Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
A Case of Coma Bullae Associated with Brachioradial Artery
Authors Niu M, Deng LJ , Wu RB, Lu ZZ
Received 17 May 2023
Accepted for publication 5 July 2023
Published 18 July 2023 Volume 2023:16 Pages 1857—1864
DOI https://doi.org/10.2147/CCID.S418477
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Anne-Claire Fougerousse
Mu Niu,1,* Li-Jun Deng,2,* Rui-Bin Wu,2 Zhen-Zhong Lu2
1Department of Dermatology, The Fifth People’s Hospital of Hainan Province, Affiliated Dermatology Hospital of Hainan Medical University, Haikou, People’s Republic of China; 2Department of Dermatology, Wuzhong People’s Hospital, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Rui-Bin Wu; Zhen-Zhong Lu, Wuzhong People’s Hospital, Suzhou, People’s Republic of China, Email [email protected]; [email protected]
Abstract: We present the first case of coma bullae observed in a 67-year-old woman due to pressure and ischemia associated with brachioradial artery. A skin biopsy taken from the ulcer border revealed extensive loss of the epidermis, fibrosis of dermis, mild infiltration by lymphocytes and neutrophils, and necrosis of the focal eccrine ducts. CT angiography of the right upper limb showed a high origin of the radial artery, meanwhile both high originating radial artery and the anastomoses were tortuous and were of relatively small caliber. The diagnosis of coma bullae was made. After tissue debridement, the skin lesions gradually recovered, leaving atrophic scars.
Keywords: coma bullae, brachioradial artery
Introduction
Coma blisters or coma bullae (CB) are usually associated with overdose of pharmacological agents and alcohol, or in the setting of neurological conditions and metabolic alterations. CB present as tense blisters, erosions, or violaceous plaques appearing on healthy skin and/or erythema and plaques in regions of compression during unconscious states. We report a case observed in a female due to pressure and ischemia associated with brachioradial artery and discuss the potential underlying mechanisms.
Case Presentation
A 67-year-old woman presented with purpura and ulcer on her right arm and hand. She indicated that she developed multiple erythema, plaques, vesicles and bullae over her right upper extremity 25 days ago. Neither medication use nor history of medical conditions was noted. The only notable thing was that the patient had taken a 2-hour nap with her right arm laying under her head while watching TV on the couch the day before the rash. There was no fever, pain, numbness or any other discomfort. She was first admitted to a local hospital with the diagnosis of “infection of right upper limb”. Laboratory tests revealed no significant abnormalities except for low-titers (1:100) ANA. Multiple tissue cultures for bacteria and fungi as well as bilateral upper limb vessels Doppler ultrasonography were negative. Tests for autoantibodies including Dsg1, Dsg3, BP180, BP230 and type VII collagen were negative. Blisters were “absorbed” and dried up leaving ulcers, necrosis and violet patches after fifteen days. Then the patient came to our hospital complaining of non-healing ulcers. Physical exam revealed several variously sized purpura, necrosis, erosion and ulcers located on her right arm and hand (Figure 1A and B).
Figure 1 Continued. Figure 1 Continued.

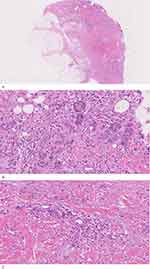
A skin biopsy taken from the ulcer border revealed extensive loss of the epidermis, fibrosis of dermis (Figure 2A), mild infiltration by lymphocytes and neutrophils (Figure 2C), and necrosis of the focal eccrine ducts (Figure 2B). Inflammation affected the superficial layer of fat only. Damage or thrombosis of the vessels in the lower dermis was not observed. CT angiography of the right upper limb showed a high origin of the radial artery, meanwhile both high originating radial artery and the anastomoses were tortuous and were of relatively small caliber (Figure 1E and F). The diagnosis of coma bullae was made. Without any other specific treatment except tissue debridement during two weeks, her ulcers diminished and most of the purpuras fell off, leaving focal atrophic scars (Figure 1C and D). There was no erythema, bullae or ulcers on any part of her skin during a 2-year follow-up after discharge (Figure 3A and B).
Discussion
Coma blisters or coma bullae (CB) are usually associated with overdose of pharmacological agents and alcohol, or in the setting of neurological conditions and metabolic alterations.1 Clinically, the lesions present as tense blisters, erosions, or violaceous plaques appearing on healthy skin and/or erythema and plaques in regions of compression during unconscious states. The characteristic histopathological finding is necrosis of eccrine sweat glands or sweat duct keratinocytes. The exact etiopathogenesis remains unclear. It has been reported in non-coma cases.2,3 While an increasing number of drugs have been implicated, there is no direct evidence of relation between CB and any specific drug.4 In addition, coma blisters located not only in pressure areas but also in nonpressure-bearing sites, suggests that additional mechanisms may be involved besides dermal pressure damage.1 It is likely to be multifactorial with prolonged pressure, hypoxia, drug toxicity, trauma as well as immune-mediated mechanisms.1 Here, we present the first case observed in a female related to brachioradial artery. She did not experience coma or usage of any medicine.
The brachioradial artery is defined as a radial artery with a high origin. Recent studies have indicated that a high origin of the radial artery is of relatively small caliber and is associated with a more tortuous course,5 which may predispose to symptomatic ischemia by altering the collateral systems in the forearm and hand.6 To our knowledge, our patient did not experience coma or usage of any medicine. We suspected that while falling asleep resting her head on her right forearm, blood supply from the ulnar artery was reduced or interrupted by compression. Meanwhile, collateral flow was unable to compensate due to her slender radial artery, contributing to critical ischemia in the right upper extremity. Besides, ischemia-reperfusion injury after revascularization may have aggravated tissue damage.7
Generally, differential diagnosis may include autoimmune bullous diseases, bullosis diabeticorum and arterial occlusion. Negative tests for autoantibodies and blood glucose as well as history of medical conditions ruled out autoimmune bullous diseases and bullosis diabeticorum. Our female patient had no symptoms of artery occlusion or ischemia in her upper limb previously. CT angiography (CTA) and color Doppler flow imaging did not show vascular lumen stenosis or arterial disease due to arteriosclerosis. Normal tests for cholesterol as well as no intravascular thrombosis observed in histopathology, did not support the diagnosis of arterial occlusion, which is usually seen in smoking men with abnormal cholesterol, in their lower extremities. As no blisters but just purpura, necrosis, erosion and ulcers were observed in our patient on admission, it needs to be differentiated from necrotizing fasciitis, purpura fulminans and pyoderma gangrenosum. Necrotizing fasciitis is a rapidly progressive bacterial infection including necrotizing forms of fasciitis, myositis and cellulitis. Negative results of bacterial and fungal culture as well as inflammation in the biopsy that affected the superficial layer of fat only, did not support the diagnosis of necrotizing fasciitis. Idiopathic purpura fulminans is an acute purpuric rash characterized by thrombosis and disseminated necrosis of the microvasculature which is associated with infection or complications of warfarin therapy. Without systemic symptoms such as fever, hemorrhage and hypotension, abnormalities in coagulation system examination or intravascular thrombosis, the diagnosis of purpura fulminant was not established. Pyoderma gangrenosum (PG) is a noninfectious neutrophilic dermatosis associated with an underlying disease including inflammatory arthritis and inflammatory bowel disease. However, violaceous plaques or purpura did not appear in PG, and no characteristic cribriform pitting was observed in our case.
Conclusion
We reported a case of coma bullae associated with brachioradial artery and discussed the potential underlying mechanisms.
Ethics Statement
The publication of images was included in the patient’s consent for publication of the case. The Hospital Ethics Committees of the Fifth People’s Hospital of Hainan Province gave approval to publish the case details.
Acknowledgments
We would like to thank the patient and physicians for participating in our study.
Funding
This work was supported by Hainan Province Clinical Medical Center.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Torres-Navarro I, Pujol-Marco C, Roca-Ginés J, Botella-Estrada R. Coma blisters. A key to neurological diagnosis. Neurologia. 2020;35(7):512–513. Epub 2019/03/13. Ampollas por coma. Una clave para el diagnóstico neurológico. doi:10.1016/j.nrl.2018.11.005
2. Heinisch S, Loosemore M, Cusack CA, Allen HB. Coma blisters sans coma. Cutis. 2012;90(3):137–139.
3. Ferreli C, Sulica VI, Aste N, et al. Drug-induced sweat gland necrosis in a non-comatose patient: a case presentation. J Eur Acad Dermatol Venereol. 2003;17(4):443–445. doi:10.1046/j.1468-3083.2003.00695.x
4. Ruiz-Rivero J, Pulido-Pérez A, Suárez-Fernández RM. Coma blisters with deep soft tissue involvement after drug overdose. Int J Dermatol. 2017;56(8):881–883. doi:10.1111/ijd.13658
5. Garg N, Sagar P, Kapoor A, et al. Arterial anomalies of the upper limb and their influence on transradial coronary procedures. J Invasive Cardiol. 2021;33(3):E165–E171.
6. Polfer EM, Sabino JM, Giladi AM, Higgins JP. Anatomical variation of the radial artery associated with clinically significant ischemia. J Hand Surg Am. 2018;43(10):952.e1–952.e5. doi:10.1016/j.jhsa.2018.02.036
7. Guo J, Yin Y, Jin L, Zhang R, Hou Z, Zhang Y. Acute compartment syndrome: cause, diagnosis, and new viewpoint. Medicine. 2019;98(27):e16260. doi:10.1097/md.0000000000016260
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.