Back to Journals » International Journal of Women's Health » Volume 14
A Clinical Review on Paroxetine and Emerging Therapies for the Treatment of Vasomotor Symptoms
Authors David PS, Smith TL, Nordhues HC , Kling JM
Received 18 December 2021
Accepted for publication 3 March 2022
Published 10 March 2022 Volume 2022:14 Pages 353—361
DOI https://doi.org/10.2147/IJWH.S282396
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Paru S David,1 Taryn L Smith,2 Hannah C Nordhues,3 Juliana M Kling1
1Department of Internal Medicine, Mayo Clinic, Scottsdale, AZ, USA; 2Department of Internal Medicine, Mayo Clinic, Jacksonville, FL, USA; 3Department of Internal Medicine, Mayo Clinic, Rochester, MN, USA
Correspondence: Paru S David, Email [email protected]
Abstract: Most women experience vasomotor symptoms (VMS) during their menopausal transition. Menopausal hormone therapy (HT) is the most effective treatment for VMS, but some women choose not to use HT or have contraindications to using HT. Non-hormonal treatment options should be offered to these symptomatic menopausal women. Multiple large randomized controlled trials have demonstrated statistically significant reductions in hot flash severity and/or frequency with the use of selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs). To date, paroxetine mesylate remains the only non-hormonal treatment that has been approved by the United States Food and Drug Administration (FDA) for the management of moderate to severe postmenopausal vasomotor symptoms. Lower doses are needed to reduce VMS than those used to treat anxiety or depression, which is beneficial since side effects are typically dose dependent. The recommended dosage is 7.5 mg once daily at bedtime. Dose dependent side effects include nausea, fatigue, and dizziness. Knowing potential medication interactions is critical such as with medications that can lead to serotonin syndrome, concomitant use with monoamine oxidase inhibitors and being aware of p450 drug metabolism is essential for patients taking drugs that utilize the CYP2D6 enzyme for metabolism including tamoxifen. This review discusses in detail the available data supporting the use of paroxetine for the treatment of VMS, including side effects and considerations regarding prescribing. A discussion of other emerging treatments is included as well, including estetrol, oxybutynin and neurokinin 3 (NK3) receptor antagonists.
Keywords: menopause, vasomotor symptoms, non-hormonal treatments, paroxetine
Introduction
Worldwide, approximately 80% of women experience bothersome hot flashes and night sweats, known as vasomotor symptoms (VMS), during the menopause transition and beyond.1,2 The central thermal regulatory neutral zone in the hypothalamus is altered when estradiol levels decline due to menopause.1 Innervation of hypothalamus involves neurons that coexpress kisspeptin, neurokinin B (NKB), and dynorphin known collectively as KNDy neurons.3–6 These KNDy neurons are stimulated by NKB and inhibited by estrogen.3–7 When estrogen levels decline in perimenopause and menopause, there is an increase in NKB signaling which then overstimulates KNDy neurons in the absence of estrogen, thereby increasing activity in the temperature control center, resulting in VMS.3–7 Consequently, this can lead to flushing, sweating and sensation of intense heat in menopausal and perimenopausal women.8 Women may also experience worsening anxiety or depression, irritability and brain fog as a result of the decline in circulating estradiol.8 Bothersome VMS have been shown to adversely impact sleep quality, work productivity, interpersonal relationships and quality of life for many postmenopausal women.9,10 Menopausal hormone therapy is an effective treatment for VMS and is considered to be a safe treatment option in healthy menopausal women when initiated before the age of 60 or within 10 years of menopause.11,12 In addition to managing bothersome menopausal symptoms, hormone therapy (HT) effectively reduces the risk of fractures associated with menopausal bone loss and osteoporosis.11,12 Multiple studies have demonstrated beneficial cardiovascular effects of timely HT use, especially in women who undergo menopause before the age of 45.13
Although HT is considered the standard treatment for managing menopausal symptoms, it is not always the best option for all women. Non-hormonal treatment options should be offered to menopausal women with bothersome VMS who have contraindications or prefer to avoid hormonal therapies. HT should be avoided in women with or at high risk for coronary heart disease, stroke, venous thromboembolism and in women with a history of estrogen dependent cancers.1,8 Multiple large randomized controlled trials (RCTs) have demonstrated statistically significant reductions in hot flash severity and/or frequency with the use of selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) including paroxetine, escitalopram, citalopram, desvenlafaxine and venlafaxine.14–18 SSRIs contribute to VMS management through two proposed mechanisms: lowering core body temperature through central vasodilation to negate the effects that occur during menopause due to the narrowed thermoregulatory zone and by decreasing blood flow to the skin to counter the vasodilation during flushing.19 To date, paroxetine mesylate remains the only non-hormonal treatment that has been approved by the United States Food and Drug Administration (FDA) for the management of moderate to severe postmenopausal vasomotor symptoms.1 This article reviews available data for using paroxetine for the treatment of bothersome menopausal symptoms. In addition, other emerging treatments are reviewed. These emerging therapies include estetrol, oxybutynin and neurokinin 3 (NK3) receptor antagonists.
Overview of Paroxetine for VMS
Paroxetine mesylate 7.5 mg once daily at bedtime was approved by the United States FDA in 2013 solely for the treatment of VMS. While higher doses of paroxetine mesylate and paroxetine hydrochloride are available, they are reserved for the treatment of depression and other psychiatric disorders.10,20 With low dose paroxetine mesylate, improvements were found in VMS frequency and severity up to 6 months along with improvements in sleep disruption attributed to VMS without negative effects on libido or weight gain.21,22 In a position statement put out by the North American Menopause Society (NAMS) on non-hormonal options, paroxetine is considered Level I evidence for the treatment of VMS.10 Paroxetine comes in two forms: paroxetine mesylate and paroxetine hydrochloride. The mesylate and hydrochloride salts are both inactive and disassociate from active paroxetine in the gastrointestinal tract. The differences between the two salts are minor and there is no evidence that the differences have any clinical implications.23 The effect of paroxetine on reducing VMS for severe symptoms is seen as early as 1 week and as early as 2 weeks for moderate VMS symptoms, while the effect on reducing depression is seen at 6 weeks.22,24 Counseling patients on the benefits of early symptom relief of VMS without affecting weight or libido are essential. It also important for clinicians and patients to understand that the low dose is not indicated for the treatment of depression.
Clinical Studies for Use of Paroxetine for VMS
Paroxetine Hydrochloride
Initially, studies were done with paroxetine hydrochloride. Two early pilot studies in 2000 and 2002 were conducted as open-label studies for 6 weeks that showed significant hot flash reduction.25,26 In 2005, Stearns et al conducted a 4 week, double-blind, randomized, controlled, crossover study in 151 menopausal women, with the majority being breast cancer survivors. With 10 mg paroxetine HCl vs placebo, hot flash frequency was decreased by 40.6% vs 13.7% (P=0.0006). Furthermore, hot flash frequency was significantly decreased by 51.7% vs 26.6% (P=0.0002) with 20 mg paroxetine HCl vs placebo. Seventeen (11%) patients withdrew due to adverse effects. Most of the withdrawals were in the 20 mg paroxetine HCl group (n=13), with fewer in the 10 mg paroxetine HCl group (n=4). The most reported adverse effects were drowsiness and nausea.27 Overall, paroxetine HCl was associated with a 40–67% reduction in hot flash frequency with 4–6 weeks of treatment compared to 14–27% reductions with placebo. It was also associated with significant reductions in hot flash severity. The benefits of paroxetine HCl on VMS were observed within 1–2 weeks of therapy and were shown to persist throughout a 6-week treatment duration in this patient population. These trials showed both doses of paroxetine HCl – 10 mg and 20 mg – to be effective for VMS, however the 10 mg dose was better tolerated.28
Paroxetine Mesylate
Following this, 4 RCTs were conducted to assess paroxetine and VMS in women without breast cancer, including two Phase 3 placebo-controlled clinical trials looking at paroxetine mesylate.22 In these 4 trials, paroxetine was associated with a 33–65% reduction in hot flash frequency with 6–12 weeks of treatment compared to 17–38% reductions with placebo. Additionally, paroxetine was also associated with significant reductions in hot flash severity. Patient-perceived improvement was seen at 4 weeks, however patient-perceived improvement did not remain significant at 12 weeks. A 50% reduction in hot flash frequency was observed within 2 weeks of therapy and persisted throughout the 24-week treatment duration (p=0.006).22 In these trials, sleep quality was also evaluated while on paroxetine 7.5 mg daily. Patients reported a mean baseline of 3.6 awakenings per night due to VMS. They found a significant reduction in nighttime awakening from VMS at 4 weeks (39% reduction for paroxetine vs 28% placebo; P=0.0049), and these results were sustained through the 24-week treatment period (62% reduction for paroxetine vs 43% placebo; P, 0.0001). The paroxetine mesylate group also had significantly increased nighttime sleep duration at all assessments, but no differences were found in sleep-onset latency or sleep-related adverse events such as sedation.29 Although most literature supporting use of paroxetine consists of doses between 10 mg and 25 mg, significant reductions in VMS were observed with the low dose of paroxetine mesylate (7.5 mg/day). Additionally, the lower dose had a tolerable adverse effect profile and no significant withdrawal symptoms at discontinuation without tapering.28
Paroxetine Use in Men with Vasomotor Symptoms
Men who undergo androgen ablation therapy for prostate cancer are at risk for VMS, and up to 75% of men will have VMS that affect their quality of life considerably.30 A prospective pilot study was conducted using paroxetine in men experiencing VMS due to androgen ablation therapy for prostate cancer. Patients were evaluated with an initial dose of extended-release paroxetine 12.5 mg daily, escalating to 37.5 mg daily over 5 weeks. Of the 18 patients who completed the study, when compared to baseline, by week 5 study participants had a significant improvement in hot flashes, sweating, trouble sleeping and with quality of life (p<0.05).31 Thus, paroxetine may be effective for men with VMS although the United States FDA indication for the 7.5 mg paroxetine mesylate dose is for vasomotor symptoms of menopause. Additional studies are needed to evaluate the efficacy of paroxetine for vasomotor symptoms in men.
Side Effects
Compared to placebo, the most common side effects reported with paroxetine mesylate were nausea (3.8% vs 1.4%), fatigue (3.4% vs 1.5%), and dizziness (2% vs 0.8%). Reasons that prompted discontinuation that occurred in at least 2% of patients and twice as often compared with placebo included muscle cramps, spasms, and/or twitching (3.4% vs 1.5%); restless leg feeling (2.6% vs 1.2%); and insomnia (2.6% vs 1.2%).22 Although uncommon, there is a black box warning for the potential of paroxetine HCl to increase the risk of suicidal thinking and behavior, however low dose paroxetine mesylate was not tested in women who have a history of depression, suicide attempts, or psychiatric conditions.22 Other adverse effects linked to SSRI use in general include syndrome of inappropriate antidiuretic hormone secretion, bone fractures,32,33 seizures, akathisia, acute angle closure glaucoma, and cognitive and/or motor impairment.34 In the pooled analysis evaluation of the treatment’s effect on weight and sexual dysfunction, there were no statistically significant changes observed from baseline in terms of weight or sexual function in the paroxetine mesylate 7.5 mg group.35
Most adverse effects reported were of mild-to-moderate severity, with improved tolerability associated with lower doses (7.5–12.5 mg/day).28 If lower doses are not effective, dose escalation can be done, however patients may develop side effects necessitating switching to other SSRIs/SNRIs. Suggested dosing for treating VMS include paroxetine mesylate, 7.5 mg per day; paroxetine HCl, 10 to 25 mg per day; escitalopram, 10 to 20 mg per day; citalopram, 10 to 20 mg per day; desvenlafaxine, 100 to 150 mg per day; and venlafaxine, 37.5 to 150 mg per day.10 Additionally, gabapentinoids such as gabapentin 900–2400 mg per day or pregabalin 150–300 mg per day may be used for VMS.10
Contraindications and Inhibition of CYP2D6
Contraindications to SSRIs and SNRIs include serotonin syndrome (consider possible synergy with other medications such as triptans), prior neuroleptic syndrome and concurrent use of monoamine oxidase inhibitors.36 Clinicians should be aware of potential interactions with paroxetine and patients with bipolar disease, uncontrolled seizures, liver or kidney insufficiency, uncontrolled hyponatremia or poorly controlled hypertension, concurrent use of other SSRIs or SNRIs, or relevant polymorphisms in cytochrome P450 enzyme pathways. In women using tamoxifen, concurrent use of SSRIs may lead to inhibition of CYP2D6 (the enzyme that converts tamoxifen to its most active metabolite, endoxifen). The most potent inhibition of CYP2D6 occurs with paroxetine and fluoxetine, so these should be avoided in tamoxifen users. Safer choices include venlafaxine or desvenlafaxine (SNRIs) or escitalopram or citalopram (SSRIs)10 (Table 1).
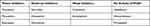 |
Table 1 SSRI/SNRI and CYP2D6 Activity |
An in vivo study of 12 women found that paroxetine decreased the mean serum concentration of the active metabolite endoxifen by 6.9 ng/mL (CI: 2.7–11.2 ng/mL; P=0.004).24,27 A study of 80 newly diagnosed breast cancer patients found that women taking potent CYP2D6 inhibitors, including paroxetine, had levels of endoxifen that were 58% lower (CI: −86.1 to −19.5; P=0.0025).37 Aubert and others conducted a trial of 1298 patients with breast cancer and compared the rate of breast cancer recurrence in patients treated with tamoxifen with or without a CYP2D6 inhibitor. Patients who were receiving a CYP2D6 inhibitor had significantly higher rates of breast cancer recurrence at 2 years, 13.9% vs 7.5%.38 Additionally, a retrospective study found that patients on paroxetine and tamoxifen had a significant increase in risk of death from breast cancer. The study consisted of 2430 women breast cancer survivors who were prescribed an SSRI along with tamoxifen were assessed for all-cause mortality and breast cancer mortality. Women who were prescribed and took paroxetine had increased breast cancer mortality. The risk was further increased based on the amount of overlapped time patients took tamoxifen with paroxetine (overlap percentage of 25% of time caused a 24% increase, 50% overlap generated a 54% increase, and 75% overlap resulted in 91% increase: P<0.05 for all). Based on the results from this study, there would be an additional death from breast cancer for every 19.7 patients who took paroxetine and tamoxifen together 41% of the time (median overlap in this study population). The risk with more extensive overlap would be even greater. This increased risk was not observed among other SSRIs that do not inhibit CYP2D6 in this study.39
It is important to consider this drug interaction because patients with a history of breast cancer who are on tamoxifen tend to report increased rates of VMS (up to 80%) and may rely on certain SSRIs or SNRIs to help with VMS.10,19,24 As a result of this interaction resulting in decreased efficacy of tamoxifen, both the National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology recommend using caution with concomitant use of paroxetine and tamoxifen. The NCCN and International Menopause Society specifically prefer citalopram and venlafaxine over paroxetine and fluoxetine.40
Emerging Uses for Paroxetine
A study published in 2019 showed that paroxetine caused apoptosis of breast cancer cells. Specifically, it mostly reduced the viability of MCF-7 cells in a time-and dose-dependent manner. Paroxetine also showed a synergistic effect on cell death induced by chemotherapeutic drugs in MCF-7 and MDA-MB-231 cells. Paroxetine may serve as an anticancer adjuvant to current cancer therapies for breast cancer patients with or without depression.41 It has been clinically observed that paroxetine has shown cytotoxicity on human tumor cell lines including brain, breast and colon cancers. This is due to kinase pathways involved in tumorigenesis. Studies have established that this is due to the structural similarities including size, shape, and physicochemical properties of paroxetine with many known kinase inhibitors. Consequently, it is not surprising that paroxetine is very compatible with the kinase active site.42 This provides a possibility for a new role for paroxetine in patients with breast cancer. Certainly, consideration needs to be made in those patients with breast cancer on tamoxifen therapy due to CYP2D6 inhibition as previously described.
Discussion of Patient Selection and Relevant Counseling
One must counsel patients on potential side effects that are dose dependent including nausea, fatigue, and dizziness. Bothersome side effects that can lead to discontinuation include muscle cramping, restless leg symptoms and insomnia. Knowing potential medication interactions is critical such as with medications that can lead to serotonin syndrome, concomitant use with monoamine oxidase inhibitors. Lastly, being aware of p450 drug metabolism is essential for patients taking drugs that utilize the CYP2D6 enzyme for metabolism including tamoxifen. Paroxetine can be used in women who do not wish to be on HT or breast cancer patients who are not on tamoxifen.
Due to saturable CYP2D6 metabolism, paroxetine (HCl and mesylate) exhibits nonlinear pharmacokinetics, and therefore dose adjustments can lead to disproportional changes in plasma drug levels.23 Consequently, adverse effects may be observed with dose increases. Although there are no trials directly comparing the 7.5 mg, 10 mg, and 12.5 mg doses, tolerability is comparable based on adverse event rates in similar patient populations. Additionally, there is currently no evidence that doses of 20–25 mg provide significantly greater relief than doses less than or equal to 12.5 mg, and the 25 mg dose was associated with increased frequencies of adverse effects.28 Initiate paroxetine at a low dose and titrate if there is a suboptimal response after 2 weeks.
Emerging Options for Vasomotor Symptom Management
Paroxetine can be an effective alternative to HT for treatment of vasomotor symptoms, but still has some limitations for use. The NAMS 2015 provides additional guidance on other evidence based medications and treatments that could be considered for women with VMS who cannot or choose not to use HT.10 Additionally, the following emerging medications may become acceptable alternatives for VMS treatment. Table 2 summarizes all current and emerging medications for vasomotor symptoms.
 |
Table 2 Comparison of Non-Hormonal Options for Vasomotor Symptoms4,39,41,42,46,57,58 |
Estetrol (E4)
In rodents, the human fetal steroid estetrol (E4) has estrogenic agonist properties in bone, vaginal tissues, endometrium, for temperature regulation and inhibiting ovulation while acting as an estrogen antagonist in breast tumor tissue.43 Early human study evaluating escalating doses of E4 (2, 5, and 10 mg) revealed that E4 appears to be safe when used for VMS, without serious adverse events over an 8-week period.44 However, a multicenter randomized study to evaluate lowest effective dose of E4 for vasomotor symptoms found 15 mg of estetrol as the minimum effective dose, while lower doses failed to reach statistical significance.44 Early studies suggested that estetrol was a weak estrogen; however, advancement of our understanding has shown that E4 has varying pharmacodynamic and metabolic properties as compared to estradiol.43,45 Estetrol has high oral bioavailability, does not enter enterohepatic circulation, and is minimally metabolized giving it a long half-life.46 While traditional forms of estrogen-containing hormone therapy have been associated with thromboembolism and increases in breast cancer E4 is suggested to have an enhanced safety profile.43,45 It does not stimulate sex hormone binding globulin, has less cytochrome inhibition than other synthetic estrogens and therefore, theoretically, has fewer drug interactions and lower venous thromboembolism risk.46,47 While encouraging, further study is needed to identify effective doses and confirm safety and side effect profiles at these doses as well as verify additional estrogenic properties of E4 in post-menopausal women.48
Oxybutynin
Oxybutynin is an anticholinergic, antimuscarinic medication traditionally used for urinary urge incontinence and overactive bladder. Anecdotal evidence suggested that oxybutynin was beneficial for generalized hyperhidrosis49 and for vasomotor symptoms in post-menopausal women taking the medication for overactive bladder.50 One prospective analysis reviewed the safety and effectiveness of oxybutynin for secondary, post-menopausal hyperhidrosis in 21 women using doses of 5 and 10 mg daily.49 A larger, multicenter, randomized, double-blind study of post-menopausal women, with moderate to severe vasomotor symptoms, evaluated doses of 15 mg extended-release oxybutynin versus placebo.50 Women treated with oxybutynin had significant improvements in moderate-to-severe vasomotor symptoms, sleep, and quality of life measures at both 4 and 12 weeks.50 In 2019 a study evaluated lower doses of oxybutynin (2.5 mg or 5 mg twice daily) in a population of women with and without breast cancer in a randomized double-blind placebo-controlled trial.51 These doses were effective at improving hot flashes, sleep, and quality of life and were safe in patients with breast cancer, not on cytotoxic therapy.51 In each of these analyses, oxybutynin was generally well tolerated, the most common side effects were dry mouth and urinary difficulties and appear to be dose dependent.49–51 At higher doses side effects may contribute to discontinuation of the medication limiting its use for some patients.50,51 Additionally, long-term use of anticholinergic medications may be associated with cognitive effects and contribute to medication interactions, especially in elderly patients.52 A recent systematic review of medications used for overactive bladder has shown an association between cognitive decline and oxybutynin use, even in patients without baseline cognitive impairment. Caution should be undertaken if using this medication in older patients.53
Neurokinin 3 (NK3) Receptor Antagonists
Study to further understand the mechanism behind vasomotor hot flashes has implicated neurokinin B (NKB) signaling on the neurokinin 3 receptor (NK3R) in specialized kisspeptin, neurokinin B and dynorphin (KNDy) neurons as a mediator in the hypothalamic-pituitary-gonadal axis and potential target for intervention.4,54,55 In rat models KNDy neurons act on thermoregulatory areas in the brain; activating NK3R reduces rat body temperature and ablation of KNDy neurons reduced cutaneous vasodilation implicated in hot flushes.4 In healthy, post-menopausal women, intravenous infusion of NKB induced hot flashes consistent with their vasomotor symptoms.6 In addition, genetic variation in the gene encoding the NK3R may be able to account for the experienced variability of hot flashes in post-menopausal women.56 A Phase 2, randomized, double-blind, placebo-controlled study evaluated the effectiveness of an oral NK3R antagonist to reduce the number of hot flashes in post-menopausal women.55 A crossover method showed proof-of-concept and overall safety in both groups of participants. Over a four-week treatment period, administration of a twice daily oral NK3R antagonist significantly reduced the number and severity of hot flashes as compared to placebo. It was generally well tolerated but was associated with rise in transaminase concentrations in a subgroup of participants.55 Of the NK3R antagonists currently in clinical development for the treatment of VMS, fezolinetant is the most advanced with several Phase III trials underway.57 A phase IIb trial of fezolinetant, the VESTA trial, showed a significant reduction in VMS frequency and severity when compared to placebo. After 12 weeks, 93% in the fezolinetant group had an improvement of moderate to severe VMS compared to 39% in the placebo group. Similarly, there was a reduction in VMS frequency with a mean of 80.7 weekly episodes at baseline to 5.7 at week 12 in the fezolinetant group compared to reduction of a mean of 72.0 weekly episodes at baseline to 39.0 at week 12 in the placebo group.58
Conclusion
Given that HT is not indicated or preferred by all patients who present with moderate to severe VMS, clinicians need to look to alternatives such as paroxetine. Paroxetine has shown excellent VMS reduction in clinical trials, is considered Level 1 evidence by NAMS as a non-hormonal treatment option for VMS. Choices include the United States FDA approved paroxetine mesylate at 7.5 mg nightly (now available in a generic) or off-label doses of paroxetine hydrochloride 10 −20 mg daily. Since both salts have shown efficacy in clinical trials, initiating therapy with paroxetine HCl 10 mg or 12.5 mg CR may be an option when availability or cost is an issue. Other options beyond paroxetine also exist, as outlined in the NAMS non hormonal management position statement. It is promising that additional non hormonal treatments have also been identified for off label use (oxybutynin) and others are being studied in clinical trials. Ultimately, having many tools available to alleviate bothersome VMS in menopause or other circumstances that lead to VMS improves patient care and outcomes.
Disclosure
Dr Juliana M Kling reports personal fees from Procter and Gamble and Triangle Insights Group, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Pinkerton JV, Santen RJ. Managing vasomotor symptoms in women after cancer. Climacteric. 2019;22(6):544–552. doi:10.1080/13697137.2019.1600501
2. Freeman EW, Sherif K. Prevalence of hot flushes and night sweats around the world: a systematic review. Climacteric. 2007;10(3):197–214. doi:10.1080/13697130601181486
3. Mittelman-Smith MA, Williams H, Krajewski-Hall SJ, McMullen NT, Rance NE. Role for kisspeptin/neurokinin B/dynorphin (KNDy) neurons in cutaneous vasodilatation and the estrogen modulation of body temperature. Proc Natl Acad Sci U S A. 2012;109(48):19846–19851. doi:10.1073/pnas.1211517109
4. Rance NE, Dacks PA, Mittelman-Smith MA, Romanovsky AA, Krajewski-Hall SJ. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: a novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34(3):211–227. doi:10.1016/j.yfrne.2013.07.003
5. Dacks PA, Krajewski SJ, Rance NE. Activation of neurokinin 3 receptors in the median preoptic nucleus decreases core temperature in the rat. Endocrinology. 2011;152(12):4894–4905. doi:10.1210/en.2011-1492
6. Jayasena CN, Comninos AN, Stefanopoulou E, et al. Neurokinin B administration induces hot flushes in women. Sci Rep. 2015;5(1). doi:10.1038/srep08466
7. Rance NE, Young WS. Hypertrophy and increased gene expression of neurons containing neurokinin-b and substance-p messenger ribonucleic acids in the hypothalami of postmenopausal women. Endocrinology. 1991;128(5):2239–2247. doi:10.1210/endo-128-5-2239
8. Mirkin S, Graham S, Revicki DA, Bender RH, Bernick B, Constantine GD. Relationship between vasomotor symptom improvements and quality of life and sleep outcomes in menopausal women treated with oral, combined 17β-estradiol/progesterone. Menopause. 2019. doi:10.1097/GME.0000000000001294
9. Sarrel P, Portman D, Lefebvre P, et al. Incremental direct and indirect costs of untreated vasomotor symptoms. Menopause. 2015;22(3):260–266. doi:10.1097/GME.0000000000000320
10. Carpenter JS. Nonhormonal management of menopause-associated vasomotor symptoms: 2015 NAMS position statement. Menopause. 2016;23(12):1365.
11. Smith T, Sahni S, Thacker HL. Postmenopausal hormone therapy—local and systemic: a pharmacologic perspective. J Clin Pharmacol. 2020;60(S2). doi:10.1002/jcph.1740
12. El Khoudary SR, Aggarwal B, Beckie TM, et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American Heart Association. Circulation. 2020;142(25). doi:10.1161/CIR.0000000000000912
13. Pinkerton JV, Solomon CG. Hormone therapy for postmenopausal women. N Engl J Med. 2020;382(5):446–455. doi:10.1056/nejmcp1714787
14. Stearns V, Beebe KL, Iyengar M, Dube E. Paroxetine controlled release in the treatment of menopausal hot flashes: a randomized controlled trial. J Am Med Assoc. 2003;289(21):2827. doi:10.1001/jama.289.21.2827
15. Freeman EW, Guthrie KA, Caan B, et al. Efficacy of escitalopram for hot flashes in healthy menopausal women: a randomized controlled trial. J Am Med Assoc. 2011;305(3):267. doi:10.1001/jama.2010.2016
16. Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: a randomized controlled trial. Menopause. 2012;19(8):848–855. doi:10.1097/gme.0b013e3182476099
17. Reed SD, Guthrie KA, Joffe H, Shifren JL, Seguin RA, Freeman EW. Sexual function in nondepressed women using escitalopram for vasomotor symptoms: a randomized controlled trial. Obstet Gynecol. 2012;119(3):527–538. doi:10.1097/AOG.0b013e3182475fa4
18. Pinkerton JV, Constantine G, Hwang E, Cheng RFJ. Desvenlafaxine compared with placebo for treatment of menopausal vasomotor symptoms: a 12-week, multicenter, parallel-group, randomized, double-blind, placebo-controlled efficacy trial. Menopause. 2013. doi:10.1097/gme.0b013e31826421a8
19. Archer DF, Sturdee DW, Baber R, et al. Menopausal hot flushes and night sweats: where are we now? Climacteric. 2011;14(5):515–528. doi:10.3109/13697137.2011.608596
20. Paroxetine (Brisdelle) for hot flashes. Med Lett Drugs Ther. 2013;55(1428):85–86.
21. Capriglione S, Plotti F, Montera R, et al. Role of paroxetine in the management of hot flashes in gynecological cancer survivors: results of the first randomized single-center controlled trial. Gynecol Oncol. 2016;143(3):584–588. doi:10.1016/j.ygyno.2016.10.006
22. Simon JA, Portman DJ, Kaunitz AM, et al. Low-dose paroxetine 7.5 mg for menopausal vasomotor symptoms: two randomized controlled trials. Menopause. 2013;20(10):1027–1035. doi:10.1097/GME.0b013e3182a66aa7
23. Cristina Castelli M, Bhaskar S, Lippman J. Pharmacokinetic properties of once-daily oral low-dose mesylate salt of paroxetine (ldmp 7.5 mg) following single and multiple doses in healthy postmenopausal women. Clin Ther. 2013;35(6):862–869. doi:10.1016/j.clinthera.2013.05.001
24. Stearns V, Johnson MD, Rae J, et al. Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst. 2003;95(23):1758–1764. doi:10.1093/jnci/djg108
25. Stearns V, Isaacs C, Rowland J, et al. A pilot trial assessing the efficacy of paroxetine hydrochloride (Paxil®) in controlling hot flashes in breast cancer survivors. Ann Oncol. 2000;11(1):17–22. doi:10.1023/A:1008382706068
26. Weitzner MA, Moncello J, Jacobsen PB, Minton S. A pilot trial of paroxetine for the treatment of hot flashes and associated symptoms in women with breast cancer. J Pain Symptom Manage. 2002;23(4):337–345. doi:10.1016/S0885-3924(02)00379-2
27. Stearns V, Slack R, Greep N, et al. Paroxetine is an effective treatment for hot flashes: results from a prospective randomized clinical trial. J Clin Oncol. 2005;23(28):6919–6930. doi:10.1200/JCO.2005.10.081
28. Carroll DG, Lisenby KM, Carter TL. Critical appraisal of paroxetine for the treatment of vasomotor symptoms. Int J Womens Health. 2015;615. doi:10.2147/IJWH.S50804
29. Pinkerton JV, Joffe H, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Low-dose paroxetine (7.5 mg) improves sleep in women with vasomotor symptoms associated with menopause. Menopause. 2015;22(1):50–58. doi:10.1097/GME.0000000000000311
30. Schow DA, Renfer LG, Rozanski TA, Thompson IM. Prevalence of hot flushes during and after neoadjuvant hormonal therapy for localized prostate cancer. South Med J. 1998;91(9):855–857. doi:10.1097/00007611-199809000-00010
31. Loprinzi CL, Barton DL, Carpenter LA, et al. Pilot evaluation of paroxetine for treating hot flashes in men. Mayo Clin Proc. 2004;79(10):1247–1251. doi:10.4065/79.10.1247
32. Haney EM, Warden SJ, Bliziotes MM. Effects of selective serotonin reuptake inhibitors on bone health in adults: time for recommendations about screening, prevention and management? Bone. 2010;46(1):13–17. doi:10.1016/j.bone.2009.07.083
33. Sheu YH, Lanteigne A, Stürmer T, Pate V, Azrael D, Miller M. SSRI use and risk of fractures among perimenopausal women without mental disorders. Inj Prev. 2015;21(6):397–403. doi:10.1136/injuryprev-2014-041483
34. Carris N, Kutner S, Reilly-Rogers S. New pharmacological therapies for vasomotor symptom management: focus on bazedoxifene/conjugated estrogens and paroxetine mesylate. Ann Pharmacother. 2014;48(10):1343–1349. doi:10.1177/1060028014543099
35. Portman DJ, Kaunitz AM, Kazempour K, Mekonnen H, Bhaskar S, Lippman J. Effects of low-dose paroxetine 7.5 mg on weight and sexual function during treatment of vasomotor symptoms associated with menopause. Menopause. 2014;21(10):1082–1090. doi:10.1097/gme.0000000000000210
36. Shrestha P, Fariba K, Abdijadid S. Paroxetine. In: StatPearls. Tresure Island (FL): StatPearls Publishing;2018.
37. Jin Y, Desta Z, Stearns V, et al. CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst. 2005;97(1):30–39. doi:10.1093/jnci/dji005
38. Aubert RE, Stanek EJ, Yao J, et al. Risk of breast cancer recurrence in women initiating tamoxifen with CYP2D6 inhibitors. J Clin Oncol. 2009;27(15_suppl):CRA508–CRA508. doi:10.1200/jco.2009.27.15_suppl.cra508
39. Kelly CM, Juurlink DN, Gomes T, et al. Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ. 2010;340:c693–c693. doi:10.1136/bmj.c693
40. De Villiers TJ, Pines A, Panay N, et al. Updated 2013 International Menopause Society recommendations on menopausal hormone therapy and preventive strategies for midlife health. Climacteric. 2013;16(3):316–337. doi:10.3109/13697137.2013.795683
41. Cho YW, Kim EJ, Nyiramana MM, et al. Paroxetine induces apoptosis of human breast cancer MCF-7 cells through Ca 2+ -and p38 MAP kinase-dependent ROS generation. Cancers. 2019;11(1):64. doi:10.3390/cancers11010064
42. Kowalska M, Nowaczyk J, Fijałkowski Ł, Nowaczyk A. Paroxetine—overview of the molecular mechanisms of action. Int J Mol Sci. 2021;22(4):1662. doi:10.3390/ijms22041662
43. Coelingh Bennink HJT, Holinka CF, Diczfalusy E. Estetrol review: profile and potential clinical applications. Climacteric. 2008;11(sup1):47–58. doi:10.1080/13697130802073425
44. Coelingh Bennink HJT, Verhoeven C, Zimmerman Y, Visser M, Foidart JM, Gemzell-Danielsson K. Clinical effects of the fetal estrogen estetrol in a multiple-rising-dose study in postmenopausal women. Maturitas. 2016;91:93–100. doi:10.1016/j.maturitas.2016.06.017
45. Reame NK. Estetrol for menopause symptoms: the cinderella of estrogens or just another fairy tale? Menopause. 2020;27(8):841–843. doi:10.1097/GME.0000000000001601
46. Visser M, Foidart JM, Coelingh Bennink HJT. In vitro effects of estetrol on receptor binding, drug targets and human liver cell metabolism. Climacteric. 2008;11(sup1):64–68. doi:10.1080/13697130802050340
47. Hammond GL, Hogeveen KN, Visser M, Coelingh Bennink HJT. Estetrol does not bind sex hormone binding globulin or increase its production by human HepG2 cells. Climacteric. 2008;11(sup1):41–46. doi:10.1080/13697130701851814
48. Gaspard U, Taziaux M, Mawet M, et al. A multicenter, randomized study to select the minimum effective dose of estetrol (E4) in postmenopausal women (E4Relief): part 1. Vasomotor symptoms and overall safety. Menopause. 2020;27(8):848–857. doi:10.1097/GME.0000000000001561
49. Kim WO, Kil HK, Yoon KB, Yoo JH. Treatment of generalized hyperhidrosis with oxybutynin in postmenopausal patients. Acta Derm Venereol. 2010;90(3):291–293. doi:10.2340/00015555-0828
50. Simon JA, Gaines T, LaGuardia KD, et al. Extended-release oxybutynin therapy for vasomotor symptoms in women: a randomized clinical trial. Menopause. 2016;23(11):1214–1221. doi:10.1097/GME.0000000000000773
51. Leon-Ferre RA, Novotny PJ, Wolfe EG, et al. Oxybutynin vs placebo for hot flashes in women with or without breast cancer: a randomized, double-blind clinical trial (ACCRU SC-1603). JNCI Cancer Spectrum. 2020;4(1). doi:10.1093/jncics/pkz088
52. Fick D, Semla T, Beizer J, et al. American geriatrics society updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012. doi:10.1111/j.1532-5415.2012.03923.x
53. Duong V, Iwamoto A, Pennycuff J, Kudish B, Iglesia C. A systematic review of neurocognitive dysfunction with overactive bladder medications. Int Urogynecol J. 2021;32(10):2693–2702. doi:10.1007/s00192-021-04909-5
54. Lehman MN, Coolen LM, Goodman RL. Minireview: kisspeptin/neurokinin B/dynorphin (KNDy) cells of the arcuate nucleus: a central node in the control of gonadotropin-releasing hormone secretion. Endocrinology. 2010;151(8):3479–3489. doi:10.1210/en.2010-0022
55. Prague JK, Roberts RE, Comninos AN, et al. Neurokinin 3 receptor antagonism as a novel treatment for menopausal hot flushes: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10081):1809–1820. doi:10.1016/S0140-6736(17)30823-1
56. Crandall CJ, Manson JE, Hohensee C, et al. Association of genetic variation in the tachykinin receptor 3 locus with hot flashes and night sweats in the women’s health initiative study. Menopause. 2017;24(3):252–261. doi:10.1097/GME.0000000000000763
57. Depypere H, Lademacher C, Siddiqui E, Fraser GL. Fezolinetant in the treatment of vasomotor symptoms associated with menopause. Expert Opin Investig Drugs. 2021;30(7):681–694. doi:10.1080/13543784.2021.1893305
58. Santoro N, Waldbaum A, Lederman S, et al. Effect of the neurokinin 3 receptor antagonist fezolinetant on patient-reported outcomes in postmenopausal women with vasomotor symptoms: results of a randomized, placebo-controlled, double-blind, dose-ranging study (VESTA). Menopause. 2020;27(12):1350–1356. doi:10.1097/GME.0000000000001621
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
