Back to Journals » International Journal of Women's Health » Volume 15
A Case Report of Retroperitoneal Ectopic Pregnancy After in vitro Fertilization-Embryo Transfer and Literature Review
Received 4 March 2023
Accepted for publication 27 April 2023
Published 4 May 2023 Volume 2023:15 Pages 679—693
DOI https://doi.org/10.2147/IJWH.S408319
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Marleen van Gelder
Zesi Liu,1 Chunli Jing2
1Department of Gynecology and Obstetrics, The First Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China; 2Department of Ultrasound of Gynecology and Obstetrics, The Second Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China
Correspondence: Chunli Jing, Department of Ultrasound of Gynecology and Obstetrics, The Second Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China, Tel +86-133-522-31070, Fax +86-82866055, Email [email protected]
Background: Retroperitoneal ectopic pregnancy (REP) is an extremely rare type of ectopic pregnancy that can be life threatening. The pathogenesis of REP remains inconclusive and the diagnosis and treatment modalities are unclear.
Case Presentation and Review of the Literature: A 27-year-old woman (gravida: 3; parturition: 0) underwent transvaginal ultrasound (TVS) 40 days after in vitro fertilization-embryo transfer (IVF-ET); no intrauterine gestational sac was detected. The patient was asymptomatic and had no abnormalities on physical examination. β-HCG and progesterone were 18.210 mIU/mL and 10.891 ng/mL, respectively. Transabdominal ultrasound (TAS) showed that the gestational sac had implanted adjacent to the abdominal aorta and near a branch of the iliac artery. Laparoscopic exploration was performed under general anesthesia; intraoperative findings showed that the gestational sac was approximately 2.5 cm in diameter and in the same location as suggested by preoperative ultrasound. Histopathological examination confirmed the diagnosis of EP. On day three post-surgery, the levels of β-HCG had fallen to 911 mIU/mL. We further systematically reviewed the REP cases reported in the English literature and performed a review on the diagnosis and treatment of REP.
Conclusion: Clinicians should be alert to the occurrence of REP. Combined radiological examinations including ultrasonography (TAS and TVS), CT, and MRI are essential for the early diagnosis of REP. Once a definitive diagnosis is made, appropriate treatment should be administered immediately. Although there are cases of successful drug treatment described in the literature, surgery remains as the primary treatment option for REP.
Keywords: retroperitoneal ectopic pregnancy, ultrasound, surgery, diagnosis, review
Introduction
With recent advances in ultrasound diagnostic technology and the popularity of β-HCG testing, the rate of misdiagnosis and the mortality of ectopic pregnancy (EP) have decreased steadily.1 However, EP remains the leading cause of death among women with early pregnancy, accounting for approximately 9% of all pregnancy-related deaths.2,3 Retroperitoneal ectopic pregnancy (REP) is an extremely rare type of EP in which the embryo implants into the retroperitoneal space.4,5 By searching PubMed, we found that only 35 cases of REP have been published since Hall et al reported the very first case of REP in 1973. Due to its bizarre implantation site, variable clinical features and extremely low incidence, the misdiagnosis rate of REP is extremely high, and the mortality rate is approximately seven-fold higher than the common type of EP.6 There is no treatment guideline for REP. Therefore, in order to provide clinicians with more clues about the diagnosis and treatment of REP, we report a case of REP implanted adjacent to the abdominal aorta and near the branch of the iliac artery and conducted a review on all cases reported in the English literature.
Case Presentation
The case was a 27-year-old female, a gravida 3 para 0, with regular menstruation, moderate volume, and no dysmenorrhea. She had undergone salpingectomy for an ectopic pregnancy 3 years and 6 years previously. On this occasion, in vitro fertilization-embryo transfer (IVF-ET) had been performed at Dalian Maternal and Child Health Hospital, Dalian Medical University, and two embryos had been transferred into the uterus. After 40 days, the levels of β-HCG and progesterone were 18,210 IU/L and 10.891 ng/mL, respectively, and ultrasound was performed to assess embryonic development. Transvaginal ultrasonography (TVS) showed that the endometrium was approximately 1.6 cm thick but no gestational sac was found in the uterine cavity, bilateral uterine horns, or bilateral adnexal areas (Figure 1A and B). There was a right ovarian echo loss approximately 1.6 cm × 1.2 cm × 1.4 cm in size with a ring blood-flow signal. The left ovary was normal. No free liquid dark areas were seen in the pelvic abdomen. A transabdominal ultrasound (TAS) was performed and the scan was expanded. A gestational sac-like echo was seen 2 cm to the right of the umbilical orifice immediately anterior to the right of the abdominal aorta (near the branch of the iliac artery), measuring approximately 2.2 cm × 1.9 cm × 1.6 cm; a yolk sac and fetal buds were clearly visible (Figure 1C). The heart rate was 155 beats/min (Figure 1D).
We then performed a physical examination; vital signs were stable and no abnormalities were found during cardiopulmonary auscultation; there was no tenderness or pain, rebound pain or muscle tension in the entire abdomen, no vaginal bleeding and no sensation of anal swelling. To further clarify the diagnosis and treatment, laparoscopic exploration was performed under general anesthesia. Intraoperatively, the uterus was seen to be slightly larger in size and there was a corpus luteum approximately 1.5 cm in diameter in the right ovary without rupture or bleeding. We observed adhesion of the left ovary to the left pelvic wall, the presence of the isthmus of the right fallopian tube and attachment to the surface of the broad ligament, with the rest of the tube absent. The left fallopian tube was completely absent. No significant free fluid was seen in the pelvis, and careful exploration of the broad ligament, omentum, intestinal canal, and mesenteric surface did not reveal any embryonic tissue (Figure 2A). Next, we performed intraoperative real-time TAS; this showed a gestational sac next to the abdominal aorta with the same location and internal echogenicity as the preoperative ultrasound. The surgeon pushed open the intestinal canal and the greater omentum, revealing a smooth posterior peritoneal surface and purple-blue staining next to the abdominal aorta. The operator also prepared plasma and red blood cells and asked the vascular surgeon to consult and assist in the exploration because of the risks associated with the operation, including the risk of hemorrhagic shock if the vessel ruptured. The retroperitoneal space and arterial vascular sheath were opened, and an ultrasonic knife was used to separate the fat on the surface of the parietal aorta and inferior vena cava and small vascular branches layer-by-layer; the gestational lesion was then freed (Figure 2B); its diameter was approximately 2.5 cm (Figure 2C). Based on the postoperative histopathological results, villi tissue was observed in the retroperitoneal mass. Three days after surgery, the levels of β-HCG had decreased to 911 IUL. The patient had recovered well when checked after 3 months of follow-up.
Clinical Characteristics
By searching the literature, we identified a total of 35 patients (Table 1) with REP and their clinical information are summarized in Table 2. The mean age was 30.51 years with the standard deviation is 4.19. Almost half of the patients had a history of tubal pregnancy and underwent salpingectomy (15/35, 42.8%). Notably, of the REP patients who underwent only unilateral tubal resection, the proportion of right-sided tubal EP was extremely high (8/10 vs 2/10). A total of 12 patients underwent IVF; most of these had two or more embryos transplanted (11/12, 91.6%). Those findings indicated that IVF-ET and right tubal ectopic pregnancies may be the risk factor for REP. The duration of amenorrhea and β-HCG values in REP patients spanned a wide range, from 35 to 161 d (mean: 55.8 d) and from 267 to 99,286 IU/L (mean: 31,192.5 IU/L), respectively. This difference in β-HCG values may be related to the site of embryo implantation. For example, Meire et al reported an embryo that had implanted in the retroperitoneal paravesical space on the right pelvic cavity; this seemed to provide more space for embryo development compared to other sites.7 The clinical presentation of REP lacks specificity when compared to the common type of EP; A significant proportion of patients, including the present case, did not show any significant clinical symptoms (9/35, 25.7%). Abdominal pain was more frequent in patients with REP (20/35, 57.1%), while some other common clinical manifestations of EP, such as vaginal bleeding (7/35, 20.0%), were less frequent. Therefore, although REP is an extremely rare type of EP, clinicians need to be alert for the occurrence of REP when patients with elevated β-HCG and no intrauterine and adnexal region gestational sac and present with some non-specific clinical manifestations such as flank pain (4/35, 11.4%) and back pain (2/35, 5.7%).
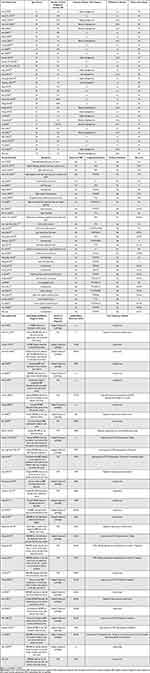 |
Table 1 Clinical Information of All Patients with Retroperitoneal Ectopic Pregnancy in the English Literature |
 |
Table 2 Summary of All Cases with Retroperitoneal Ectopic Pregnancy (n=35) |
Pathogenesis
The exact pathogenesis of REP is not known, although four hypotheses have been proposed in previous literature. First, lymphoid tissue was found in the postoperative pathology of many cases; this appears to suggest that the embryo may have been implanted in the retroperitoneal space through lymphatic tracts as in the case of gynecological endometrial cancer lymphatic metastases.8–11 It is noteworthy that the embryonic implantation sites in REP patients were not randomly distributed in the vast retroperitoneal space but mostly concentrated in the place adjacent to major vessels with abundant lymphatic vessels (19/35, 54.3%), such as the abdominal aorta (17/19), inferior vena cava (8/19), iliac artery (4/19), and renal vein (3/19). In addition, to avoid implantation failure, fertilized embryos are often placed deep within the cavity of uterine during ART implantation, thus increasing the likelihood of lymphatic metastasis.12 Second, we found that more than 50% of REP patients with history of fallopian tube surgery, if a fistula forms between the tubal stump and the retroperitoneal space after salpingectomy, may result in direct communication between the uterine cavity and the retroperitoneum, thus making the spontaneous transfer of embryos from the uterine cavity to the retroperitoneum possible.13 However, in this case, we found that although the right fallopian tube isthmus was present but attached to the surface of the broad ligament, the left fallopian tube was completely absent and no traces of fistula were found intraoperatively. In addition, 17 REP patients were without a history of tubal surgery; this is inconsistent with the hypothesis described above. Third, the prevalence of EP has been reported to be significantly higher in women who underwent assisted reproductive technology (ART) than in the general population; of a cohort of REP patients, we found that a high proportion (34.3%; 12/35) had undergone ART. During implantation, the embryo may implant in the retroperitoneal space due to iatrogenic factors. However, this hypothesis is less likely considering that IVF-ET is performed under ultrasound guidance.14–16 In addition, this hypothesis does not apply to REP patients who conceive naturally. Finally, for all REP patients, the embryo may be initially implanted on the peritoneal surface and reach the retroperitoneal space via invasion of the trophoblast cells.14 In summary, we believe that there may be multiple pathogenic mechanisms associated with REP and the exact pathogenesis of REP is still worthy of further research. Clinicians should individualize the specific pathogenic mechanism in the context of the patient’s specific situation.
Diagnosis
REP has a very high rate of misdiagnosis (22/35, 62.9%) due to its extremely low incidence, variable clinical symptoms, and specific location of the lesion. Fortunately, the rate of REP misdiagnosis has decreased significantly since 2010 (10/13, 76.9% vs 12/22, 54.5%). Ultrasound plays an important role in the diagnosis of REP as a simple and efficient diagnostic tool that allows better visualization of the yolk sac and fetal heart when compared to CT and MRI, especially before emergency surgery.13 The definitive diagnosis was made by ultrasound in 13 patients (12 by TAS and 1 by TVS). Compared to TVS, TAS ultrasound provides a broader sweep to detect REPs in the mid or upper abdomen and real-time intraoperative TAS guidance allows for the immediate determination of gestational sac location and reduces surgical risk. However, there were still some REPs (10/35, 28.6%) that were misdiagnosed when only ultrasound was performed. CT or MRI can be performed as supplemental approaches before treatment to further clarify the diagnosis, determine the relationship between the location of the gestational sac and the peritoneum and assess the relationship between the gestational sac and the adjacent organs. Above all, we believed that ultrasound combined with CT and MRI can increase diagnostic accuracy of REP, provided that the vital signs of the patient with suspected REP are stable and the risk of gestational sac rupture is excluded. In addition, although there is no significant difference in β-HCG values in REP patients compared to other types of EP patients, dynamic monitoring of β-HCG values is still a useful tool for diagnostic and postoperative assessment of prognosis. For example, a decrease in β-HCG values to zero after treatment suggests an effective treatment.
Treatment
By searching the literature, the prognosis of REP is extremely poor, and no case reports of successful delivery in REP patients have been found. Laparoscopy has become the main treatment option for REP because it is associated with a low injury rate, reduced bleeding, and had a quick postoperative recovery; a total of 10 cases have been treated with laparoscopy alone. However, in patients with REP, blastocysts are often localized near large blood vessels and vital organs. Although most cases only show adhesion to blood vessels or organ surfaces rather than infiltration into blood vessel walls or organic tissue, in the case of intraoperative blastocyst or vessel wall rupture, it can be difficult to stop bleeding during laparoscopy; this can lead to deterioration of the disease and even shock and death. In a previous study, Hou et al concluded that laparotomy was safer than laparoscopy and more appropriate for REP patients in shock or suffering from blastocyst rupture.17 We suggest that patients with REP should be evaluated by diagnostic laparoscopy to assess the disease and surgical risk and select further treatments according to the specific situation, such as whether to choose laparoscopic or exploratory dissection treatment. In addition, operator experience, accurate preoperative evaluation, thorough preoperative preparation, and multidisciplinary consultations, including anesthesiology, vascular surgery, and gastrointestinal surgery, can have a significant impact on surgical risk and patient prognosis.
Of the REP patients reported, a total of 11 cases were treated with methotrexate (MTX). Since MTX can reduce embryonic activity, it has been suggested that the combination of surgery and MTX might reduce intraoperative bleeding and decrease the length of hospital stay, especially in patients with suspected preoperative vascular or organ invasion.18 In a previous study, six cases were treated with MTX and underwent surgical removal of an extraperitoneal gestational sac due to treatment failure. Xu et al suggested that this may be related to higher β-HCG levels, more advanced gestations, and the presence of an ectopic viable embryo.12 In addition, we found that five out of six blastocysts were localized near major blood vessels. In this regard, we speculate that the reason for the failure of drug therapy may be related to an insufficient drug concentration at the site of the lesion. Huang et al successfully applied a CT-guided local injection of MTX for two REP patients (pre-treatment β-HCG:92079IU/L and 97,333.01 IU/L, respectively), thus supporting this hypothesis.5 Although it took longer for the levels of β-HCG to drop to normal after treatment, this result indicated that the image-guided local injection of MTX may represent a safe, minimal/minimally invasive, and effective form of treatment, especially for REP patients whose lesions are located close to vital organs or major blood vessels and whose imaging findings consider villi encroaching on organ parenchyma or vessel walls. However, the sample size of patients treated with image-guided local injection of MTX for REP is too small to date, and future randomized controlled trials with larger samples are needed to demonstrate the efficacy and safety of this treatment.
Mifepristone can cause embryonic cell necrosis and terminate early pregnancy and has been used to treat common types of EP.19 Hou et al reported that the preoperative application of Mifepristone significantly reduced intraoperative bleeding, thus suggesting that Mifepristone may be an effective agent for the treatment of REP.17 However, we still need to be alert to some of the side effects of Mifepristone, such as hemorrhage, sepsis, and an increased risk of infection.20
Conclusion
REP is an extremely rare and specific type of EP for which specific pathogenesis has yet to be elucidated. Given the propensity of REP to implant adjacent to major blood vessels and vital organs, rupture can be life-threatening to patients; thus, clinicians should pay more attention to REP. Combined imaging, including ultrasound (TAS and TVS), CT and MRI, is recommended to identify the location of the lesion and fully evaluate the condition. Once a definitive diagnosis is made, appropriate treatment should be administered immediately. Surgery remains the primary treatment for REP and can be preceded by diagnostic laparoscopy; the next step in treatment is subject to a specific situation. Moreover, the image-guided local injection of MTX may be an effective treatment for REP.
Study Location
The study was carried out in the second affiliated hospital of Dalian medical university in Dalian, China.
Data Sharing Statement
All data analyzed during this study are available within reasonable request to the corresponding author.
Ethics Approval
This paper was approved by the Ethics Committee of the Institutional Review Board (IRB) of the second affiliated hospital of Dalian Medical University.
Consent for Publication
Written informed consent was obtained from the patient for the publication of this report.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. OuYang Z, Yin Q, Wu J, Zhong B, Zhang M, Li F. Ectopic pregnancy following in vitro fertilization after bilateral salpingectomy: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2020;254:11–14. doi:10.1016/j.ejogrb.2020.08.046
2. Fetischeva LE, Mozes VG, Zakharov IS. ACOG practice bulletin no. 193 summary: tubal ectopic pregnancy. Obstet Gynecol. 2018;131:613–615. doi:10.1097/AOG.0000000000002559
3. Centers for Disease Control and Prevention (CDC). Ectopic pregnancy-United States, 1990–1992. MMWR Morb Mortal Wkly Rep. 1995;44:46–48.
4. Le MT, Huynh MH, Cao CH, Hoang YM, Le KC, Dang VQ. Retroperitoneal ectopic pregnancy after in vitro fertilization/embryo transfer in patient with previous bilateral salpingectomy: a case report. Int J Gynaecol Obstet. 2020;150:418–419. doi:10.1002/ijgo.13136
5. Huang X, Zhong R, Tan X, et al. Conservative management of retroperitoneal ectopic pregnancy by computed tomographic-guided methotrexate injection in the gestational sac: 2 case reports and literature review. J Minim Invasive Gynecol. 2019;26:1187–1192. doi:10.1016/j.jmig.2018.12.016
6. Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod. 2002;17:3224–3230. doi:10.1093/humrep/17.12.3224
7. Meire I, van Heusden A, Roukema MS, Niezen RA, Dhont MA. retroperitoneal pregnancy of an anencephalic fetus. J Obstet Gynaecol. 2007;27:518–519. doi:10.1080/01443610701465071
8. Hall JS, Harris M, Levy RC, Walrond ER. Retroperitoneal ectopic pregnancy. J Obstet Gynaecol Br Commonw. 1973;80:92–94. doi:10.1111/j.1471-0528.1973.tb02140.x
9. Persson J, Reynisson P, Måsbäck A, Epstein E, Saldeen P. Histopathology indicates lymphatic spread of a pelvic retroperitoneal ectopic pregnancy removed by robot-assisted laparoscopy with temporary occlusion of the blood supply. Acta Obstet Gynecol Scand. 2010;89:835–839. doi:10.3109/00016341003623779
10. Liang C, Li X, Zhao B, Du Y, Xu S. Demonstration of the route of embryo migration in retroperitoneal ectopic pregnancy using contrast-enhanced computed tomography. J Obstet Gynaecol Res. 2014;40:849–852. doi:10.1111/jog.12233
11. Veleminsky M, Stepanek O, Koznar P, Michal M, Mainzerová P, Stikova ZA. rare case of ectopic pregnancy - retroperitoneal ectopic pregnancy. Neuro Endocrinol Lett. 2018;39:156–159.
12. Xu H, Cheng D, Yang Q, Wang D. Multidisciplinary treatment of retroperitoneal ectopic pregnancy: a case report and literature review. BMC Pregnancy Childbirth. 2022;22:472. doi:10.1186/s12884-022-04799-5
13. Iwama H, Tsutsumi S, Igarashi H, Takahashi K, Nakahara K, Kurachi HA. case of retroperitoneal ectopic pregnancy following IVF-ET in a patient with previous bilateral salpingectomy. Am J Perinatol. 2008;25:33–36. doi:10.1055/s-2007-1004829
14. Ferland RJ, Chadwick DA, O’Brien JA, Granai CO. An ectopic pregnancy in the upper retroperitoneum following in vitro fertilization and embryo transfer. Obstet Gynecol. 1991;78:544–546.
15. Dmowski WP, Rana N, Ding J, Wu WT. Retroperitoneal subpancreatic ectopic pregnancy following in vitro fertilization in a patient with previous bilateral salpingectomy: how did it get there? J Assist Reprod Genet. 2002;19:90–93. doi:10.1023/A:1014451932539
16. Reid F, Steel M. An exceptionally rare ectopic pregnancy. Bjog. 2003;110:222–223. doi:10.1046/j.1471-0528.2003.01172.x
17. Hou Q, Xin L, Jian L, Pan J, Chen L, Song W. Retroperitoneal ectopic pregnancy: a case report and literature review. J Obstet Gynaecol Res. 2021;47:1186–1190. doi:10.1111/jog.14669
18. Ansong E, Illahi GS, Shen L, Wu X. Analyzing the clinical significance of postoperative methotrexate in the management of early abdominal pregnancy: analysis of 10 cases. Ginekol Pol. 2019;90:438–443. doi:10.5603/GP.2019.0078
19. Zhang W. Wang L Mifepristone in treating ectopic pregnancy. Chin Med J. 1999;112:376–378.
20. Shu SR, Luo X, Wang ZX, Yao YH. Cesarean scar pregnancy treated by curettage and aspiration guided by laparoscopy. Ther Clin Risk Manag. 2015;11:1139–1141. doi:10.2147/TCRM.S86083
21. Sotus PC. Retroperitoneal ectopic pregnancy: a case report. JAMA. 1977;238:1363–1364. doi:10.1001/jama.1977.03280140041007
22. Lee JW, Sohn KM, Jung HS. Retroperitoneal ectopic pregnancy. AJR Am J Roentgenol. 2005;184:1600–1601. doi:10.2214/ajr.184.5.01841600
23. Chang YL, Ko PC, Yen CF. Retroperitoneal abdominal pregnancy at left paracolic sulcus. J Minim Invasive Gynecol. 2008;15:660–661. doi:10.1016/j.jmig.2008.05.005
24. Lin JX, Liu Q, Ju Y, Guan Q, Wu YZ, Zheng N. Primary obturator foramen pregnancy: a case report and review of literature. Chin Med J. 2008;121:1328–1330. doi:10.1097/00029330-200807020-00016
25. Bae SU, Kim CN, Kim KH, et al. Laparoscopic treatment of early retroperitoneal abdominal pregnancy implanted on inferior vena cava. Surg Laparosc Endosc Percutan Tech. 2009;19:e156–e158. doi:10.1097/SLE.0b013e3181ab91b0
26. Okorie CO. Retroperitoneal ectopic pregnancy: is there any place for non-surgical treatment with methotrexate? J Obstet Gynaecol Res. 2010;36:1133–1136. doi:10.1111/j.1447-0756.2010.01270.x
27. Martínez-Varea A, Hidalgo-Mora JJ, Payá V, Morcillo I, Martín E, Pellicer A. Retroperitoneal ectopic pregnancy after intrauterine insemination. Fertil Steril. 2011;95:2433.e1–3. doi:10.1016/j.fertnstert.2011.02.026
28. Jiang W, Lv S, Sun L, Singer G, Xu C, Lu X. Diagnosis and treatment of retroperitoneal ectopic pregnancy: review of the literature. Gynecol Obstet Invest. 2014;77:205–210. doi:10.1159/000353691
29. Protopapas A, Akrivos N, Athanasiou S, Chatzipapas I, Domali A, Loutradis D. Ultrasound-assisted intraoperative localization and laparoscopic management of a previously missed unruptured retroperitoneal ectopic pregnancy. Gynecol Surg. 2014;11:207–211. doi:10.1007/s10397-014-0847-3
30. Ouassour S, Filali AA, Raiss M, et al. Retroperitoneal Ectopic Pregnancy: diagnosis and Therapeutic Challenges. Case Rep Surg. 2017;2017:9871865. doi:10.1155/2017/9871865
31. Yang M, Cidan L, Zhang D. Retroperitoneal ectopic pregnancy: a case report and review of the literature. BMC Pregnancy Childbirth. 2017;17:358. doi:10.1186/s12884-017-1542-y
32. Pak JO, Durfee JK, Pedro L, Osborne A, Larkins-Pettigrew M. Retroperitoneal Ectopic Pregnancy. Obstet Gynecol. 2018;132:1491–1493. doi:10.1097/AOG.0000000000002965
33. Yang Y, Liu Z, Song L, Liu H, Li L, Meng Y. Diagnosis and surgical therapy of the retroperitoneal ectopic pregnancy: a case report. Int J Surg Case Rep. 2018;49:21–24. doi:10.1016/j.ijscr.2018.05.027
34. Zhang M, Qin LL. A case of retroperitoneal para-aortic ectopic pregnancy detected by sonography. J Clin Ultrasound. 2018;46:412–414. doi:10.1002/jcu.22554
35. Lu Q, Zhang Z, Zhang Z. Laparoscopic management of retroperitoneal ectopic pregnancy. J Minim Invasive Gynecol. 2019;26:405–406. doi:10.1016/j.jmig.2018.07.007
36. Wang X, Ma D, Zhang Y, et al. Rare heterotopic pregnancy after frozen embryo transfer: a case report and literature review. BMC Pregnancy Childbirth. 2020;20:542. doi:10.1186/s12884-020-03214-1
37. Anh ND, Hai NX, Ha NT, Toan NK, Thuong PH, Duc NM. Retroperitoneal ectopic pregnancy after in vitro fertilization: a case report of a patient with bilateral salpingectomy. Radiol Case Rep. 2022;17:721–724. doi:10.1016/j.radcr.2021.12.011
38. Wen X, Yan X, Zhang Q, Dong P, Zhou L, Wang S. Retroperitoneal ectopic pregnancy: a case report. J Minim Invasive Gynecol. 2021;28:1662–1665. doi:10.1016/j.jmig.2021.05.008
39. Di Lorenzo G, Romano F, Mirenda G, et al. ”Nerve-sparing” laparoscopic treatment of parametrial ectopic pregnancy. Fertil Steril. 2021;116:1197–1199. doi:10.1016/j.fertnstert.2021.05.106
40. Yuan J, Xie H, Chen M, Zeng F, Xiao S. A case report of retroperitoneal ectopic pregnancy with lymphatic migration after in vitro fertilization-embryo transfer: an explanation to embryo distant migration. Fertil Steril. 2022;118:598–600. doi:10.1016/j.fertnstert.2022.05.034
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


