Back to Journals » Journal of Pain Research » Volume 12
A clinical trial comparing ultrasound-guided ilioinguinal/iliohypogastric nerve block to transversus abdominis plane block for analgesia following open inguinal hernia repair
Authors Faiz SHR , Nader ND , Niknejadi S, Davari-Farid S , Hobika GG , Rahimzadeh P
Received 8 July 2018
Accepted for publication 12 November 2018
Published 4 January 2019 Volume 2019:12 Pages 201—207
DOI https://doi.org/10.2147/JPR.S179506
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Seyed Hamid Reza Faiz,1 Nader D Nader,2 Soraya Niknejadi,1 Sina Davari-Farid,2 Geoffrey G Hobika,2 Poupak Rahimzadeh3
1Department of Anesthesiology, Iran University of Medical Sciences, Tehran, Iran; 2Department of Anesthesiology, University at Buffalo, Buffalo, NY, USA; 3Pain Research Center, Iran University of Medical Sciences, Tehran, Iran
Objective: To compare the efficacy of ilioinguinal/iliohypogastric (IINB) nerve block to transversus abdominis plane (TAP) block in controlling incisional pain after open inguinal hernia repair.
Patients and methods: This was a prospective randomized clinical trial of 90 patients who received either IINB (N=45) or TAP block (N=45) using 0.2% bupivacaine 15 mL under ultrasound (US) guidance based on a random assignment in the postanesthesia care unit after having an open repair of inguinal hernia. Numeric Rating Scale (NRS) scores were recorded immediately following, 4, 8, 12, and 24 hours after completion of the block. NRS scores at rest and during movement were recorded 24, 36, and 48 hours after surgery. Analgesic satisfaction level was also evaluated by a Likert-based patient questionnaire.
Results: NRS scores were lower in the IINB group compared to the TAP block group both at rest and during movement. The difference in dynamic pain scores was statistically significant (P=0.017). In addition, analgesic satisfaction was significantly greater in the IINB group than the TAP block group (mean score 2.43 vs 1.84, P=0.001). Postoperative opioid requirements did not differ between the two groups.
Conclusion: This study demonstrated that compared to TAP block, local blockade of ilioinguinal and iliohypogastric nerves provides better pain control after open repair of inguinal hernia when both blocks were administered under US guidance. Greater satisfaction scores also reflected superior analgesia in patients receiving IINB.
Keywords: US-guided nerve block, transversus abdominis plane, ilioinguinal, iliohypogastric nerve, inguinal hernia surgery
Corrigendum for this paper has been published.
Introduction
The International Association for the Study of Pain defined pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”.1 Postoperative pain is a common complication2 that may cause a neuroendocrine stress response which is characterized by increased release of catabolic and immunosuppressive pituitary hormones and activation of the sympathetic nervous system.3 Excessive postoperative pain and the physiological stress response can influence postoperative outcomes, length of hospital stay, and overall costs of hospital care.4,5
Open repair of inguinal hernia is a common surgical procedure that can be performed under general or regional anesthesia.6 Incisional pain after such an open repair is the most significant factor that determines how soon the patients can return to work after surgery. Postoperative chronic pain, with a prevalence ranging from 6.0% to 54% in various reports, is a significant complication of surgical hernia repair.7,8 This pain has been reported as more frequent in female patients, younger age and higher intensity of the pain in early postoperative period.9 Several analgesic modalities have been used to treat postoperative pain, the mainstay of which is administration of parenteral or oral opioids. However, the systemic use of these analgesic medications is associated with an extensive side effect profile. As a result, there is an ongoing interest in developing regional anesthetic techniques that may reduce or eliminate the use of opioid analgesics after minor surgical procedures such as hernia repair.
Regional analgesia has found wide acceptance both by the patients and their treating physicians, and therefore, it is now an important part of the multimodal analgesia techniques. Paravertebral, rectus sheath, ilioinguinal/iliohypogastric (IINB), and transversus abdominis plane (TAP) blocks have all been used for providing analgesia following abdominal surgeries. From those, IINB and TAP blocks are commonly used to provide both intraoperative anesthesia supplemented with some systemic sedation and meanwhile extend analgesia after the open repair of inguinal hernia.6,10,11 Traditionally, IINB is performed blindly without using ultrasound (US) technology, and in fact most comparisons, which have been made between IINB and TAP blocks, have used US guidance only for the TAP block. IINB blocks have been shown to be more effective when done under US guidance.8 Other reports indicate safety may be greater with US-guided techniques as well (compared to landmark-based techniques). To the best of our knowledge, this is the first randomized clinical trial, which examines the analgesic efficacy of either IINB or TAP block following open repair of inguinal hernia in adults, while both are performed under US guidance. Based on previous reports, we hypothesize that the quality of analgesia attained with either IINB or TAP block is merely equal.
Patients and methods
This was an open-label randomized clinical trial that examined the analgesic efficacy of US-guided IINB or TAP block after open inguinal hernia repairs performed in a in a University Medical Hospital from September 2014 to March 2015. The study was registered with Iranian Registry for Clinical Trials, under (IRCT2014030816888N1, in accordance with requirement by the WHO and the International Committee of Medical Journal Editors’ initiatives (http://www.irct.ir/searchresult.php). The study design, protocol, and the informed consent process were reviewed and approved by the institutional review board of Iran University of Medical Sciences on January 29, 2013, for its scientific merit and ethics in accordance with Declaration of Helsinki.
Inclusion and exclusion criteria
All patients within the age range of 18–70 years old and the American Society of Anesthesiology physical Status 1 through 3 undergoing elective primary open surgical repair of unilateral inguinal hernia were screened and enrolled after they signed an informed consent to participate in the study. Exclusion criteria consisted of inability to consent to the study, body mass index (BMI) ≥40 kg m−2, the presence of skin infection at the puncture site, contraindication to anesthetic drugs, established chronic hepatic failure, chronic kidney disease Stages IV and V (estimated glomerular filtration rate <63ml/min/1.73m−2), and preoperative intake of opioid or non-steroidal anti-inflammatory drugs.
Sample size determination, enrollment, and randomization
The primary outcome variable for this study was the Numeric Rating Scale (NRS) of pain which is an ordinal data ranging from 0 for no pain to 10 for the worst imaginable pain. The clinical significance was set at the differences of >2 in the scale of 11. A mean difference of 2 for NRS scores with an SD of ±3 and alpha error of 0.05 revealed that a minimum of 36 patients in each group were required to produce a power of 80%. After initial screening for inclusion and exclusion criteria, a total of 90 patients (45 in each group) were enrolled in the trial using a factorial design and randomized into two groups using block randomization method based on block of 4 (Figure 1).
Anesthetic techniques and nerve block
All patients were preoperatively educated about anesthesia and postoperative pain management modalities. The process of randomization was explained, and an informed consent was obtained from all patients. All participants received either general or neuraxial anesthesia to have their inguinal hernia surgically repaired. Following completion of the repair, patients were transferred to the postanesthesia care unit (PACU) to recover from general anesthesia. Under US guidance, IINB or TAP block was performed in the PACU based on the randomly assigned grouping.
All patients were continuously monitored with 2-lead electrocardiography, noninvasive arterial pressure, and pulse oximetry throughout the procedure while administered supplemental oxygen (2–3 L/min) via nasal cannula. In both groups, 30 mg (15 cc from 0.2% solution) of plain bupivacaine (Mylan, Chambray Les Tours, France) was used as the local anesthetic agent. For performing the blocks, the patients were placed in the supine position and a sterile prep of the anterior and lateral parts of the abdominal wall was performed with 5% alcoholic povidone-iodine. The blocks were performed under US guidance using MicroMaxx® (SonoSite Inc., Bothell, WA, USA) and a linear HFL38 13–6 MHz probe. For performing the TAP block, the US probe was placed at mid-axillary line in umbilicus level and after identifying three abdominal muscles layers, a sono-opaque 10 cm needle (Vigon Inc., Seoul, South Korea) was introduced with in-plane technique and guided to the potential space between the internal oblique fascia and transvers abdominis muscle followed by injection of the local anesthetic solution. The IINB block was performed by placing the probe between anterior superior iliac spine and umbilicus, and three abdominal muscles layers were visualized and a sono-opaque 10 cm needle was introduced using in-plane technique and guided to internal oblique and transverse abdominis muscle and the local anesthetic mixture was injected. It was not required for the anesthesiologist to visualize the individual ilioinguinal and iliohypogastric nerves when performing the IINB. The hydro-dissection effect was observed confirming a correct placement in both techniques.
A data collection questionnaire was designed and used for this study. The questionnaire contained demographic and background information, as well as the duration of surgery. Postoperative pain was assessed using a 10-point NRS scoring system, recording dynamic and rest pain scores in the PACU, and at 4, 8, 12, and 24 hours after surgery. NRS scores were recorded only at rest in the first 24 hours; however, the later assessments included both rest and dynamic NRS pain scores at 36 and 48 hours after surgery. Supplemental analgesia was provided using intravenous infusions of acetaminophen 1 g every 8 hours in both groups. In patients with NRS pain scores >3 despite acetaminophen, intravenous meperidine 25 mg was also administered. Patients rated their satisfaction with analgesia at the time discharge based on a 5-point Likert scale as follow: (0= weak, 1= moderate, 2= good, 3= very good, and 4= excellent). The patients were evaluated for any additional analgesic need. The results were recorded in a questionnaire.
Sample size determination and power analysis were performed using a publicly available web-based calculator offered by the University British Columbia. The data then entered into Microsoft Excel Worksheet 2016 and transferred to SPSS 24.0 (IBM, Chicago, IL, USA) for analysis and statistical inference. In brief, the categorical data were expressed as the frequency and the percentage and were analyzed using chi-squared test. Numerical variables were analyzed using repeated measures ANOVA and expressed as median with IQR. Numerical data with normal distribution were expressed as mean ± SD and were analyzed with independent t-test for two-group comparisons. Null hypotheses were rejected where P-values were <0.05.
Ethics committee approval
The study design, protocol, and the informed consent process were reviewed and approved by the institutional review board of Iran University of Medical Sciences on January 29, 2013 for its scientific merit and ethics.
Informed consent
All patients signed an informed consent to participate in the study.
Results
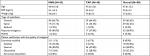
The study population included 90 male patients who were randomized into either study arm. Average age was 47.0±13.2 years old, mean body weight was 77.2±8.3 kg, and height was 1.75±0.05 m. There was no difference in age, BMI, and duration of surgery between two groups (Table 1). Of 90 patients, 59 patients received general anesthesia while 29 had spinal and 2 had epidural anesthesia for the repair of inguinal hernia. It is important to point out that the distribution of the type of operative anesthesia was similar between the two study groups.
Patients in both groups experienced mild-to-moderate pain within the first 24 hours of surgery with a median NRS score of 3 ranging from 2 to 5. The highest level of pain was experienced upon movement at 24-hour time point (NRS scores peaking 6 on a scale of 10). Patients who received IINB block expressed less pain at rest assessed at 4, 8, and 12 hours after the deposition of the block (P=0.013) (Figure 2A). However, the pain scores at rest were similar between the two groups assessed 24 hours after the placement of the block (P=0.141). The patients in the IINB block group also had less pain on movement than the TAP block group up to 48 hours after the nerve block (P=0.017) (Figure 2B).
Total dose of meperidine used to treat break through pain in IINB group was 7.8±10.0 mg which was similar to 7.9±12.1 mg in the TAP block group (P=0.120). Although there was no difference in the dose of parenteral analgesic between IINB group and TAP block group, patients in IINB group requested the first dose of analgesics 2.1 hours later than the patients who received TAP block (P=0.034) (Figure 3).
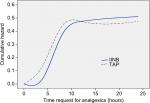  | Figure 3 The probability of request for additional parenteral analgesic drugs is shown at any given time. Abbreviations: IINB, ilioinguinal/iliohypogastric; TAP, transversus abdominis plane. |
A total of 20 patients in IINB group were either satisfied or extremely satisfied with their level of analgesia, while only 6 patients in the TAP group had this level of satisfaction (P=0.002). In addition, the average patient satisfaction score for analgesia in the IINB group was 2.4, which was significantly higher than 1.5 in the TAP block group (P=0.001). No patient from either group experienced nausea or vomiting.
We are willing to share the data for this trial through available data depositories such as Mendeley databank. If there is such a link on the manuscript submission engine, we will be able to upload our deidentified data for sharing.
Discussion
Our data indicate that patients who receive a US-guided IINB have significantly less postoperative pain both at rest and movement and are overall more satisfied than the patients who receive a US-guided TAP block after an open repair of inguinal hernia. In addition, the request for parenteral analgesia to treat the break-through pain is delayed by 2 hours in patients who receive IINB. We also note that more patients in the IINB group (20 patients) report high satisfaction with the quality of their analgesia than the group of patients receiving TAP block (6 patients).
We also demonstrate that the difference in rest pain scores between the two groups gradually decreases after 12 hours until its significance is lost 24 hours after the placement of the block. This observation is in agreement with pharmacokinetic properties of bupivacaine with a reported duration of action approximating 720 minutes.12 However, after 24 hours the group of patients who receive IINB have less dynamic pain (during movement) compared with those following TAP block, and interestingly this difference persists up to 2 days after surgery.
Uncontrolled perioperative pain even in relatively minor surgeries such as inguinal hernia repair may lead to a chronic pain condition and related disability.9,13 Although several studies have compared IINB to TAP block for their effectiveness in alleviating the postoperative pain after inguinal herniorrhaphy, this study is unique in that it is the first to utilize US technology for both IINB and TAP blocks in adult patients. In all previous studies that have been completed in adults, IINB was performed blindly while TAP block was performed under US guidance. Only one study has compared US-guided TAP block to US-guided IINB in children undergoing inguinal hernia repair, and they reported superior pain relief in children who received an IINB compared to those who received a TAP block, which are similar to the results reported herein.14 In a study by Aveline et al, through a comparison between US-guided IINB to blind TAP block, the investigators report a better control of acute pain with IINB technique but no significant difference in the incidence of chronic pain.15 Petersen et al conducted a study on patients undergoing inguinal hernia repair and compared TAP block to ilioinguinal nerve block and to placebo for postoperative pain management. They demonstrated similar analgesic effects with either technique while both are superior to the placebo group.16 It should be noted that these investigators utilized US guidance exclusively for the placement of the TAP block while IINBs were performed blindly by the operating surgeons. It has been shown that US-guided techniques for placement of IINB are superior to the blind technique.8,17 In addition, the same study shows that the use of US guidance not only improves the success of the IINB in relieving the postoperative pain but it also decreases the required volume of the injectate compared to a blind technique.
Sensory innervation of the inguinal region is within the dermatomal distribution of T12 and L1 roots via the cutaneous branch of subcostal nerve, ilioinguinal, iliohypogastric, and genitofemoral nerves.18 The genitofemoral nerve also receives branches from the L2 nerve root. IINB can be done blindly using the landmark technique. In the blind technique, local anesthesia is usually injected 1 inch medial and 1 inch inferior to the anterior superior iliac spine by the anesthesiologist or the surgeon.16–18 US-guided ilioinguinal nerve block is an acute pain management technique in children and adults,19,20 most commonly indicated for inguinal surgery such as inguinal hernia repair. The ilioinguinal nerve originates from anterior ramus of L1 spinal nerve root, travels across the quadratus lumborum muscle and eventually pierces transversus abdominis and internal oblique muscles, and enters the inguinal canal. US-guided ilioinguinal block is a well-established technique. The probe is placed obliquely on the abdomen on a line between anterior superior iliac spine and umbilicus to perform IINB. It has been shown that the use of US increases the rate of success with IINB.17 In addition to lower volume of the local anesthetic injectate required, the time of onset is shorter with the use of US guidance,17 and patients had less static and dynamic pain, greater satisfaction, and a shorter hospital stay.8
From a technical standpoint, TAP block and ilioinguinal nerve block are very similar. TAP block is a commonly used nerve block for operations below the umbilicus and can anesthetize dermatomes from T10 to L1 roots.21 The TAP block is another US-guided nerve block that provides analgesia to the abdominal wall (skin and muscle layers) and parietal peritoneum. This block may have analgesic benefit in various general and gynecological surgeries. To perform a TAP block, the US probe is placed midway between iliac crest and the costal margin along the anterior axillary line and the local anesthetic solution is injected along TAP. Also, it must be kept in mind that performing US-guided IINB requires more skill than TAP block, and in cases of recurrent hernia, an adequate US visualization of this nerve might not be possible. This study utilized the established techniques to perform both US-guided IINB and TAP block uniformly for all participants. Exclusion of the recurrent hernia repairs and limiting the number of the operators to only two anesthesiologists (SHRF and SN) minimized the variation in the skill levels and study results.
It is possible that the superior analgesic quality of IINB is caused by the use of only 15 mL of local anesthetic solution in both IINB and TAP blocks. TAP block is essentially a “field block” of the plane in which the ilioinguinal and iliohypogastric nerves are found, and as such probably requires a higher volume of local anesthetic injectate to reach the intended site of action and surround these nerves. Conversely, in the IINB the injectate is delivered directly in the vicinity of the nerves, thereby requiring a smaller volume of local anesthetic compared to the TAP block, to achieve similar perineural concentrations of local anesthetic. Moreover, using small volumes of local anesthetic drugs is by itself a desirable clinical endpoint.
Limitations
The present study did have a number of limitations. Although the patients were allocated randomly and were blinded as to the type of block they received, the anesthesiologist and the surgery team in charge of the patient were not blinded to the type of the block. In other words, our study is a single-blinded study, which could theoretically introduce an operator bias. Having the block performed by an anesthesiologist who was not involved in the patient pain assessment and management minimized this effect. Moreover, the numeric rating pain scale is not an objective method and there could be some variability in the patients’ ability to use this scale. Another theoretical limitation of our study was the enrollment of only male participants. This was not by study design but more a result of the fact that inguinal hernia pathology is much more common in men than women. An additional study limitation was that the nerve blocks were performed in the postoperative period, after the initial physical injury and, theoretically, central sensitization and “wind up” of the pain stimulus had already occurred. Lack of intraoperative anesthesia and preemptive analgesia might increase the probability of chronic pain after the inguinal surgery. Although this effect was not studied here, we were not aware of any case of chronic pain syndrome among the study participants.
Conclusion
We conclude that US-guided IINB is superior to US-guided TAP block in providing analgesia after inguinal hernia repair in adult patients. In addition, and not surprisingly, patient satisfaction following surgery is dependent on the successful management of pain, and patient satisfaction is most improved by providing adequate analgesia by utilizing a more effective block. The use of continuous block techniques or injection of slow-release encapsulated local anesthetic products needs to be further studied in prolonging the duration of analgesia and decreasing the number of work days lost after inguinal hernia repair.
Acknowledgments
The authors wish to thank Rasoul Akram Hospital Clinical Research Development Center, Iran University of Medical Sciences
Author contributions
SHRF contributed to concept, design, and supervision. SHRF and PR contributed to resources and materials. SN, SHRF, and PR contributed to data collection and/or processing. PR and NDN contributed to analysis and/or interpretation, and literature search; SDF, GGH, and PR wrote the manuscript. GH and NDN contributed to critical review. All authors contributed toward data analysis, drafting and revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surg Clin North Am. 2015;95(2):301–318. | ||
Callesen T. Inguinal hernia repair: anaesthesia, pain and convalescence. Dan Med Bull. 2003;50(3):203–218. | ||
Desborough JP. The stress response to trauma and surgery. Br J Anaesth. 2000;85(1):109–117. | ||
Myles PS, Hunt JO, Fletcher H, et al. Remifentanil, fentanyl, and cardiac surgery: a double-blinded, randomized, controlled trial of costs and outcomes. Anesth Analg. 2002;95(4):805–812. | ||
Faiz SHR, Alebouyeh MR, Derakhshan P, Imani F, Rahimzadeh P, Ghaderi Ashtiani M. Comparison of ultrasound-guided posterior transversus abdominis plane block and lateral transversus abdominis plane block for postoperative pain management in patients undergoing cesarean section: a randomized double-blind clinical trial study. J Pain Res. 2018;11:5–9. | ||
Callesen T, Bech K, Kehlet H. One-thousand consecutive inguinal hernia repairs under unmonitored local anesthesia. Anesth Analg. 2001;93(6):1373–1376. | ||
Kurmann A, Fischer H, Dell-Kuster S, et al. Effect of intraoperative infiltration with local anesthesia on the development of chronic pain after inguinal hernia repair: a randomized, triple-blinded, placebo-controlled trial. Surgery. 2015;157(1):144–154. | ||
Demirci A, Efe EM, Türker G, et al. Bloqueio dos nervos ilio-hipogastrico/ilioinguinal em correcao de hernia inguinal para tratamento da dor no pos-operatorio: comparacao entre a tecnica de marcos anatomicos e a guiada por ultrassom [Iliohypogastric/ilioinguinal nerve block in inguinal hernia repair for postoperative pain management: comparison of the anatomical landmark and ultrasound guided techniques]. Rev Bras Anestesiol. 2014;64(5):350–356. | ||
Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005;95(1):69–76. | ||
Song D, Greilich NB, White PF, Watcha MF, Tongier WK. Recovery profiles and costs of anesthesia for outpatient unilateral inguinal herniorrhaphy. Anesth Analg. 2000;91(4):876–881. | ||
White PF, Kehlet H. Improving postoperative pain management: what are the unresolved issues? Anesthesiology. 2010;112(1):220–225. | ||
Tandoc MN, Fan L, Kolesnikov S, Kruglov A, Nader ND. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene block: a prospective randomized trial. J Anesth. 2011;25(5):704–709. | ||
Callesen T, Bech K, Kehlet H. Prospective study of chronic pain after groin hernia repair. Br J Surg. 1999;86(12):1528–1531. | ||
Fredrickson MJ, Paine C, Hamill J. Improved analgesia with the ilioinguinal block compared to the transversus abdominis plane block after pediatric inguinal surgery: a prospective randomized trial. Paediatr Anaesth. 2010;20(11):1022–1027. | ||
Aveline C, Le Hetet H, Le Roux A, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106(3):380–386. | ||
Petersen PL, Mathiesen O, Stjernholm P, et al. The effect of transversus abdominis plane block or local anaesthetic infiltration in inguinal hernia repair: a randomised clinical trial. Eur J Anaesthesiol. 2013;30(7):415–421. | ||
Khedkar SM, Bhalerao PM, Yemul-Golhar SR, Kelkar KV. Ultrasound-guided ilioinguinal and iliohypogastric nerve block, a comparison with the conventional technique: An observational study. Saudi J Anaesth. 2015;9(3):293–297. | ||
Farag E, Mounir-Soliman L, Brown DL. Brown’s Atlas of Regional Anesthesia. Philadelphia, PA: Elsevier; 2017. | ||
Gray AT. Atlas of Ultrasound-Guided Regional Anesthesia. Philadelphia, PA: Elsevier/Saunders; 2013. | ||
Willschke H, Marhofer P, Bösenberg A, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95(2):226–230. | ||
Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: a cadaveric study. Br J Anaesth. 2009;102(1):123–127. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.