based on the first date associated with that cluster of Medicaid claims. Multiple codes within 180 days of a live birth were similarly grouped into a single pregnancy outcome. Twins or higher-order pregnancies that resulted in a combination of live birth and pregnancy loss were not included in this analysis.
We used a comprehensive list of 3-digit ICD9 (ICD9 290–319) and ICD10 (ICD10 F01-F48, F50-F98) codes in order to identify outpatient visits and inpatient hospitalizations that resulted from a range of mental, behavioral, psychiatric or psychological problems, diseases, and disorders.
Our analytic strategy comprised five phases:
- Every Medicaid eligible enrollee was designated to one of the two cohorts based upon the outcome of her first pregnancy: abortion or birth.
- Utilizing the age of each woman at first pregnancy outcome, we determined the average length of the periods of exposure both before (pre) and after (post) the first outcome for each cohort.
- We identified all of the mental health-related events occurring pre- and post-first pregnancy outcome for both the abortion and birth cohorts. The three event categories are the outcome variables: a) outpatient visits; b) inpatient hospital admissions; and c) inpatient hospital days of stay.
- We calculated cohort-specific per patient per year rates for each of the three outcome variables. The rate calculation incorporated the different specific pre- and post-exposure periods previously identified.
- Utilizing event counts for each of the three outcome variables, we constructed contingency tables to enable the determination of the pre-to-post risk (risk ratio) and likelihood (odds ratio) of a mental health event presented by a first pregnancy abortion versus birth. We analyzed both the unadjusted (actual) event counts and a normalized count. The normalized count assumed the rates applied to equal pre- and post-periods of 8.5 years each. The mathematical result of the adjustment for the abortion cohort was to add 32% of events to the pre-period and subtract 20% from the post-period. For the birth cohort, 9% of events were added to the pre-period and 8% of events were subtracted from the post-period.
Summary analytic tables were created using SAS/STAT software, version 10 of the SAS system for Unix, copyright (2019) SAS Institute, Inc. The study has been exempted from Institutional Review Board (IRB) review pursuant to the US Department of Health and Human Services Policy for Protection of Human Research Subjects at C.F.R. 46.101(b). See IRB ID: 7269, www.sterlingirb.com.
Findings
Of 1331 women in the abortion cohort, 475 (35.7%) experienced 14,066 outpatient mental health visits before their first pregnancy outcome and 785 (59.0%) experienced 46,103 visits after. For the abortion cohort, average eligibility exposure time before the first pregnancy outcome was 77.10 months or 6.43 years and average eligibility exposure time after was 126.90 months or 10.57 years. Of the 3517 women in the birth cohort, 1680 (47.8%) experienced 67,682 outpatient mental health visits before their first pregnancy outcome and 2183 (62.1%) experienced 113,578 after. The women in the birth cohort experienced longer pre-first pregnancy outcome eligibility exposure (93.58 months or 7.80 years) and therefore shorter post-pregnancy outcome exposure (110.42 months or 9.20 years) (Table 1).
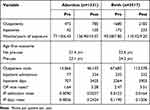 |
Table 1 Data Summary, by Cohort, Pre- and Post-First Pregnancy Outcome |
During their periods of eligibility exposure, 42 (3.2%) abortion cohort women experienced 77 hospital admissions and 707 days of stay before the first pregnancy outcome, and 105 (7.9%) experienced 334 mental health-related hospital admissions and 3425 days of stay following the first outcome. For the birth cohort, 172 (4.9%) women had 335 admissions and 3264 days of stay before their first pregnancy outcome and 233 (6.6%) women had 532 admissions and 3903 days of stay after (Table 1).
Outpatient visits per patient per year for the abortion cohort were 1.64 pre and 3.28 post. For the birth cohort, they were 2.47 pre and 3.51 post. The multiplication of the risk of a pre to post increase in the outpatient visit rate represented by the exposure to abortion rather than birth is RR = 2.10 (2.08–2.12) in the actual data and RR = 1.90 (1.87–1.93) in the data normalized for equal exposure periods. The likelihood of the pre- to post-outpatient visit increase, abortion versus birth exposure, is OR = 3.36 (3.29–3.42) actual and OR 2.35 (2.30–2.40) normalized (Figure 1 and Table 2).
 |
Table 2 Risk and Likelihood of Mental Health Utilization; Pre-to-Post First Pregnancy Outcome; Abortion versus Birth |
 |
Figure 1 Outpatient visits per patient per year. |
Inpatient admissions per patient per year for the abortion cohort were 0.0090 pre and 0.0237 post. For the birth cohort, they were 0.0122 pre and 0.0164 post. The increased relative risk and likelihood of pre-post hospital admission associated with abortion rather than birth as the first pregnancy outcome were as follows: RR = 2.75 (2.38–3.18) in the actual data and RR = 3.05 (2.50–3.71) in the exposure normalized data. OR = 5.67 (4.39–7.32) in the actual data and OR = 4.71 (3.57–6.23) in the normalized data (Figure 2 and Table 2).
 |
Figure 2 Inpatient admissions per patient per year. |
Inpatient days per patient per year for the abortion cohort were 0.0826 pre and 0.2434 post. For the birth cohort, they were 0.1190 pre and 0.1206 post. Relative risk and odds ratios were as follows: RR = 7.38 (6.83–7.97) in the actual data and RR = 75.13 (56.39–100.08) in the normalized data. OR = 19.64 (17.70–21.78) in the actual data and OR = 147.19 (109.70–197.50) in the normalized data (Figure 3 and Table 2).
 |
Figure 3 Inpatient days of stay per patient per year. |
Discussion
Women whose first pregnancy ends in induced abortion are significantly more likely than women whose first pregnancy ends in a live birth to experience mental health problems throughout their reproductive years. Previous research has indicated that a first pregnancy abortion predisposes a woman to experience multiple subsequent abortions and a range of adverse events attendant to them. While we found this relationship for all mental health services, the effect was larger for hospital admissions, and particularly length of hospital stay, than for outpatient services. A plausible interpretation of a stronger association of a history of abortion with inpatient rather than outpatient services is that hospitalization is a proxy measure of the severity of illness and that, therefore, abortion is a stronger influence on the severity of mental illness than it is on the incidence of mental illness. Since our design aggregated all mental health conditions and services into only two categories, outpatient and inpatient, and used the cohort as the unit of analysis, these results are insufficient to inform any conclusions related to the severity of illness. That question would need to be addressed by focusing on a specifically-defined mental illness or condition, using carefully matched subpopulations drawn from each cohort, and utilizing variables that would provide substantive clinical context for each condition.
An important finding is that women who have a birth in their first pregnancy have uniformly higher rates of mental health services utilization prior to that first outcome than women who abort the first pregnancy. Following a first pregnancy abortion, however, women have significantly higher rates of mental health utilization than do women in the birth cohort. For hospital inpatient days, for example, a lower percentage of abortion cohort women than birth cohort women had a psychiatric hospital admission prior to the first pregnancy outcome (3.2% versus 4.9%). The abortion cohort also had about half the inpatient days per woman of the birth cohort in the period prior to the first outcome. However, the pre- to post-outcome utilization increase is significantly greater for the abortion cohort than for the birth cohort: a 4.8-fold increase versus a 1.2-fold increase in inpatient days. The average length of stay for the patients actually admitted from each cohort provides a vivid insight. Prior to the first pregnancy, abortion cohort women admitted to the hospital experienced an average LOS of 16.8 days compared to 19.0 days for the birth cohort. In the post-pregnancy outcome period, the abortion cohort LOS nearly doubled from 16.8 to 32.6. The birth cohort LOS actually decreased from 19.0 to 16.8. Thus, there is a very large risk and likelihood of extended stays for psychiatric admissions following induced abortion.
Women in the birth cohort are, on average, about 14 months older than abortion cohort women at the time of the first outcome. This explains the differences in the exposure time pre–post between the two cohorts. In addition to the differences in the time of exposure for possible health issues, the cohorts differ in the amount of that time during which they are pregnant. For a year of pre-outcome exposure, for example, the birth cohort women will have spent nine months pregnant. Therefore, birth cohort women have a larger exposure time prior to the first outcome but also spend a proportionately greater percentage of that time pregnant. Studies indicate that several psychiatric conditions are commonly experienced by pregnant women, most notably depression and anxiety.30 A number of correlates of antenatal psychiatric morbidity have been identified and, not surprisingly, a history of past illness is frequently mentioned.31
The study population is composed of Medicaid eligible women and, as a result, the findings may not be generalizable to a population with different sociodemographic characteristics. Claims data has other limitations. Services received by beneficiaries but not paid for by Medicaid would not be included in this dataset. Different types of provider delivering a coded service may not be discernible (eg, psychiatrist or psychologist). Certain contextual variables which could be useful for analytical purposes such as marital status, education and religious affiliation are not available. While the use of comprehensive composite indices of mental health services across a 17-year observation period is a strength of the research design, it does not allow conclusions regarding any specific mental health illness, disorder or problem. Similarly, the total cohort as the unit of analysis may mask any number of associations that could be specific to some subpopulation of the cohort; eg, post-pregnancy outcome service utilization for women with and without histories of specific mental illness.
Ethics Approval and Informed Consent
The study has been exempted from Institutional Review Board (IRB) review pursuant to the US Department of Health and Human Services Policy for Protection of Human Research Subjects at C.F.R. 46.101(b). See IRB ID: 7269, www.sterlingirb.com.
Funding
This work was supported by the Charlotte Lozier Institute.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jacob L, Gerhard C, Kostev K, Kalder M. Association between induced abortion, spontaneous abortion, and infertility respectively and the risk of psychiatric disorders in 57,770 women followed in gynecological practices in Germany. J Affect Disord. 2019;251:107–113. doi:10.1016/j.jad.2019.03.060
2. Jacob L, Kostev K, Gerhard C, Kalder M. Relationship between induced abortion and the incidence of depression, anxiety disorder, adjustment disorder, and somatoform disorder in Germany. J Psychiatr Res. 2019;114:75–79. doi:10.1016/j.jpsychires.2019.04.022
3. Gissler M, Karalis E, Ulander VM. Decreased suicide rate after induced abortion, after the Current Care Guidelines in Finland 1987–2012. Scand J Public Health. 2015;43(1):99–101. doi:10.1177/1403494814560844
4. Lega I, Maraschini A, D’Aloja P, et al. Maternal suicide in Italy. Arch Womens Ment Health. 2020;23(2):199–206. doi:10.1007/s00737-019-00977-1
5. Luo M, Jiang X, Wang Y, et al. Association between induced abortion and suicidal ideation among unmarried female migrant workers in three metropolitan cities in China: a cross-sectional study. BMC Public Health. 2018;18(1):625. doi:10.1186/s12889-018-5527-1
6. McCarthy FP, Moss-Morris R, Khashan AS, et al. Previous pregnancy loss has an adverse impact on distress and behaviour in subsequent pregnancy. BJOG. 2015;122(13):1757–1764. doi:10.1111/1471-0528.13233
7. Wie JH, Nam SK, Ko HS, Shin JC, Park IY, Lee Y. The association between abortion experience and postmenopausal suicidal ideation and mental health: results from the 5th Korean National Health and Nutrition Examination Survey (KNHANES V). Taiwan J Obstet Gynecol. 2019;58(1):153–158. doi:10.1016/j.tjog.2018.11.028
8. Sullins DP. Abortion, substance abuse and mental health in early adulthood: thirteen-year longitudinal evidence from the United States. SAGE Open Med. 2016;4:2050312116665997. doi:10.1177/2050312116665997
9. Biggs MA, Neuhaus JM, Foster DG. Mental health diagnoses 3 years after receiving or being denied an abortion in the United States. Am J Public Health. 2015;105(12):2557–2563. doi:10.2105/AJPH.2015.302803
10. Biggs MA, Rowland B, McCulloch CE, Foster DG. Does abortion increase women’s risk for post-traumatic stress? Findings from a prospective longitudinal cohort study. BMJ Open. 2016;6(2):e009698. doi:10.1136/bmjopen-2015-009698
11. Biggs MA, Upadhyay UD, McCulloch CE, Foster DG. Women’s mental health and well-being 5 years after receiving or being denied an abortion: a prospective, longitudinal cohort study. JAMA Psychiatry. 2017;74(2):169–178. doi:10.1001/jamapsychiatry.2016.3478
12. Biggs MA, Upadhyay UD, Steinberg JR, Foster DG. Does abortion reduce self-esteem and life satisfaction? Qual Life Res. 2014;23(9):2505–2513. doi:10.1007/s11136-014-0687-7
13. Foster DG, Steinberg JR, Roberts SC, Neuhaus J, Biggs MA. A comparison of depression and anxiety symptom trajectories between women who had an abortion and women denied one. Psychol Med. 2015;45(10):2073–2082. doi:10.1017/S0033291714003213
14. Munk-Olsen T, Laursen TM, Pedersen CB, Lidegaard Ø, Mortensen PB. Induced first-trimester abortion and risk of mental disorder. N Engl J Med. 2011;364(4):332–339. doi:10.1056/NEJMoa0905882
15. Steinberg JR, Laursen TM, Adler NE, Gasse C, Agerbo E, Munk-Olsen T. The association between first abortion and first-time non-fatal suicide attempt: a longitudinal cohort study of Danish population registries. Lancet Psychiatry. 2019;6(12):1031–1038. doi:10.1016/S2215-0366(19)30400-6
16. Koyun A, Kır Şahin F, Çevrioğlu S, Demirel R, Geçici Ö. Depression following induced abortion. Obstet Gynaecol Reprod Med. 2007;13(2):80–84.
17. Marengo E, Martino DJ, Igoa A, et al. Unplanned pregnancies and reproductive health among women with bipolar disorder. J Affect Disord. 2015;178:201–205. doi:10.1016/j.jad.2015.02.033
18. Ali NS, Azam IS, Ali BS, Tabbusum G, Moin SS. Frequency and associated factors for anxiety and depression in pregnant women: a hospital-based cross-sectional study. Sci World J. 2012;2012:653098. doi:10.1100/2012/653098
19. Spaulding JG, Cavenar JO Jr. Psychoses following therapeutic abortion. Am. J Psychiatry. 1978;135(3):364–365. doi:10.1176/ajp.135.3.364
20. Yilmaz N, Kanat-Pektas M, Kilic S, Gulerman C. Medical or surgical abortion and psychiatric outcomes. J Matern Fetal Neonatal Med. 2010;23(6):541–544. doi:10.3109/14767050903191301
21. Brende JO. Fragmentation of the personality associated with post-abortion trauma. Assoc Interdis Res Values Soc Change Newsletter. 1995;8(3):1–8.
22. Sullins DP. Affective and substance abuse disorders following abortion by pregnancy intention in the United States: a longitudinal cohort study. Medicina. 2019;55(11):741. doi:10.3390/medicina55110741
23. Steinberg JR, Finer LB. Examining the association of abortion history and current mental health: a reanalysis of the National Comorbidity Survey using a common-risk-factors model. Soc Sci Med. 2011;72(1):72–82. doi:10.1016/j.socscimed.2010.10.006
24. Morrissey E, Schuckit M. Stressful life events and alcohol problems among women seen at a detoxication center. J Stud Alcohol. 1978;39:1559–1576. doi:10.15288/jsa.1978.39.1559
25. Kuzma JW, Kissinger DG. Patterns of alcohol and cigarette use in pregnancy. Neurobehav Toxicol Teratol. 1981;3(2):211–221.
26. Houston H, Jacobson L. Overdose and termination of pregnancy: an important association? Br J Gen Pract. 1996;46(413):737–738.
27. Studnicki J, Longbons T, Reardon DC, et al. The enduring association of a first pregnancy abortion with subsequent pregnancy outcomes: a longitudinal cohort study. Health Serv Res Manag Epidemiol. 2022;9:23333928221130942. doi:10.1177/23333928221130942
28. Gissler M, Berg C, Bouvier-Colle MH, Buekens P. Pregnancy-associated mortality after birth, spontaneous abortion, or induced abortion in Finland, 1987–2000. Am J Obstet Gynecol. 2004;190(2):422–427. doi:10.1016/j.ajog.2003.08.044
29. Reardon DC, Thorp JM. Pregnancy associated death in record linkage studies relative to delivery, termination of pregnancy, and natural losses: a systematic review with a narrative synthesis and meta-analysis. SAGE Open Med. 2017;5:2050312117740490. doi:10.1177/2050312117740490
30. Chandra PS. The interface between reproductive health and psychiatry. In: Chandra PS, Herrman H, Fisher J, editors. Contemporary Topics in Women’s Mental Health: Global Perspectives in a Changing Society. United Kingdom: John Wiley & Sons, Ltd; 2009:189–196.
31. Rich-Edwards JW, Kleinman K, Abrams A, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60(3):221–227. doi:10.1136/jech.2005.039370
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
