Back to Journals » Research Reports in Clinical Cardiology » Volume 13
A Case of Infective Endocarditis and Pulmonary Septic Emboli Caused by Coagulase-Negative Staphylococci
Authors Abdi IA , Nur AAA, Duale A
Received 31 July 2022
Accepted for publication 21 November 2022
Published 28 November 2022 Volume 2022:13 Pages 95—99
DOI https://doi.org/10.2147/RRCC.S384433
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Kones
Ishak Ahmed Abdi,1 Abdirahim Ali Adan Nur,2 Abdirahman Duale3
1Department of Cardiology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 2Department of Infectious Disease, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 3Department of Pulmonary Disease, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somaia
Correspondence: Ishak Ahmed Abdi, Department of Cardiology, Mogadishu Somali Turkish Training and Research Hospital, Second Street, Black Sea, Hodan District, Mogadishu, Somalia, Tel +252 618439596, Email [email protected]
Abstract: Infectious endocarditis (IE) is a serious illness that puts the patient’s life at risk and renders them severely disabled. Right-sided IE is referred to as infective endocarditis that affects the tricuspid or pulmonic valve. In the 1980s, a coagulase-negative staphylococci (CoNS) member has been identified as a causative agent of infective endocarditis. Coagulase-negative staphylococci (CoNS) form a vast majority of gram-positive cocci shared by their mutual lack of the virulence factor coagulase. More than 50 distinct CoNS species have so far been identified. Six species in total are thought to have a higher therapeutic importance, including S. S. epidermidis, S. saprophyticus, S. haemolyticus, S. capitis as well as S. lugdunensis. Several species, such as S. Serious clinical illness is known to be caused by lugdunensis. In prosthetic valves, CoNS causes 20– 45% of endocarditis cases. Most strains of contamination are methicillin-resistant and typically occur after surgery. CoNS are not frequently found in native valve endocarditis, 1– 3% are the typical percentages given. Pulmonary artery embolization (PAE) is a serious consequence of infected endocarditis (IE). We report a case of 37 years old with right-sided valve endocarditis caused by coagulase-negative endocarditis complicated by septic embolism.
Keywords: Infective endocarditis, coagulase-negative staphylococci, septic embolism, right-sided infective endocarditis, tricuspid valve vegetation
Introduction
Right-sided infective endocarditis (RSIE) is referred to as infective endocarditis that affects the tricuspid or pulmonic valve. The percentage of cases with isolated right-sided IE is around 10%, and the percentage of cases of concurrent left- and right-sided IE is around 12%.1,2 Native valve endocarditis caused by coagulase-negative staphylococci (CoNS) was a rare occurrence, although recently cCoNS native valve involvement has increased. Previously, it was believed that CoNS was a less harmful pathogen that exclusively resulted in opportunistic infections or infections of foreign objects, such as endocarditis in prosthetic valves and in situ grafts. This historical viewpoint is shifting; however there have been notable recent increases in the incidence of CoNS-induced native valve endocarditis.3,4 Non-intravenous drug users who develop tricuspid valve endocarditis might do so for a number of reasons, such as congenital heart disease, intra cardiac devices, central venous catheters, and immunologically compromised people. Rare cases of RSIE have been reported after septic abortion, abscess, and septic arthritis.3,5,6 Septic thrombophlebitis, or SPE, is a rare disorder in which microorganisms implant in the circulatory system of the lungs as a result of embolization from an infectious nidus, such as TV vegetation, an infected venous catheter, or very rarely from periodontal disease.7 From case investigations conducted as early as 1883, infectious endocarditis has been identified as a frequent cause of septic emboli.8 We report a case of 37 years old with right-sided valve endocarditis caused by coagulase-negative endocarditis complicated by septic embolism.
Case Presentation
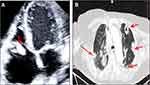
A 37-year-old multiparous woman with history of septic abortion before 3 weeks became febrile and shortness of breath associated with pleuritic chest pain, coughs, and chills in a week. She was a very weak patient brought to the emergency department with a walker. She had no chronic disease. Her vital signs were 38.5 °C, normotensive (BP 128/78 mmHg), pulse rate of 110 bpm, and SPO2 88 in the emergency. Physical examination did not show any focus of infection through general examination rather than the previous history of septic abortion. Normal peripheral examination, ie no deep vein thrombosis signs. Upon pelvic examination normal-sized uterus with a closed cervix, no cervical pain, no discharge, and no adnexal masses were visible. Cardiac auscultation revealed a regular rate with a grade II/IV systolic pansystolic murmur, no JVD raised, and no crackles. Laboratory evaluation revealed anemia (hemoglobin 6.8 g/dL), and elevation of inflammatory markers (WBC 14,000/mm3, neutrophil count 12.9, C-reactive protein 234 mg/dL, procalcitonin 3.54 ng/mL (0–0.3 ng/mL)). Kidney function and renal function test was unremarkable. Abdominal ultrasound revealed was noted normal findings except moderate splenomegaly of 15 cm. Transthoracic echocardiography examination showed large, mobile vegetation on the tricuspid valve (Figure 1A). A blood culture was drawn immediately and while pending the blood culture a diagnosis of infective endocarditis was definitely reached. CT thorax revealed multiple cavitary and nodular lesions with sub-pleural weight were observed in both lungs (Figure 1B). She was managed in the inpatient unit with supplemental oxygen; IV fluids and broad-spectrum antibiotics (vancomycin 1 g once and ceftriaxone 500 mg 2×2). During inpatient duration she was also transfused with two units of erythrocyte transfusion. After four days of hospital stay blood culture had grown coagulase-negative staphylococci and gram stain showed clusters of gram+staphylococci (Figure 2). The susceptibility testing revealed sensitive to all routine used antibiotics except penicillin G. The vancomycin was upgraded to twice daily after blood culture result. On the sixth day the patient's temperature reduced and an echocardiography repeated on the 7thday revealed mild tricuspid regurgitation, TR velocity 2.8 cm/s, and no tricuspid valve vegetation. The patient's situation improved after 8 days of hospital and was decided to discharge from the hospital with oral antibiotics clindamycin 500 mg 2×1. Three weeks later the patient was followed in the outpatient clinic, and blood culture was negative for bacterial growth and she was enjoying a good health.
 |
Figure 2 Blood agar media showing positive cocci in clusters. |
Discussion
Infective endocarditis (IE), which was first identified in the middle of the 16th century, is known for having a high in-hospital mortality rate 17–30%.9 Infective endocarditis is a microbial infection of the heart valves, intra cardiac device, septal defects, mural endocardium, or, in rare cases, the subvalvular apparatus. The typical symptoms of right-sided infectious endocarditis include fever, persistent bacteremia, and septic emboli to the lungs. Initial symptoms of septic emboli to the lungs can include hemoptysis, coughing, or chest discomfort. Patients with RSIE frequently exhibit septic shock, renal failure, and uncontrolled disseminated infection without obvious risk factors. Tricuspid regurgitation is the most frequent cardiac consequence of tricuspid valve endocarditis (TVE), and in addition to vegetation size, its severity is a predictor of mortality. In the presence of the “tricuspid syndrome”, which includes recurrent pulmonary episodes, anemia, and microscopic hematuria, clinical suspicion of should be increased of TVE.6,10,11 Medical treatment continues to be the cornerstone of TVE management. The mainstay of treatment is intravenous antibiotics adjusted to culture and sensitivity results with initial coverage of assumed pathogen.10,12 Surgery is required in 5–16% of TVE cases, and it must be taken into account in the following circumstances: 1) persistent bacteremia despite use of appropriate antimicrobial therapy; 2) right-sided intractable heart failure with poor response to diuretics; 3) large vegetation (>20 mm) that does not shrink in size despite repeated embolism; 4) fungal endocarditis; 5) concurrent left-sided IE; and 7) prostatic valve endocarditis. For tricuspid valve endocarditis, valvectomy, valve replacement, or valve repair are often performed procedures.10,12,13 An improvement was seen after 6 weeks of intravenous vancomycin therapy in a case report by Kumar et al.14 CoNS are not frequently found in native valve endocarditis, 1–3% are the typical percentages reported in the literature. The majority of patients with native IE caused by coagulase-negative staphylococcus are treated surgically, according to the literature, but a few cases have been documented to be managed medically.3
In this case report, the blood culture was obtained using a septic approach, and three bottles were drawn at different times to rule out contamination and lengthen the time it took for a positive result.
As reported in many literatures most coagulase-negative staphylococcal clinical isolates were resistant to penicillin G (100%), gentamicin (83.3%), and oxacillin (91.7%) and susceptible to vancomycin (100%), ciprofloxacin (100%), and rifampicin (79.2%).15
In our susceptibility test many drugs has been sensitive like vancomycin and ciprofloxacin and were resistant to penicillin G. Vancomycin is the drug of choice for CoNS. Other drugs like daptomycin, linezolid, and clindamycin have activity against coagulase-negative staphylococci.
In conclusion we described a 33-year-old lady who had previously experienced a septic abortion and who complained of having a fever, chills, and SOB. The patient was diagnosed with right-sided infective endocarditis, which was brought on by coagulase-negative staphylococcus and worsened by septic emboli; medical care was provided for the patient.
Data Sharing Statement
We declared that we had full access to all of the data in this study, and we take complete responsibility for the integrity of the data. All original data are available in the Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia. Data used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval
Based on the regulations of the review board of the Mogadishu Somali Turkish Training and Research Hospital, institutional review board approval is not required for case reports.
Consent for Publication
Written informed consent was obtained from the patient to have the case details and any accompanying images published.
Acknowledgment
We thank to the patient who gave their consent to be published in this case report.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, case presentation, discussion or in all these areas; took part in drafting, revising or critically reviewing the case; gave final approval of the version to be published; have agreed on the journal to which the case has been submitted; and agree to be accountable for all aspects of the work.
Funding
We declare that we have no funding source.
Disclosure
The authors declare no conflicts of interest in relation to this work.
References
1. Chahoud J, Sharif Yakan A, Saad H, Kanj SS. Right-sided infective endocarditis and pulmonary infiltrates. Cardiol Rev. 2016;24(5):230–237. doi:10.1097/CRD.0000000000000095
2. Akinosoglou K, Apostolakis E, Marangos M, Pasvol G. Native valve right sided infective endocarditis. Eur J Intern Med. 2013;24(6):510–519. doi:10.1016/j.ejim.2013.01.010
3. Abdi IA, Nur AA, Karataş M, Mohamud MF. Post-splenectomy native valve endocarditis caused by coagulase negative staphylococci: a rare case report. Ann Med Surg. 2022;103929. doi:10.1016/j.amsu.2022.103929
4. Kirkwood ML, Knowles M, Modrall JG, Valentine RJ. Mycotic inferior mesenteric artery aneurysm secondary to native valve endocarditis caused by coagulase-negative Staphylococcus. Ann Vasc Surg. 2014;28(5):1312–e13. doi:10.1016/j.avsg.2013.08.023
5. Raut N, Potdar A, Sharma S. Tricuspid valve endocarditis in non-drug abusers: a case series from India. Indian Heart J. 2018;70(4):476–481. doi:10.1016/j.ihj.2017.09.011
6. Ortiz C, López J, García H, et al. Clinical classification and prognosis of isolated right-sided infective endocarditis. Medicine. 2014;93(27):27. doi:10.1097/MD.0000000000000137
7. Cook RJ, Ashton RW, Aughenbaugh GL, Ryu JH. Septic pulmonary embolism: presenting features and clinical course of 14 patients. Chest. 2005;128(1):162–166. doi:10.1378/chest.128.1.162
8. Edgeworth FH. Case of septic endocarditis with cerebral embolism. Bristol Med Chir J. 1891;9(32):89–93.
9. Cahill TJ, Prendergast BD. Infective endocarditis. Lancet. 2016;387(10021):882–893. doi:10.1016/S0140-6736(15)00067-7
10. Hussain ST, Witten J, Shrestha NK, Blackstone EH, Pettersson GB. Tricuspid valve endocarditis. Ann Cardiothorac Surg. 2017;6(3):255. doi:10.21037/acs.2017.03.09
11. Heydari AA, Safari H, Sarvghad MR. Isolated tricuspid valve endocarditis. Int J Inf Dis. 2009;13(3):e109–e111. doi:10.1016/j.ijid.2008.07.018
12. Revilla A, López J, Villacorta E, et al. Isolated right-sided valvular endocarditis in non-intravenous drug users. Rev Esp Cardiol. 2008;61(12):1253–1259. doi:10.1016/S1885-5857(09)60052-9
13. Meel R. Right-Sided Infective Endocarditis Secondary to Intravenous Drug Abuse. Infective Endocarditis; 2019.
14. Kumar B, Chauhan G, Soni S, Singh A. Rare or rarely detected: septic pulmonary embolism with tricuspid valve infective endocarditis after an unsafe abortion. India J Med Specialities. 2020;11(4):226. doi:10.4103/INJMS.INJMS_109_20
15. Qu Y, Daley AJ, Istivan TS, Garland SM, Deighton MA. Antibiotic susceptibility of coagulase-negative staphylococci isolated from very low birth weight babies: comprehensive comparisons of bacteria at different stages of biofilm formation. Ann Clin Microbiol Antimicrob. 2010;9(1):1–2. doi:10.1186/1476-0711-9-16
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.