Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
5-Aminolevulinic Acid Photodynamic Therapy Combined with Intralesional Triamcinolone and 5-Fluorouracil to Treat Acne Hypertrophic Scar
Authors Wei J , Du L , Cao Z , Li M , Zhang C , Zhang C , Meng L
Received 24 June 2023
Accepted for publication 17 October 2023
Published 27 October 2023 Volume 2023:16 Pages 3057—3064
DOI https://doi.org/10.2147/CCID.S427427
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Anne-Claire Fougerousse
Jingjing Wei, Lingyun Du, Zhiqiang Cao, Mingming Li, Chunhong Zhang, Chunmin Zhang, Liya Meng
Department of Dermato-Venereology, The Second Hospital of Shandong University, Jinan, People’s Republic of China
Correspondence: Liya Meng, Department of Dermato-venereology, The Second Hospital of Shandong University, 247 Beiyuan Dajie Street, Jinan, 250033, People’s Republic of China, Tel +86-531-85875027, Fax +86-531-88962544, Email [email protected]
Background: Acne is a chronic inflammatory disease of the pilosebaceous unit. Improper treatment of acne can lead to skin lesions in some people. Acne hypertrophic scar is relatively rare, but it significantly affects the appearance and beauty, and usually has a great psychological and social impact on patients.
Objective: To evaluate the clinical efficacy and safety of 5-aminolevulinic acid photodynamic therapy (ALA-PDT) combined with 5-fluorouracil (5-FU) injection and triamcinolone acetonide (TAC) solution in the treatment of acne hypertrophic scars.
Methods: This article included 13 outpatients with acne accompanied by acne hypertrophic scar who were treated from September 2018 to September 2022. All patients received ALA-PDT combined with intralesional injection of 5-FU and TAC. At first, patients received ALA-PDT once every two weeks. After the third ALA-PDT, 5-FU and TAC were mixed in a ratio of 3:7, and then immediately injected in the local scars. The effect was observed after 1 month. If the effect is not obvious, a further injection of 5-FU and TAC to the lesion is necessary. The patients were followed up for 6 months. The Vancouver Scars Scale (VSS) was used to evaluate the efficacy before and after treatment and photos of patients were collected.
Results: After ALA-PDT combined with intralesional 5-FU and TAC, all patients achieved good clinical efficacy. 23.08% of patients received one local injection and 76.92% received two local injections. After treatment, the scar lesions were reduced and flattened, and the scars became soft. The total score of VSS after treatment was significantly lower than before, and the difference was statistically significant (P< 0.05). The main adverse reactions were pain, erythema, and pigmentation, which can subside within 3 weeks. There was no recurrence after 6 months of follow-up.
Conclusion: ALA-PDT combined with intralesional injection of 5-FU and TAC significantly affects acne hypertrophic scars, which is worthy of further in-depth and large-scale research.
Keywords: acne hypertrophic scars, ALA-PDT, 5-FU, TAC, acne
Introduction
Acne scar occurs in the healing process of active acne, which can be caused by various types of acne, from papules, pustules, and comedones to nodular cystic acne.1,2 The distribution is associated with predilection sites for acne, such as the face, back, and chest.3 The incidence of acne scars is related to the early control of acne, body mass index, gender, family history of severe acne, scratching, and so on. Acne scars can be divided into three main types: atrophic, hypertrophic, and keloid.2 There are a number of strategies for acne hypertrophic scar, including laser treatment, cryotherapy, intralesional drug injections, surgery, and so on.4 Among them, intralesional injection of drugs such as corticosteroids combined with 5-fluorouracil has become an effective treatment for acne hypertrophic scars. ALA-PDT has been widely used and rapidly developed in dermatology. However, ALA is limited in how deep it can penetrate the skin, so it is limited in treating deeper lesions.5 Acne hypertrophic scar is mainly related to the accumulation of collagen fibers in the dermis.6 The effect of ALA-PDT alone on acne hypertrophic scar is not good, and there is a certain degree of recurrence rate.5 Therefore, ALA-PDT alone is rarely used clinically to treat acne hypertrophic scars. However, PDT can improve the vascular composition of scars by targeting the microvessels on the lesions and reducing the erythema, height, and stiffness caused by the proliferation of capillaries in hypertrophic scar.7,8 It has also been reported that the effect of laser on the skin can reduce the side effects caused by intralesional injection, such as improving the telangiectasia caused by intralesional injection of steroids.7 Therefore, we tried to combine ALA-PDT with intralesional injection of drugs to treat acne hypertrophic scars. In this article, we explored the clinical efficacy and safety of ALA-PDT combined with intralesional injection of 5-FU and TAC in the treatment of hypertrophic acne scar. The purpose of this study is to explore a more effective and safer treatment for acne hypertrophic scar and provide evidence support for its promotion.
Patients and Methods
General Information
We retrospectively collected a case series of 13 patients with hypertrophic acne scar diagnosed clinically in the outpatient clinic of the Department of Dermato-venereology, the Second Hospital of Shandong University, from 2018 to 2022. Sex, age, disease course, and the information about skin lesions of patients were recorded. Exclusion criteria included patients who had received scars treatment within the past 6 months, had any history of kidney disease or changes in liver enzyme or white blood cell counts, and women who were pregnant, nursing, or planning to become pregnant in the near future. Clinical information was obtained from medical records and clinical follow-ups. The study was approved by the Ethics Committee of the Second Hospital of Shandong University (Ethics No. KYLL-2022LW155).
Methods
ALA was diluted to a concentration of 5% and applied to the overall area with acne and hypertrophic scars in patients. The face was sealed with plastic wrap and a shading mask to prevent the solution from volatilizing and protected from light for 2 hours. The 633 nm LED red light was used to irradiate the skin covered by the drug for 20 minutes. The radiation energy is different for each patient. The conventional starting energy is 60J/cm2, and the irradiation time is generally 20 minutes. During this process, the operator can adjust the energy according to the patient’s response. For example, if the patient cannot tolerate it, the radiation energy can be reduced. If the patient’s pain is unbearable, it can be divided into two steps, that is, each down 10% of the energy density, the lighting time is extended by 5 minutes, or 40mw/cm2, lighting for 5 minutes, and then 80mw/cm2, lighting for 20 minutes. The irradiation distance was 10 cm. Once every two weeks, twice in total. 4 weeks later, 5-FU injection and TAC solution diluted in a ratio of 3:7 were injected into the hypertrophic scars immediately after the third ALA-PDT. The curative effect was observed after 1 month. If the effect was not obvious, another intralesional injection of 5-FU and TAC was performed. And the evaluation was conducted after 6 months. The Vancouver Scars Scale (VSS) (Table 1) includes four evaluation criteria: pigmentation, height, vascularity, and pliability. The VSS was used to evaluate the curative effect of left and right face respectively. The mean VSS score was used to independently assess acne hypertrophic scar in all patients before and after treatment. The data collected were statistically analyzed using SPSS (version 27.0; IBM SPSS Inc, Armonk, NY, USA). The threshold for the statistical significance was set at p < 0.05.
 |
Table 1 The Vancouver Scars Scale (VSS) |
Follow-Up
Follow-up for at least 6 months after the last treatment was conducted by combining outpatient visits with WeChat and telephone interviews.
Results
Our study included 13 patients, 3 women and 10 men, aged 19–28 (mean 22.92) years. The basic clinical information of patients is listed in Table 2. The clinical characteristics of the patients were analyzed in Table 3. 23.08% of patients received one intralesional injection and 76.92% received two intralesional injections. Patient 2 only had acne scar lesions on the right cheek. All patients were scored on the left and right cheek respectively. The score of the VSS before and after treatment is shown in Table 4. The mean VSS score before treatment was 10.56, but the mean VSS score decreased to 2.60 after treatment.
 |
Table 2 Clinical Data of Patients with Hypertrophic Acne Scar |
 |
Table 3 Analysis of Clinical Features of 8 Cases of Hypertrophic Acne Scar |
 |
Table 4 VSS Before and After Treatment |
Paired t-test was performed on the sum of VSS scores of patients before and after treatment (Table 5), and it was found that there was statistical significance before and after treatment (P<0.05). As shown in Figures 1–4, compared with before, scars lesions became smaller and flatter, scars became softer and erythema became lighter after ALA-PDT combined with intralesional injection of 5-FU and TAC.
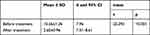 |
Table 5 t-test of the Total Score of VSS Before and After Treatment |
All treatments were well tolerated. Some patients have various degrees of erythema and moderate pain during treatment with ALA-PDT, which can be tolerated. Any adverse reactions were not observed in all patients treated with intralesional injection. At the later follow-up, most patients had no obvious feelings or external manifestations. Only a few patients developed pigmentation after the third ALA-PDT treatment, which subsided about 3 months later. All patients had no recurrence of scars and no new scars at 6 months after treatment.
Discussion
The formation of acne hypertrophic scars is mainly related to the disorder of dermal collagen fibers, excessive proliferation of fibroblasts, and excessive deposition of collagen.6 The current treatment methods mainly include intralesional injection of corticosteroid, scars revision, cryotherapy, radiotherapy, laser therapy and intralesional injection of 5-FU. Nevertheless, treatment outcomes and recurrence rates are unsatisfactory.9
PDT has been shown to be an effective treatment for acne. It can be used for mild to severe inflammatory and cystic acne and is suitable for various skin types.10 The mechanism of PDT is that a series of photochemical toxic effects occur in the target tissue under the excitation of specific wavelengths of light by photosensitizers, inducing the apoptosis of inflammatory cells, regulating the local immune state, and thus causing the damage and death of the target tissue. It has the advantages of good efficacy, small trauma, high safety, and so on.11,12 In vitro studies have shown that fibroblasts exposed to PDT have reduced expression of type 1 collagen mRNA 1761 and TGF-8, as well as decreased proliferation and mobility, which supports the mechanism of PDT in the treatment of hypertrophic scar.13 Clinical trials have also shown that PDT can improve hypertrophic scar.14 Preclinical studies have shown that PDT affects the histopathological features of both hypertrophic scar, excessive fibroblast proliferation, and collagen accumulation. However, due to the limited penetration of photosensitizers, the efficacy of PDT alone for acne hypertrophic scar is not good. Especially for scar with a depth of more than 3mm, the therapeutic effect may be poor.15 5-FU induces the proliferation of fibroblast by influencing antimetabolic activity.16,17 Since its introduction, corticosteroids, especially TAC, have been considered the most widespread and efficient treatment owing to their low recurrence rate and non-invasiveness.18,19 Clinical studies have revealed that compared with the application of steroids alone or 5-FU alone, the combination of 5-FU and TAC has a clear and lasting effect in reducing the clinical symptoms and appearance of scar.17,18 This may be related to the combination of TAC and 5-FU induced cell cycle arrest in G2 phase, down-regulated the expression of VEGF and inhibited the synthesis of COL-1 and MMP2.18 In the literature,19–21 the combined treatment of intralesional injection of 5-FU and TAC generally requires once a week for a total of 8 times, only in this way can a better therapeutic effect be obtained. Our patients had a significant improvement after combined intralesional injection of 5-FU and TAC 2 times on the basis of ALA-PDT treatment. This combination therapy reduced the total number of injections. This can not only reduce the pain caused by each injection but also reduce the side effects caused by the injection of drugs. Although the combined injection of 5-FU and TAC has reduced the symptoms of adjacent skin atrophy and pigmentation caused by the use of TAC alone, as well as the symptoms of erythema and ulcer caused by the use of 5-FU alone, the increase in the number of injections will lead to an increased risk of these side effects.18 Therefore, in our reported cases, the combined treatment of ALA-PDT combined with intralesional injection of 5-FU and TAC can not only enhance the efficacy in the case of the same number of injections but also effectively improve the skin lesions of patients with acne and reduce the occurrence of scar.
The 13 cases we reported were all acne patients with hypertrophic scar. Before the injection of 5-FU and TAC into the scars lesions, the patients were treated with 3 times of ALA-PDT. The concentration of ALA was 5%, and the low concentration reduced the irritation to the skin and reduced the economic burden of the patients. In the course of treatment, it was found that ALA-PDT was effective for acne hypertrophic scar while improving acne. However, ALA-PDT alone was slower in treating scar, so we injected 5-FU injection and TAC solution diluted in a ratio of 3: 7 into the lesions after the third photodynamic therapy. This can not only shorten the course of disease but also increase the efficacy and achieve good cosmetic results. After 3 times of ALA-PDT and 1 time of intralesional injection, the scars lesions were smaller and softer than before. However, most patients have more hypertrophic scars or have higher requirements for the recovery of facial skin lesions. Therefore, 1 month after the first intralesional injection, some patients were given the second intralesional injection of 5-FU and TAC. After treatment, the VSS scores of 13 patients were less than 4 points, and the patients were satisfied with the therapeutic effect. The lesions of the 13 cases reported in this article were located in important areas requiring high aesthetic requirements, which was extremely challenging, so we used combination therapy. All patients in this study were able to live and work as usual after combined treatment.
Conclusion
In summary, ALA-PDT combined with intralesional injection of 5-FU and TAC has a significant therapeutic effect on acne hypertrophic scar while controlling acne. The adverse reactions during the treatment subsided naturally within 3 weeks, and these were tolerable to the patients. During the follow-up of 13 cases, no recurrence of acne hypertrophic scar was found, and the smoothness and fineness of the skin were significantly improved compared with those treatment before. Therefore, this study provides a new effective and safe treatment for patients with acne scar, especially those with acne. However, further studies, such as clinical controlled trials, are needed to evaluate the efficacy and recurrence of combined therapy in patients with longer follow-up periods and to compare the efficacy with patients receiving other treatments.
Ethics and Dissemination
This study complies with the Declaration of Helsinki. All patients provided written informed consent for publication of this study and accompanying images. The study was approved by the Ethics Committee of the Second Hospital of Shandong University (Ethics No. KYLL-2022LW155).
Funding
There is no funding to report.
Disclosure
All authors declare that there are no conflicts of interest.
References
1. Fabbrocini G, Annunziata MC, D’Arco V, et al. Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080. doi:10.1155/2010/893080
2. Clark AK, Saric S, Sivamani RK. Acne scars: how do we grade them? Am J Clin Dermatol. 2018;19(2):139–144. doi:10.1007/s40257-017-0321-x
3. Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–372. doi:10.1016/S0140-6736(11)60321-8
4. Soliman YS, Horowitz R, Hashim PW, Nia JK, Farberg AS, Goldenberg G. Update on acne scar treatment. Cutis. 2018;102(1):21.
5. Liu L, Liu P, Wei G, Meng L, Zhang C, Zhang C. Combination of 5-Aminolevulinic acid photodynamic therapy and isotretinoin to treat moderate-to-severe acne. Photodiagnosis Photodyn Ther. 2021;34:102215. doi:10.1016/j.pdpdt.2021.102215
6. Slemp AE, Kirschner RE. Keloids and scars: a review of keloids and scars, their pathogenesis, risk factors, and management. Curr Opin Pediatr. 2006;18(4):396–402. doi:10.1097/01.mop.0000236389.41462.ef
7. Son IP, Park KY, Kim B, Kim MN. Pilot study of the efficacy of 578 nm copper bromide laser combined with intralesional corticosteroid injection for treatment of keloids and hypertrophic scars. Ann Dermatol. 2014;26(2):156–161. doi:10.5021/ad.2014.26.2.156
8. Trace AP, Enos CW, Mantel A, Harvey VM. Keloids and hypertrophic scars: a spectrum of clinical challenges. Am J Clin Dermatol. 2016;17(3):201–223. doi:10.1007/s40257-016-0175-7
9. Lee HJ, Jang YJ. Recent understandings of biology, prophylaxis and treatment strategies for hypertrophic scars and keloids. Int J Mol Sci. 2018;19(3):711.
10. Boen M, Brownell J, Patel P, Tsoukas MM. The role of photodynamic therapy in acne: an evidence-based review. Am J Clin Dermatol. 2017;18(3):311–321. doi:10.1007/s40257-017-0255-3
11. Gdovin MJ, Kadri N, Rios L, Holliday S, Jordan Z. Focal photodynamic intracellular acidification as a cancer therapeutic. Semin Cancer Biol. 2017;43:147–156. doi:10.1016/j.semcancer.2017.02.005
12. Liu L, Zhang C, Wei G. Photodynamic therapy combined with fire needle for a case of bullous lichen sclerosus. Photodiagnosis Photodyn Ther. 2022;41:103143. doi:10.1016/j.pdpdt.2022.103143
13. Mendoza-Garcia J, Sebastian A, Alonso-Rasgado T, Bayat A. Ex vivo evaluation of the effect of photodynamic therapy on skin scars and striae distensae. Photodermatol Photoimmunol Photomed. 2015;31(5):239–251. doi:10.1111/phpp.12180
14. Zhou ZW, Chen XD, Wu XY. 5-ALA PDT successfully treats facial hidradenitis suppurativa-induced severe hypertrophic scar. Photodiagnosis Photodyn Ther. 2019;28:343–345. doi:10.1016/j.pdpdt.2019.10.008
15. Yan D, Zhao H, Li C, et al. A clinical study of carbon dioxide lattice laser-assisted or microneedle-assisted 5-aminolevulinic acid-based photodynamic therapy for the treatment of hypertrophic acne scars. Photodermatol Photoimmunol Photomed. 2022;38(1):53–59. doi:10.1111/phpp.12716
16. Darougheh A, Asilian A, Shariati F. Intralesional triamcinolone alone or in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. Clin Exp Dermatol. 2009;34(2):219–223. doi:10.1111/j.1365-2230.2007.02631.x
17. Khalid FA, Mehrose MY, Saleem M, et al. Comparison of efficacy and safety of intralesional triamcinolone and combination of triamcinolone with 5-fluorouracil in the treatment of keloids and hypertrophic scars: randomised control trial. Burns. 2019;45(1):69–75. doi:10.1016/j.burns.2018.08.011
18. Ren Y, Zhou X, Wei Z, Lin W, Fan B, Feng S. Efficacy and safety of triamcinolone acetonide alone and in combination with 5-fluorouracil for treating hypertrophic scars and keloids: a systematic review and meta-analysis. Int Wound J. 2017;14(3):480–487. doi:10.1111/iwj.12629
19. Muneuchi G, Suzuki S, Onodera M, Ito O, Hata Y, Igawa HH. Long-term outcome of intralesional injection of triamcinolone acetonide for the treatment of keloid scars in Asian patients. Scand J Plast Reconstr Surg Hand Surg. 2006;40(2):111–116. doi:10.1080/02844310500430003
20. Asilian A, Darougheh A, Shariati F. New combination of triamcinolone, 5-Fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32(7):907–915. doi:10.1111/j.1524-4725.2006.32195.x
21. Khan MA, Bashir MM, Khan FA. Intralesional triamcinolone alone and in combination with 5-fluorouracil for the treatment of keloid and hypertrophic scars. J Pak Med Assoc. 2014;64(9):1003–1007.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




