Back to Journals » International Medical Case Reports Journal » Volume 17
A Case Report of Varicella Zoster Virus Infection Progressing to Necrotizing Fasciitis in an Immunocompetent Adult
Authors Ali AM , Bayrak E, Ahmed Mohamud A , Ali ZK
Received 6 June 2023
Accepted for publication 1 February 2024
Published 7 February 2024 Volume 2024:17 Pages 105—109
DOI https://doi.org/10.2147/IMCRJ.S421248
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Ahmed Mohamed Ali,1 Edip Bayrak,1 Abdirahman Ahmed Mohamud,2 Zakaria Kasim Ali2
1Department of Infectious Diseases and Clinical Microbiology, Mogadishu-Somalia Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia; 2Department of General Surgery Mogadishu-Somalia Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia
Correspondence: Ahmed Mohamed Ali, Tel +252615462742, Email [email protected]
Abstract: Adults who have had varicella zoster virus (VZV) infection may experience the unusual consequence of necrotizing fasciitis (NF), which is brought on by a secondary bacterial infection. The optimum approach to treat this medical condition is with a precise diagnosis, quick antibiotic therapy, and immediate surgery. We present 36-year-old case of post chickenpox NF in an immunocompetent male adult patient by diagnosing clinical and laboratory investigations.
Keywords: necrotizing fasciitis, varicella zoster virus, chickenpox
Introduction
Chickenpox is a viral illness that typically causes a mild illness in children, but it can be more severe in adults and in individuals with weakened immune systems. Adults infected with chicken pox account for roughly 47% of cases, with men making up the majority.1 Necrotizing fasciitis is a rare but serious bacterial infection that affects the fascia, the tissue that surrounds muscles, nerves, and blood vessels. It can rapidly spread and lead to tissue death and organ failure.
In rare cases, severe chickenpox can lead to secondary bacterial infections, including to NF. This is more likely to occur in individuals with weakened immune systems, such as those with HIV infection, cancer, or certain medications that suppress the immune system. NF is a rare but potentially fatal skin and soft tissue infection and a surgical and medical emergency.2 Prevention of chickenpox and early treatment of any associated bacterial infections can help reduce the risk of complications such as NF.
Diagnosing of NF is based on clinical and laboratory parameters specially of scoring system which sum total of C-reactive protein (CRP) test, total count, serum sodium, serum creatinine, and blood glucose levels.2 Positive and negative predictive values of 92% and 96%, respectively, are found when the LRINEC score is 6 or more. We present a case of post-chicken pox NF in a Immunocompetent adult male patient.
Case Presentation
A 36-year-old man patient was brought to the emergency room with a high-grade fever, excruciating pain, and an abscess in his right upper thigh. His thigh abscess starts gradually and spreads to posterior and lateral compartment of thigh within three days period. One month ago, he had chicken pox, and his scars are still visible across his body. He has a chronic Hepatitis B illness and no prior vaccination history; he works as a porter. On clinical examination, he was conscious, alert, febrile, dehydrated, generalized post-chicken pox body scars, no jaundice, no sunken eyes, and dry mouth. He was cathetic and skiny, his vital signs Temperature: 40°C, Blood pressure: 111/69 mm Hg, pulse: 149pbm, respiratory rate: 25 breath/min.
There are areas of necrosis from his wound, bad odorous and with discharge involving lateral and posterior thigh as well as deep subcutaneous tissue and skeletal muscle are both affected by the abscess (Figure 1). In the laboratory examinations of patients were provided (Table 1).
 |
Table 1 Laboratory Values |
 |
Figure 1 Lateral and posterior thigh shows necrotic, dead skin and subcutaneous tissues. |
We diagnosed with NF based on his clinical manifestations, abnormal laboratory parameters and Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score (Table 2). Our patients (LRINEC) score is ten score which indicates severe NF. We admitted the patient and immediately began administering antibiotics, analgesics, and fluid resuscitation. Following resuscitation, we administered packed red blood cells (pRBCs). After stabilizing him, we talked to general surgery doctors, who prepared an operating room and made debridement which was cleared abscesses or any dead or black tissues (Figure 2).
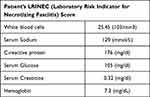 |
Table 2 LRINEC Score |
 |
Figure 2 Post-operative debridement. |
After the surgery, we admitted the patient to the operating room. He was hemodynamically stable and able to take in tiny amounts of liquid. Proteus mirabilis was detected in our abscess culture. We give Intravenous Meropenem 1grm three times a day which was sensitive to Proteus mirabilis was initiated. After three week of treatment and dressing, the patient improved and discharged with polyclinic follow-up.
Discussion
Necrotizing fasciitis is a very rare complication of varicella zoster virus. There are rare reported cases.3 The rapid bacterial spread along the fascial plane that characterizes NF as an infectious disease. It is a rare illness with a yearly incidence of roughly 1.5 cases/100 000 people;3 even the death rate is fairly significant, reaching 20–30%.4,5 There have been two main kinds of NF identified. Type 1 frequently comprises multiple organisms (70–90% of which are group A streptococcus, staphylococcal species, enterococcal species, Enterobacteriaceae, and bacteroides species), whereas type 2 tends to include group A streptococcus (10%).6,7 Diabetes, immunosuppressive medication, chronic infectious illnesses, old age, and other conditions have been recognized as risk factors, particularly for type 1 NF. There are currently no known risk factors for type 2 NF, and even young, healthy patients have been reported to develop streptococci-induced NF. Since there are very few methods for diagnosing obtainable, early detection and prompt treatment are the most crucial factors in determining a patient’s survival.8 It is crucial that patients are presented right away to an authorized surgeon and rushed into surgery at the initial suspicion of NF due to the lack of accurate test criteria and specific symptoms. When patients get surgery within 12 hours of the beginning of their symptoms, the mortality rate is around 6%, but it can increase to 30% after 24 hours.9 Can et al described a case of herpes zoster infection (diagnosed by typical distribution of skin rash), which was exacerbated by NF, difficult to diagnose NF, and correctly identified and treated by LRINEC score.10 We also suspected NF in our patient, who had a blackish skin lesion that was promptly removed for debridement after an early LRINEC score diagnosis. The histology and tissue biopsy results later supported the NF diagnosis.
In our NF which were described above the LRINEC score was 10 durıng admısıon perıod (Table 2). The LRINEC score, which results from the primary blood tests, aids in an earlier diagnosis by distinguishing between NF and cellulitis.
Our case originated in a faraway location approximately 900 kilometers away from us, due to his delayed arrival, his necrotic wounds were severely infected. Fortunately, we were able to quickly respond to the infectious disease Doctors and general surgeons who handled perfectly and discharged the after three week of treatment.
Conclusion
Necrotizing fasciitis is a rare, progressive, medical emergency following VZV infection. Particularly in countries such as Somalia, where access to medical care and childhood immunizations is very limited, complications related to the disease can occur. Complications such as NF, which require rapid diagnosis, surgical management and antibiotic treatment, can cause serious morbidity and mortality in sub-Saharan Africa. In Somalia, cases living in rural areas face serious difficulties in reaching hospitals and receiving medical care. This leads to delayed cases and therefore increased morbidity and mortality.
Ethical Approval
A case report is described in the article. Consequently, no further approval from our Ethics Committee was necessary.
Consent
Patient’s informed written permission was obtained before this report was published.
Limitations
Since PCR and Eliza, which can quickly and accurately identify VZV, are not accessible in our country, we made diagnosis based on clinical and historical data.
Funding
We certify that no institution has provided funding for the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Al‐ Turab M, Chehadeh W. Varicella infection in the Middle East: prevalence, complication and vaccination. J Resp Med Sci. 2018;23:19.
2. Shaikh N, Khwaiter J, Althani H. Necrotizing fasciitis: a surgical and medical emergency. Surg Sci. 2012;3(11):518–525. doi:10.4236/ss.2012.311103
3. Shaikh N, Amara UE, Hussein MI, et al. Varicella zoster viral infection complicating into necrotizing fasciitis: a case report. Clin Case Rep. 2022;10(10):e6408. doi:10.1002/ccr3.6408
4. Davies HD, McGeer A, Schwartz B, et al. Invasive group A streptococcal infections in Ontario, Canada. Ontario Group A Streptococcal Study Group. N Engl J Med. 1996;335(8):547–554. doi:10.1056/NEJM199608223350803
5. Angoules AG, Kontakis G, Drakoulakis E, et al. Necrotising fasciitis of upper and lower limb: a systematic review. Injury. 2007;38(Suppl 5):S19–S26. doi:10.1016/j.injury.2007.10.030
6. Giuliano A, Lewis F, Hadley K, et al. Bacteriology of necrotizing fasciitis. Am J Surg. 1977;134(1):52–57. doi:10.1016/0002-9610(77)90283-5
7. Elliott D, Kufera JA, Myers RA. The microbiology of necrotizing soft tissue infections. Am J Surg. 2000;179(5):361–366. doi:10.1016/S0002-9610(00)00360-3
8. McHenry CR, Piotrowski JJ, Petrinic D, et al. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995;221(5):558–63; discussion 63–5. doi:10.1097/00000658-199505000-00013
9. Wong CH, Chang HC, Pasupathy S, et al. Necrotizing fasciitis: clinical presentation, microbiology and determinants of mortality. J Bone Joint Surg Am. 2003;85-A(8):1454–1460. doi:10.2106/00004623-200308000-00005
10. Can B, Gözel B. Necrotizing fasciitis after herpes zoster infection: a rare case with diagnostic difficulties. Cureus. 2022;14(5):e24805. doi:10.7759/cureus.24805
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
