Back to Journals » Clinical Ophthalmology » Volume 16
A Clinical Study of the Impact of Soft Contact Lenses on the Progression of Myopia in Young Patients
Authors Malinowski A, Mrugacz M, Stopa M, Filipek E , Moniuszko-Malinowska A, Czupryna P
Received 7 September 2021
Accepted for publication 12 November 2021
Published 11 January 2022 Volume 2022:16 Pages 51—62
DOI https://doi.org/10.2147/OPTH.S338199
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Andrzej Malinowski,1,* Małgorzata Mrugacz,2,* Marcin Stopa,3 Erita Filipek,4 Anna Moniuszko-Malinowska,5 Piotr Czupryna5
1EliteOptyk Malinowscy, Białystok, Poland; 2Laboratory of Eye Rehabilitation; Medical University of Białystok, Białystok, Poland; 3Department of Ophthalmology, Heliodor Swiecicki University Hospital, Poznan University of Medical Sciences, Poznan, Poland; 4Clinic and Department of Pediatric Ophthalmology, School of Medicine in Katowice, Medical University of Silesia in Katowice, Katowice, Poland; 5Department of Infectious Diseases and Neuroinfections, Medical University of Białystok, Białystok, Poland
*These authors contributed equally to this work
Correspondence: Anna Moniuszko-Malinowska Tel +48-85-740-95-14
Email [email protected]
Purpose: To assess the impact of soft contact lenses on the progression of myopia in young patients.
Patients and Methods: The observational study included 102 patients divided into 3 groups: MFCL (multifocal contact lenses) group: 15 girls and 9 boys, aged 8– 20 (= 14.12 ± 2.863) with soft multifocal contact lenses with myopia: = − 3.12 D ± 1.776 D and mean myopia progression − 0.23 ± 0.233D after 2 years; SVCL (single vision contact lenses) group: 30 girls and 5 boys, 11– 20 years old (=15.5 ± 2.24) with myopia = − 2.88 ± 2.122 D at admission and mean myopia progression − 0.54 ± 0.464 D after 2 years; the spectacle (single vision glasses) group: 25 girls and 18 boys, aged 8– 18 years ( = 13.65 ± 2.448) with single vision glasses with myopia: = − 1.74 ± 1.412 D at admission and mean myopia progression − 0.86 ± 0.489D after 2 years. Medical history and physical examination were performed every 6, 12, 18 and 24 months. Refractive error was examined using the autorefractometry after cycloplegia.
Results: The analysis of myopia correction after 2 years showed differences between MFCL and spectacle correction. The change in myopia progression after 2 years was statistically significant for MFCL vs SVCL and MFCL vs spectacle correction when the myopia occured before the period of intensive growth. When myopia occurred during the period of intensive growth, difference was noted for MFCL vs spectacle correction and SVCL vs spectacle correction. When myopia occurred after a period of intensive growth, no significant differences between the groups were observed.
Conclusion: 1) Multifocal contact lenses and some single vision contact lenses (Biofinity) may be useful in the control of myopia in younger patients, slowing the progression of nearsightedness; therefore, they can be a therapeutic option in inhibiting the progression of myopia. 2) The best effects of using multifocal contact lenses occur if myopia is diagnosed before the period of intensive growth.
Keywords: myopia, multifocal contact lenses, single vision contact lenses, spectacles
Introduction
Myopia (nearsightedness) is a common refractive error in which parallel light rays are focused in front of the retina, causing blurred vision to the distance. It was estimated that in 2010, myopia and high myopia affected 27% (1,893 million) and 2.8% (170 million) of the world’s population, respectively, ie almost 2.1 billion.1 In 2020, the estimated number was 2.5 billion nearsighted people in the world.1
The development of myopia is influenced by optical, environmental and genetic factors.2 According to the literature, myopia is significantly positively associated with higher age, female sex, height, weight, and body mass index, parental myopia, education levels, near work, and spending a long time indoors.3–5
Experimentally induced peripheral hyperopic defocus, which is common in accurately corrected myopia eyes, can exacerbate eyeball growth. On the other hand, myopic defocus, especially when it covers large areas of the retina, may slow down the axial elongation of the eyeball. People with typical myopia have relative hyperopia in the periphery, while people with hyperopia have relative myopia in the periphery.2 Ghosh et al have suggested that the mechanism by which near work increases the axial length is the result of the influence of biomechanical factors, eg ciliary muscle contractions.6 Goss et al and Charman et al observed that working close-up and reading, causing a lag of accommodation (insufficiently strong accommodative response to nearby objects), resulted in focusing these objects behind the retina (hyperopic defocus).7,8 This observation became the basis for the theory that the optical blur caused by delayed accommodation lag may be a signal that contributes to the excessive growth of the eye and causes myopia.
One of the myopia control options are soft multifocal contact lenses, which were originally designed to correct presbyopia. There are two different designs of multifocal contact lenses: the first is a concentric ring system or a bifocal lens and a progressive lens with peripheral additions. Both constructions influence the central and peripheral mapping on the retina. The design of the concentric rings includes alternating distance correction and near zone correction (addition – plus power), providing two focal planes or simultaneous distance correction and myopic retinal defocus. The rationale for this design is to ensure good visual acuity while inducing myopic defocus during fixation at both distances: far and near.9 The progressive lens, on the other hand, thanks to the gradual change in the curvature, ensures distance correction in the central zone with a gradual increase in the addition towards the periphery. This design is made to provide a clear central vision when inducing peripheral myopic defocus when looking at both distances.10–12 Two-year studies in children aged 8–11 demonstrated the effectiveness of Cooper Vision’s Proclear D-Design (Central Correction for Distance) lenses in controlling myopia progression.13 It was noticed that the progression of myopia in the case of single vision contact lenses was: −1.03 ± 0.06 diopters, and in the case of multifocal contact lenses −0.56 ± 0.06 diopters. Similar effects were noted in the axial elongation of the eyeball of 0.41 ± 0.03 mm in the control group compared to 0.29 ± 0.03 mm in the group wearing multifocal lenses. There is therefore a 50% reduction in myopia progression and a 29% reduction in the axial elongation of the eyeball.14 This was also observed in the study of Varnas et al, who performed meta-analyses involving 1662 children and concluded that both multifocal spectacle and contact lenses moderately slow down progression of myopia, relative to single-vision spectacle lenses in the first 12 months after intervention.15 In 2019 FDA approved MiSight MFCL as a method of slowing myopia progression.16
In myopia control, except soft multifocal contact lenses, orthokeratology, DIMS (defocus incorporated multiple segments) spectacle lenses and such pharmacological agents as atropine, pirenzepine and 7-methylxanthine are used.17–21
Younger patients show greater myopia control effects due to the fact that the potential for increased myopia in this age group is greater than in older patients.22 It should be emphasized that axial elongation slows with age and it is more difficult to detect significant differences in the progression of myopia between the groups over a longer follow-up period.
Myopia therapy should be personalized and based on patient and parents family preferences after comprehensively presenting the risks and benefits of each method. One of them is the use of contact lenses, including multifocal lenses.23 Multifocal contact lenses with far power in the central part cause sharp focusing in the middle part of the retina, and at the same time cause extra light myopic defocus. They reduce the growth of the eyeball, and thus inhibit the growth of myopia.24 Compared with traditional methods of correcting myopia (single vision glasses and contact lenses), multifocal soft contact lenses allow myopic patients to maintain sharp vision, further slowing the defect worsening.25
The aim of the study was to assess the influence of soft contact lenses on the progression of myopia in young patients under 20 years old: children and adolescents. Moreover, we aimed to assess the differences in myopia progression when myopia occurred before, during and after the period of intensive growth.
Patients and Methods
One hundred and two patients, who came from the same location (Bialystok, Poland) and were ethnically homogenous, were included in a clinical study. It was an observational study where the patients/parents decided on the type of myopia correction. To prevent investigators from influencing the results, all patients were analyzed by the same specialists in the same time frame and were divided into 3 subgroups from the beginning.
Inclusion Criteria
Myopia of the one or both eyes; age from 8 years to 20 years; astigmatism ≤−1.00 Dcyl; consent of the patient and parent to enter the study.
Exclusion Criteria
Anterior segment diseases of the eye constituting contraindications to the application of contact lenses.
Methodology
A medical history and physical examination were performed in all patients at fixed time points: every 6, 12, 18 and 24 months. Binocularity to check the mean change in two eyes was also included in the analysis. An anterior segment of the eye with a slit lamp and a refractive error were examined, but not axial length. The examination of the refractive error was performed using the objective method – autorefractometry after cycloplegia (Tonoref III (Nidek) autorefractometer). All measures were taken 30 minutes after the last drop instillation (1% cyclopentolate was instilled three times at 10-minute intervals). Best corrected visual acuity (BCVA) was achieved by minimum minus power prescription using the logMAR scale. The values for refraction in the Results were the mean sphere values (sphere + Cyl/2).
All patients were evaluated by the same specialists at all time points.
Depending on the preferences of parents and patients, the myopia was corrected by single vision glasses or with contact lenses: multifocal or monofocal. More often, patients decided on contact lenses, especially multifocal contact lenses when parents, especially mother, had myopia. The patients were under the constant care of an ophthalmologist.
The influence of soft multifocal and single vision contact lenses as well single vision glasses on changes in vision correction depending on the period of intensive growth was analyzed. The study was conducted in accordance with the Declaration of Helsinki.
Questionnaire
All patients and/or parents completed a questionnaire, which included questions about prematurity, coexistence of eye diseases and systemic diseases, and adolescence onset: the first menstruation in girls and mutation in boys, age of intensive growth (year, when a child grew the fastest). The period of intensive growth was determined by patients and parents. The entire group of patients was examined by the same researcher, to minimize the risk of question misunderstanding by patients.
The end of the intensive growth period was determined by patients and parents.
Characteristics of the Groups
Allocation to groups was not randomized. The patients were divided into 3 groups. The number of groups resulted from patients’ and parents’ preferences.
Group I – MFCL (multifocal contact lenses) – 24 children with myopia corrected with soft multifocal contact lenses – Biofinity or Proclear type D. The lenses used in the study had an addition of +2.00 D. This lens has central zone for distance and periphery for near distance – with a progressive addition.
Group II – SVCL (single vision contact lenses) – 35 children with myopia corrected with single vision contact lenses – Biofinity (CooperVision), which stimulate the periphery of the retina by myopic defocus in periphery.
Group III – Spectacle (single vision glasses) – 43 children with myopia with single vision glasses correction.
Further, patients were divided into 3 subgroups: when myopia was detected before the period of intensive growth, when myopia was detected during the period of intensive growth, and when myopia was detected after the period of intensive growth.
Statistical Analysis
The normality was tested with Shapiro–Wilk test. Data were presented as means and standard deviations or medians (interquartile ranges), as appropriate.
Since the data were not normally distributed, Kruskal–Wallis test was used. The differences between the groups were tested with post hoc Dunn’s test. A p < 0.05 was considered significant. The Statistica 13 (StatSoft Polska) software was used.
Results
General Results
Group I - MFCL - 24 children with myopia: Mean= −3.12 D± 1.776 D (binocularly), 15 girls and 9 boys, aged 8–20 ( = 14.12 ± 2.863).
= 14.12 ± 2.863).
Group II- SVCL - 35 children with myopia: Mean= −2.88 D± 2.122 D (binocularly) 30 girls and 5 boys, 11-20 years old ( = 15.54 ± 2.24).
= 15.54 ± 2.24).
Group III - Spectacle - 43 children with myopia: Mean= −1.74 D ± 1.412 D (binocularly), 25 girls and 18 boys, aged 8-18 years ( = 13.65 ± 2.448).
= 13.65 ± 2.448).
The characteristics of the groups are presented in Table 1.
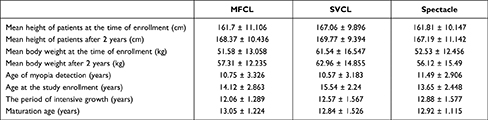 |
Table 1 Characteristics of the Groups: MFCL, CVCL and Spectacle Correction |
The characteristics of the groups/subgroups including children with myopia occurring before (n=54), during (n=33) and after intensive growth (n=15) are presented in Table 2.
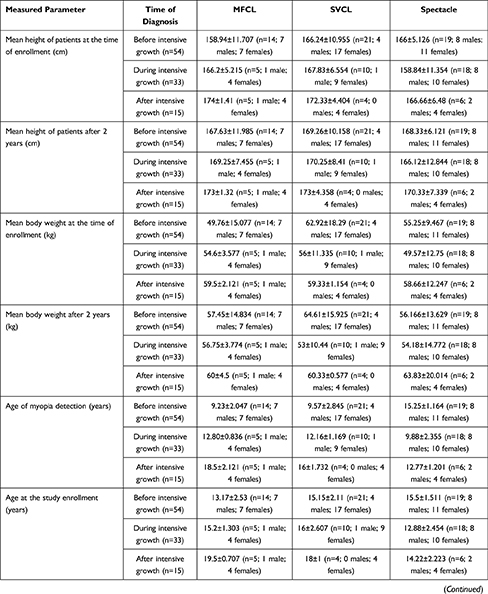 | 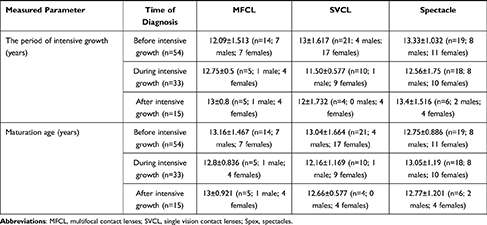 |
Table 2 Characteristics of the Groups: MFCL, CVCL and Spectacle Correction When Divided into Subgroups Depending on Myopia Occurrence: Before, During and After Intensive Growth |
The mean, standard deviation, median, minimum value and maximum value of changes in refraction after 6 months, after one year, after 1.5 years, after 2 years and after 2 years in total are summarized in Table 3.
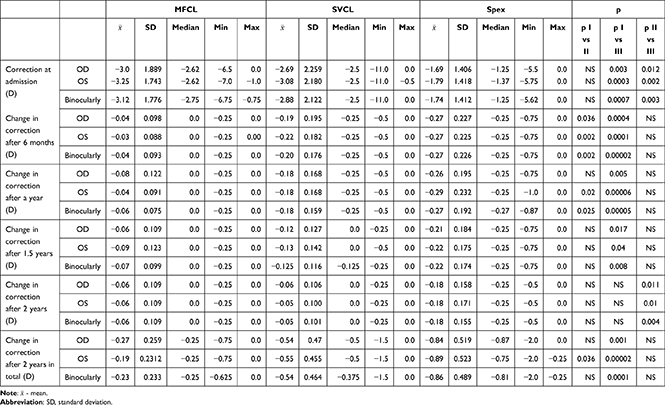 |
Table 3 Mean, Standard Deviation, Median, Minimum and Maximum Value of Correction Changes in Patients from Groups I, II, III |
There was no difference between the groups when the height at the onset of the study was analyzed. There was a difference between the SVCL and Spectacle groups when the weight at the onset of the study was analyzed (SVCL children had higher body mass) and a difference in refractive error at the time of first change in refraction (MFCL (Me=−2.7 D) vs. Spectacle. (Me=−1.25 D)).
Changes in refraction over time for individual patient groups are presented in Figure 1. There were statistically significant differences at the beginning of the study between MFCL and Spectacle as well as SVCL and Spectacle (p < 0.05). Significant differences in refraction were found after 6 months of using both MFCL compared to SVCL, and Spectacle; p <0.05. This relationship was also maintained after one year. After 1.5 and 2 years, a statistically significant change was observed between patients using MFCL and those corrected with glasses. There were no differences between MFCL and SVCL, or MFCL and Spectacle groups. The analysis of myopia progression after 2 years in total showed statistically significant differences between the MFCL group and Spectacle; p <0.05 (Figure 1).
 |
Figure 1 Changes in the myopia refraction after 6 months, 1 year, 1.5 years, 2 years in total – binocularly in MFCL, SVCL and Spectacle correction patients (summed). |
 |
|
 |
Figure 2 Continued. |
Mean BCVA in MFCL patients was 0.93 ± 0.04 (min - 0.8, max - 1), in SVCL patients 0.95 ± 0.36 (min - 0.5, max - 1), and in Spectacle patients 0.96 ± 0.04 (min - 0.8, max - 1). No statistically significant differences were noted between the groups in visual acuity. When multifocal lenses were applied, 13 (54%) of the examined patients reported the impression of overlapping images in the distance immediately after application. Eighteen MFCL patients (75%) required overcorrection (greater minus) to improve visual acuity.
Assessment of the occurrence of adverse events did not reveal any abnormalities in the anterior segment. In addition, a patient satisfaction survey showed satisfaction with the use of multifocal contact lenses, single vision contact lenses and glasses.
Analysis of the influence of soft multifocal and single vision contact lenses as well single vision glasses on changes in refraction over time depending on the period of intensive growth.
The results obtained in the subgroup with the onset of myopia before the period of intensive growth are presented in Figure 2A. A significant difference was found between the effects of the applied changes in correction methods on myopia progression depending on the period of intensive growth. There was a statistically significant differenence in myopia progression between MFCL vs SVCL and MFCL vs Spectacle when the onset of myopia was before the period of intensive growth. Significance was demonstrated after 6 months of the use of multifocal lenses (MFCL) compared to patients from the SVCL and Spectacle groups (p <0.05). The same difference was also observed later in the study - after one and 1.5 years. Changes in refraction after 2 years were statistically significantly different between MFCL vs SVCL and MFCL vs Spectacle (p<0.05).
The results obtained in the subgroup with the onset of myopia during the period of intensive growth are presented in Figure 2B. A statistically significant differenence was demonstrated in myopia progression between MFCL vs Spectacle and SVCL vs Spectacle when the onset of myopia was during the period of intensive growth. There was a significant difference between the effects of the applied changes in refraction on the changes in vision correction after 1.5 years between MFCL and Spectacle, and SVCL and Spectacle (p <0.05). The differences were also maintained after 2 years in total; p <0.05 (Figure 2B).
The results obtained in the subgroup with the onset of myopia after a period of intense growth are presented in Figure 2C. There was a statistically significant difference in myopia progression between MFCL and Spectacle when the onset of myopia was after the period of intensive growth only 6 months after the beginning of the study. There were no statistically significant relationships between the groups at subsequent observation points: after 1 year, after 1.5 years, after 2 years, and after 2 years in total.
Discussion
In the present study, significant differences were observed in inhibiting the progression of myopia in patients wearing multifocal contact lenses compared to patients wearing single vision lenses, although the control of myopia in the group of patients wearing single vision lenses was more effective than in the group of patients corrected with glasses. Significant statistical differences were still present after 2 years of total observation. Also, Holden et al obtained similar results using multifocal lenses. It is assumed that thanks to the lens design (a central far power and peripheral addition), hyperopia in the peripheral part of the retina was reduced, and hence the progression of myopia was diminished.26 An important observation was the occurrence of the best results of multifocal contact lens therapy in the first periods of the study (after the first 6 months and after 1 year), which then translated into final results – after 2 years of follow-up. As myopia progression is slowing down with age, the differences observed in the later stage of the study were smaller than at the beginning of the treatment. The overall mean myopia progression ranges across different age groups with the maximum change in refractive error observed in children aged 6–10 years and at the minimum in adults aged 26–30 years. Early onset of myopia is associated with high myopia in adulthood.27
However, this relationship was not observed in the case of correction with contact lenses and single vision glasses. In the first year of observation, a statistically significant difference was observed in the progression of myopia between the MFCL and SVCL groups and between the MFCL and Spectacle groups in both cases in favor of multifocal contact lenses. In the following year, the difference in the progression of myopia between the groups decreased and was not statistically significant. This may be due to the principle that the increase in myopia stabilizes with the patient’s age. The mean age of the people surveyed after the two-year research period was 16.50 ± 2.59 years. At the same time, after two years in total, statistical significance was demonstrated in slowing the progression of myopia between the MFCL and Spectacle groups, but no statistical significance was found between the SVCL and Spectacle groups or between MFCL and SVCL. Lack of statistical significance between the MFCL and SVCL groups in the later period of the study may be due to the older age of patients in the SVCL group – on average over 1 year compared to patients in the MFCL group. Age difference at the time of entering the study between the MFCL group and the Spectacle group was less than 0.5 year. These observations may indirectly suggest a higher efficiency of correction with multifocal lenses over other correction methods considered in this study.
It is known that younger patients show greater myopia control effects due to the fact that the potential for increased myopia in this age group is greater than in older patients.22 In our study, we analyzed the differences of myopia control depending on the period of myopia onset, which is in accordance with the results of COMET study.22 On the contrary, Li et al proved that younger patients had weaker response to atropine treatment.28
Statistically significant differences between the groups were found in case when myopia onset was before the period of intense growth. Multifocal lenses should be considered in the control of myopia because of the statistically significant difference in the progression of myopia between patients using spectacle correction or single vision contact lenses. Especially that statistical significance was found to occur between patients in the MFCL group vs the SVCL group, but there was no significance in the initial defect. In the case of myopia in adolescence, a difference in the progression of myopia was found between the MFCL and Spectacle groups and between the SVCL and Spectacle groups. Although no significant difference was noted between the MFCL and SVCL groups, the best myopia control effects were observed in the case of multifocal lenses - the median change after two years was 45% lower than in the case of single vision contact lenses. At the same time, there were visible differences in the progression of myopia between patients corrected with SVCL and single vision glasses. The inconclusive results of research conducted by other authors, who assessed the effect of single vision soft contact lenses on the progression of myopia, starting from a negligible negative effect, through no effect, and ending with a positive effect compared to the correction with single vision glasses, probably result from the difference in the design of single vision contact lenses themselves.13 The positive effect of soft contact lenses in myopia progression has been suggested in some worldwide publications.16,29
The construction of spherical soft contact lenses can affect peripheral hyperopia defocusing that is experienced in well-corrected myopic eyes. Some single vision contact lenses reduce peripheral hyperopia. Moore et al showed that among the single vision lenses tested, the strongest peripheral myopic defocusing was caused by Air Optix Night & Day Aqua and Biofinity lenses. In our study, 100% of patients corrected with SVCL used Biofinity lenses, and the statistically significant results of the effectiveness of myopia control confirmed the observations of Moore et al.24
In the case of myopia onset after the period of intensive growth, no differences were found in the progression of this visual defect depending on the correction method. It is related to the spontaneous slowing of myopia progression with age and the well-known observation that the late onset of the defect does not cause significant increases in myopia. The early onset of myopia carries the risk of a rapid progression of the visual impairment and the achievement of high myopia. At the same time, when the decision to introduce correction with contact lenses was made, there was a correlation with family burden – especially in the mother. Parents, having experience related to the progression of their myopia and taking into account the risk of rapid progression of the defect in the child, look for alternative methods of correction another than glasses.
The limitations of our study include a relatively small number of patients in the groups and subgroups (with the division into patients before, during and after intensive growth) and the wide range of patient ages, which caused high variance in data. The patients differed also in initial parameters, such as weight, height and initial refractive error, which may have influenced the obtained results. We collected as many patients as possible over the observation time, but we would like to emphasize that any results identified in this initial study must be confirmed using a large sample set.
Moreover, our patients did not have axial length examination performed. Although accepting that this is a clinical study, the main scientific limitation of the research in addressing the aims, is the method of group allocation by patient preference. We also did not have any possibilities to influence the patients’ and parents’ decision, as it was affected by many factors, such as skills to wear contact lenses. The consequences are that at baseline the groups were not well matched for a number of factors, which may have influenced the outcomes.
Although the results of our study may be useful for clinicians, they should be interpreted with care. Further studies are needed.
Conclusions
- Multifocal contact lenses and single vision contact lenses (Biofinity) may be useful in the control of myopia in younger patients, slowing the progression of the defect; therefore, they can be a therapeutic option in inhibiting the progression of myopia.
- Multifocal contact lenses give better myopia correction results in the first 18 months after application compared to single vision contact lenses, while after 24 months both types of contact lenses give better results than spectacles.
- The best effects of using multifocal contact lenses occur when applied in children in whom myopia was diagnosed before the period of intensive growth.
- Some single vision contact lenses, especially those which reduce peripheral hyperopic defocus, can be useful in myopia control, especially in patients with myopia onset during the period of intensive growth.
Data Sharing Statement
Data supporting reported results can be found in corresponding Author.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent for publication was obtained from participating patients and their parents.
Institutional Review Board Statement
The study received agreement of Bioethical Committee by Medical University of Bialystok, Poland, R-I-002/383/2018.
Implications and Contribution of the Manuscript
Multifocal contact lenses may be useful in the control of myopia in children and adolescents, slowing the progression of the defect; therefore, they can be a therapeutic option in inhibiting the progression of myopia.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors declare no conflict of interest.
References
1. WHO. The impact of myopia and high myopia. Report of the Joint World Health Organization–Brien Holden Vision Institute Global Scientific Meeting on Myopia, University of New South Wales, Sydney, Australia. Vol . 1; 2015:5–8.
2. Mutti DO, Sholtz RI, Friedman NE, Zadnik K. Peripheral refraction and ocular shape in children. Invest Ophthalmol Vis Sci. 2000;41:1022–1030.
3. Ramamurthy D, Lin Chua SY, Saw SM. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Optom. 2015;98(6):497–506.
4. Myrowitz EH. Juvenile myopia progression, risk factors and interventions. Saudi J Ophthalmol. 2012;26(3):293–297.
5. Xie Z, Long Y, Wang J, et al. Prevalence of myopia and associated risk factors among primary students in Chongqing: multilevel modeling. BMC Ophthalmol. 2020;20(1):146.
6. Ghosh A, Collins MJ, Read SA, et al. Axial elongation associated with biomechanical factors during near work. Optom Vis Sci. 2014;91:322–329.
7. Goss DA, Hampton MJ, Wickham MG. Selected review on genetic factors in myopia. J Am Optom Assoc. 1988;59(11):875–884.
8. Charman WN. Near vision, lags of accommodation and myopia. Ophthalmic Physiol. Opt. 1999;19(2):126–133.
9. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152–1161.
10. Kang P, Fan Y, Oh K, et al. The effect of multifocal soft contact lenses on peripheral refraction. Optom Vis Sci. 2013;90:658–666.
11. Berntsen DA, Kramer CE. Peripheral defocus with spherical and multifocal soft contact lenses. Optom Vis Sci. 2013;90:1215–1224.
12. Lopes-Ferreira D, Ribeiro C, Maia R, et al. Peripheral myopization using a dominant design multifocal contact lens. J Optom. 2011;4(1):14–21.
13. González-Méijome JM, Peixoto-de-matos SC, Faria-Ribeiro M, et al. Strategies to regulate myopia progression with contact lenses: a review. Eye Contact Lens. 2016;42(1):24–34.
14. Walline JJ, Greiner KL, McVey ME, et al. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207–1214.
15. Varnas S, Gu X, Metcalfe A. Bayesian meta-analysis of myopia control with multifocal lenses. J Clin Med. 2021;10(4):730.
16. Chamberlain P, Peixoto-de-matos SC, Logan NS, et al. A 3-year randomized clinical trial of misight lenses for myopia control. Optom Vis Sci. 2019;96(8):556–567.
17. Lam CS, Tang WC, Lee PH, et al. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. Br J Ophthalmol. 2021;17:
18. Li Y, Fu Y, Wang K, et al. Evaluating the myopia progression control efficacy of defocus incorporated multiple segments (DIMS) lenses and Apollo progressive addition spectacle lenses (PALs) in 6- to 12-year-old children: study protocol for a prospective, multicenter, randomized controlled trial. Trials. 2020;21(1):279.
19. Kang P, Swarbrick H. New perspective on myopia control with orthokeratology. Optom Vis Sci. 2016;93:497–503.
20. Song YY, Wang H, Wang B, et al. Atropine in ameliorating the progression of myopia in children with mild to moderate myopia: a metaanalysis of controlled clinical trials. J Ocul Pharmacol Ther. 2011;27:361–368.
21. Ganesan P, Wildsoet CF. Pharmaceutical intervention for myopia control. Expert Rev Ophthalmol. 2010;5:759–787.
22. COMET Group. Myopia stabilization and associated. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54(13):7871–7884.
23. Mak CY, Yam JC, Chen LJ, et al. Epidemiology of myopia and prevention of myopia progression in children in East Asia: a review. Hong Kong Med J. 2018;24(6):602–609.
24. Moore KE, Benoit JS, Berntsen DA. Spherical soft contact lens designs and peripheral defocus in myopic eyes. Optometry Vision Sci. 2017;94(3):370–379.
25. Zhu Q, Liu Y, Tighe S, et al. Retardation of myopia progression by multifocal soft contact lenses. Int J Med Sci. 2019;16(2):198–202.
26. Holden BA, Sankaridurg PR, de la Jara PL, et al. Decreasing peripheral hyperopia with distance centre relatively plus powered periphery contact lenses reduced the rate of progress of myopia: a 5 year Vision CRC study. Invest Ophthal Vis Sci. 2012;53:6300.
27. Verkicharla PK, Kammari P, Das AV. Myopia progression varies with age and severity of myopia. PLoS One. 2020;15(11):e0241759.
28. Li FF, Zhang Y, Zhang X, et al. Age effect on treatment responses to 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology. 2021;8:S0161–6420.
29. Kwok E, Patel B, Backhouse S, et al. Peripheral refraction in high myopia with spherical soft contact lenses. Optom Vis Sci. 2012;89:263–270.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

