Back to Journals » Nature and Science of Sleep » Volume 16
Sleep Quality and Cognitive Abilities in the Greek Cohort of Epirus Health Study
Authors Koutsonida M, Psyhogiou M , Aretouli E, Tsilidis KK
Received 22 August 2023
Accepted for publication 3 January 2024
Published 17 January 2024 Volume 2024:16 Pages 33—42
DOI https://doi.org/10.2147/NSS.S436519
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Valentina Alfonsi
Myrto Koutsonida,1 Maria Psyhogiou,2 Eleni Aretouli,3,* Konstantinos K Tsilidis1,4,*
1Department of Hygiene and Epidemiology, University of Ioannina, School of Medicine, Ioannina, Greece; 2Interdisciplinary Department 10B, General Hospital “Evaggelismos”, Athens, Greece; 3Department of Psychology, School of Social Sciences, University of Ioannina, Ioannina, Greece; 4Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, UK
*These authors contributed equally to this work
Correspondence: Eleni Aretouli; Konstantinos K Tsilidis, Tel +30 2651005775 ; +44 20 7594 2623, Email [email protected]; [email protected]
Purpose: Sleep is essential to all human body functions as well as brain functions. Inadequate sleep quantity and poor sleep quality have been shown to directly affect cognitive functioning and especially memory. The primary aim of the present study was to investigate the association of sleep quality with cognitive abilities cross-sectionally in a middle-aged Greek population and secondarily to examine this association prospectively in a smaller group of these participants.
Patients and Methods: A total of 2112 healthy adults aged 25– 70 years (mean: 46.7± 11.5) from the Epirus Health Study cohort were included in the analysis and 312 of them participated in secondary prospective analysis. Sleep quality was measured by the Pittsburgh Sleep Quality Index (PSQI) scale and cognition was assessed in primary cross-sectional analyses with three neuropsychological tests, namely the Verbal Fluency test, the Logical Memory test and the Trail Making test, and in secondary prospective analyses with online versions of Posner cueing task, an emotional recognition task, the Corsi block-tapping task and the Stroop task. Statistical analysis was performed using multivariable linear regression models adjusted for age, sex, education, body mass index and alcohol consumption.
Results: Attention/processing speed was the only cognitive domain associated cross-sectionally with PSQI score. Specifically, participants with better self-reported sleep quality performed faster on the Trail Making Test - Part A (β= 0.272 seconds, 95% CI 0.052, 0.493).
Conclusion: Further studies are needed to clarify the association of sleep quality with cognition, especially in middle-aged people that are still in productive working years.
Keywords: sleep quality, cognition, attention, executive functions, memory, middle-aged
Introduction
Cognitive functions are the mental processes, such as perception, memory, language, planning and problem solving, that are necessary for selection, processing, manipulation, storage and retrieval of information in order for an individual to adapt to the environment.1 Insufficient sleep quantity2–4 and poor sleep quality5,6 have been linked to impaired cognitive functions.
The processes that take place during sleep are vital and serve physiological7–9 and cognitive functions.10 Although still not well understood, these processes are thought to restore homeostasis of human body networks, renormalizing the changes occurred while being awake. It is proposed that sleep minimizes energy expenditure, promotes protein synthesis and synaptic strengthening, and eliminates metabolic waste products through glymphatic network.11 Also, sleep disruptions are linked with higher levels of amyloid plaques and tau tangles,12–14 a hallmark of cognitive decline and Alzheimer’s disease.
Sleep seems to affect particularly learning and memory consolidation, as evidenced in studies of all age ranges.15–17 Regarding the neurophysiological mechanisms involved, during non-rapid eye movement sleep (or slow-wave sleep), information encoded during wakefulness is repeatedly replayed in hippocampus, distributed and integrated in neocortical regions. This strengthens synaptic connections that are renormalized during sleep by slow oscillations. As a result, relevant information becomes more salient and irrelevant information fades away.18–20
The association between sleep quality and cognitive function has been examined in previous studies with healthy adults. There are cross-sectional21–23 as well as longitudinal studies24–27 that suggested poorer sleep quality is associated with poorer cognitive function in general; and other studies that argued poor sleep quality negatively affects selectively only specific cognitive domains using both cross-sectional28–30 and longitudinal design.31 However, there are also studies that did not find an association between sleep quality and cognition cross-sectionally32,33 or prospectively.34,35
Previous studies conducted in Greece that evaluated sleep quality in relation to cognition have shown an association both with objective36 and with subjective cognitive performance.37 However, these two studies used sample from the same cohort, aged over 65 years old. It is of note that most previous studies included elderly participants over 60 years. Thus, the relationship between sleep quality and cognition in middle-aged and in younger adults remains unclear.
The aim of this study was to investigate the association between sleep quality, as defined by the Pittsburgh Sleep Quality Index (PSQI) scale, and cognition in a Greek sample of mostly middle-aged participants without any reported neurological or psychiatric diagnosis. We used data from the Epirus Health Study (EHS), a deeply phenotyped ongoing prospective cohort study in Greece involving participants aged 25–70 years.
Materials and Methods
Study Population
The EHS started in June 2019 and is an ongoing population-based prospective cohort study, which aims to investigate the etiology of multifactorial chronic diseases and thus to improve the overall health status of the Greek population. The EHS cohort consists of permanent residents of the Epirus region in Greece, of both sexes, aged 25 to 70 years, without symptoms of active infection at entry into the study. Further details on EHS cohort study design have been published previously.38 Until 31 October 2022, a total of 2230 participants were recruited to the study and the vast majority of them were residents of the urban city of Ioannina and fluent in the Greek language.
For the purposes of the current study, we excluded participants who self-reported serious neurological (n=1 Alzheimer’s disease, n=2 Parkinson’s disease, n=19 epilepsy) or psychiatric conditions (n=57 major depression disorder and n=1 bipolar disorder). Also, we excluded 20 participants with missing data on cognitive tests and 18 participants with missing data of sleep quality scores. Thus, the analyses were performed on the remaining 2112 participants, as described in Figure 1.
 |
Figure 1 Flowchart for the identification of the study population. Note: Each outcome was determined independent of the other outcomes. |
The study was approved by the Research Ethics Committee of the University of Ioannina and is conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants prior to their participation in the study.
Data Collection
The EHS collects information on socio-demographic characteristics, general health status and lifestyle data, as well as anthropometric and clinical measurements. Specifically, all study participants were interviewed using a standard close-ended questionnaire at recruitment by two trained interviewers regarding socio-demographic characteristics (ie, sex, age, level of education, place of birth and income), general health status and lifestyle factors (ie, physical activity, alcohol consumption, smoking habits). Weight, standing height and waist circumference were measured using SECA equipment.
Pittsburgh Sleep Quality Index (PSQI)
Sleep quality was assessed using the PSQI, a tool designed by Buysse et al in 1989,39 which provides a subjective measure of sleep quality and sleep patterns. It consists of 19 self-rated questions focusing on sleep quality and disturbances in the past month, of which 4 are open-ended and the remaining 15 are closed-ended (Likert-type). Τhe 19 items generate seven component scores and then are summed to yield the total PSQI score. The seven components of PSQI are subjective sleep quality, sleep latency, sleep duration, sleep disturbances, habitual sleep efficiency, use of sleep medications and daytime dysfunction. Each component score ranges from 0 to 3, and the total PSQI score ranges from 0 to 21, with higher scores indicating severe sleep difficulties. Furthermore, a total score above five indicates poor sleep quality.
Cognitive Measurements
Assessment of cognitive functions at recruitment was conducted through standardized neuropsychological tests, the Greek versions of the Trail Making Test (TMT),40 the Verbal Fluency test (VF)41 and the Logical Memory test (LM).42,43 These tests were chosen because they are widely used to assess cognitive function and are sensitive to the presence of any cognitive decline that may occur even in preclinical stages.44 Additionally, stratification by age and level of education is performed for the available normative data concerning the Greek population, which provides useful cut-off values for cognitive impairment.
For the secondary prospective analyses, the neuropsychological tests used were the online versions of the Posner cueing task,45 an emotional word recognition task,46 the Corsi block-tapping task47 and the Stroop task.48 Participants were invited to complete the computer-based neuropsychological tests through the online platform PsyToolkit.49,50 An invitation was sent via email on 28/9/2021 to all participants recruited until August 2021, and on the last day of each month to participants recruited ever since. Until 31st October 2022, 312 participants had completed the computer-based neuropsychological tests, and secondary prospective analyses were performed on 154 participants that had completed the online neuropsychological examination at least 6 months after their initial neuropsychological examination at recruitment.
TMT, Posner cueing task and Stroop task assess attention and processing speed; VF and Stroop task assess executive functions and LM, the emotional word recognition task and Corsi block-tapping task assess memory. Total scores of VF, LM, the emotional word recognition task, and Corsi block-tapping task are the sum of correct responses and higher scores indicate better performance. Total score of TMT is the seconds needed to complete each subtest and thus, lower scores indicate better performance. Scores of Posner cueing task and Stroop task are both correct responses and seconds needed to complete each condition of test. Further details for each neuropsychological test and scoring are provided in the supplementary material (Supplementary File 1).
Statistical Analysis
Baseline characteristics of the study sample were summarized using means and standard deviations (SD) or percentages, as appropriate for continuous and categorical variables, respectively. Also, baseline sample characteristics and scores of cognitive tests were analyzed according to PSQI using independent sample t-tests or x2 tests.
PSQI scores were examined both as continuous and as categorical variables in separate models. Continuous scores of PSQI were transformed according to the cut-off score for good sleep quality (0–5 points) and poor sleep quality (6–21 points).
Multivariable linear regression analysis was used to investigate the cross-sectional association of sleep quality, measured by PSQI score, with cognition, measured by the continuous scores of the three cognitive tests conducted at recruitment. In addition, multivariable linear regression analysis was performed to examine the prospective association of sleep quality with cognition using PSQI score and the continuous scores of the four computer-based cognitive tests. We also applied multivariable linear regression analysis using binary categories of PSQI scores and continuous scores of the cognitive tests.
All models were first adjusted for age (continuous), sex and level of education (primary and secondary school, high school, and higher education) and additionally adjusted for body mass index (BMI, continuous) and alcohol consumption (never, less than once/month, 1–3 times/month, 1–2 times/week, almost every day).
Interaction analyses according to sex and age groups (young: <40 years, middle-aged: 40–59.9 years, old: ≥60 years) were performed in the fully adjusted models to test whether the associations could be modified by these factors.
A sensitivity analysis was performed after excluding participants that were not born in Greece (N=181) to control for possible language difficulties that could affect the performance on cognitive tests. However, results remained similar and consequently they are no further discussed.
Statistical analyses were performed using STATA (version 13.1; StataCorp, College Station, TX, USA). A p-value of less than 0.05 was considered statistically significant for all main analyses, but the interactions were interpreted more conservatively given the higher sample size needed for such analyses.
Results
In Table 1, sociodemographic characteristics of the study participants are presented overall and by the binary PSQI score. Overall, the mean age of participants was 46.7 (SD=11.4) years and most of them belonged to the age group 40–59 years (57.48%). Women (60.1%) and individuals of higher education (64.1%) predominated in the sample. The mean PSQI score was 4.6 points (SD=2.3), ranging from 1 to 18 and suggesting a moderate sleep quality. The majority of participants (73.2%) reported good sleep quality. The mean BMI was 26.5 kg/m2 (SD=4.9). Regarding the alcohol consumption among participants, 29.7% consumed alcoholic beverages less than once a month and 29.7% consumed alcoholic beverages once or twice a week.
 |
Table 1 Sociodemographic and Lifestyle Characteristics of Epirus Health Study Participants by Level of Sleep Quality |
Participants with poor sleep quality were older, more often women and of lower education in comparison with participants with good sleep quality. Also, participants with poor sleep quality had worse cognitive scores in both subtests of TMT (Part A and Part B) and VF (semantic and phonemic), whereas they had similar performance with participants with good sleep quality in the rest cognitive tests (Supplementary Table S1).
Follow-up period ranged from 6 months to 2 years (mean period 1.4 years) (Supplementary Table S1). Participants that had completed the prospective computer-based cognitive tests were of younger age and higher education and had lower BMI compared with participants that did not complete the prospective neuropsychological examination (Supplementary Table S2).
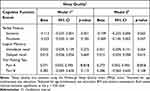
Table 2 presents the results of multivariable linear regression models that investigated the cross-sectional association between continuous scores of PSQI and the three primary cognitive tests. No significant associations were observed between continuous scores of PSQI and memory tests of LM immediate recall and delayed recall. We observed some trends toward significant associations between continuous scores of PSQI and VF semantic (b=−0.109, p=0.063) and phonemic (b=−0.069, p=0.057) subtest. A significant association was found only between PSQI and TMT A test both in basic adjusted model (b=0.271, p=0.016) and in the fully adjusted model (b=0.272, p=0.016).
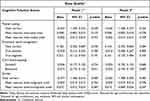
In the secondary prospective analyses that used computer-based cognitive tests to examine the association between continuous scores of PSQI and cognition, no significant associations were found (Table 3).
When binary categories of PSQI scores were used, significant associations were found for both subtests of TMT (bTMT A=1.274, p=0.028, bTMT B=1.934, p=0.036 for basic adjusted Model 1 and bTMT A=1.175, p=0.042, bTMT B=1.806, p=0.048 for fully adjusted Model 2) (Supplementary Tables S3 and S4), but not for the other primary or secondary cognitive tests.
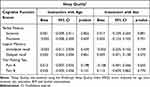
When multivariable linear regression analyses using the interaction terms by age groups and sex were performed, there was no evidence for interaction for cognitive test scores (Table 4, Supplementary Tables S5 and S6).
Discussion
In the present analysis, the main purpose was to investigate the association between sleep quality and cognitive abilities both in a cross-sectional and prospective setting, although the prospective analysis was conducted in a small subsample. The results showed a significant association between sleep quality and cognitive ability, only in the cognitive test that measures attention and processing speed assessed cross-sectionally. Namely, higher PSQI scores, implying poorer sleep quality, predicted higher scores in TMT A, indicating slower processing speed and response time in this test.
The results of our study could be explained based on the Controlled Attention Hypothesis, which posits that simpler and basic cognitive processes, such as processing speed, are more easily affected by sleep quality, in contrast with more complex cognitive processes, such as memory and executive functions.51 This can be attributed to the greater top-down control from higher-order brain areas that is needed to sustain optimal performance in more complex and challenging tasks, such as memory recall. On the contrary, vigilance tasks, assessing processing speed and reaction time, are more sensitive to sleep of insufficient quality because they demand mainly bottom-up processes that are based on prefrontal cortex,52 a brain area associated also with sleep quality.52,53 Consequently, this theory states that sleep does not affect universally cognitive functions but rather its effect is selective, depending on the characteristics of the task and the specific cognitive processes needed.
Some previous studies reported null results and supported a lack of cross-sectional association between sleep quality and executive functions30 and memory30,35 in particular. However, these findings contradict other studies that argue that poor sleep quality is cross-sectionally detrimental to both the aforementioned cognitive domains,28,54 including one study conducted in Greek older adults,36 as well as to general cognitive functioning.21 Moreover, there are longitudinal studies that confirm the negative association of sleep quality and cognition.24,27,31 Of note, one of these studies30 found only a significant relationship between sleep quality and attention using the same cognitive test but a different cut-off score for poor sleep quality compared to our study.
To the best of our knowledge, the present study is one of the few that investigated the association between sleep quality and cognitive abilities in a middle-aged population, recruited from the community with no reported neurological or psychiatric conditions. Previous studies in middle-aged healthy adults reported a negative cross-sectional association of sleep quality with memory28,29 and a negative prospective association with general cognitive levels,24,27,55 and only one study with younger mean age showed no cross-sectional associations with sleep quality.32
Disparate results possibly could not be attributed in differences in exposure measurement since both studies that found significant results between sleep quality and cognition21,22,24–26,28–31 and studies that did not report significant results,32,33,35 used PSQI to measure sleep quality. There were only five studies23,27,34,36,37 that used other types of self-reported questionnaires to measure sleep quality, and only one of them reported non-significant results.34
However, outcome measurement differed considerably among the aforementioned studies. It is noteworthy that most of the studies that reported non-significant results evaluated cognitive function with Mini-Mental State Examination (MMSE),33–35 a short screening test of global cognition, rather than domain-specific tests, that were used in studies reporting significant associations between sleep quality and cognition.23,24,28–30,36 Nevertheless, there are also studies that found significantly worse performance in participants with poor sleep quality compared with participants with good sleep quality using MMSE.21,22,26,31
Moreover, age of participants could contribute to diversity in results, as larger number of studies that found significant results included participants older than 60 years old21–23,25–28,30,31,36,37 and only two studies included middle-aged participants.24,29 In our study, we did not find a moderation effect of age, probably due to the small number of older participants included.
The results of the present study confirm the association between poor sleep quality and cognitive deficits, even in healthy middle-aged adults. In contrast with the previous studies, deficits were specific to the domain of attention. These findings indicate the need for more extensive neuropsychological assessment in individuals reporting sleep difficulties, as they may be at greater risk for cognitive impairment state.
There are potential limitations of the present study to be noted. The primarily cross-sectional design of the study prohibits the investigation of a causal relationship between sleep and cognitive deficits. Also, data on sleep quality were collected with self-reported questionnaires rather than from objective measurements, which would have provided more valid and reliable estimates. However, PSQI has been validated in the Greek population56 and it is one of the most commonly used tools worldwide. Furthermore, participants of the present study were of middle age and of higher educational level compared to different demographic characteristics of other studies, which poses limits to the potential generalization of the results.
On the other hand, several strengths of our study are noteworthy. First, the PSQI scale and cognitive tests are reliable and standardized measures with age- and education-specific normative data, resulting in increased measurement accuracy. They are also the Greek versions of widely used diagnostic tools for cognitive decline. In addition, we prospectively administered computer-based tests (although in a smaller population sample). Finally, the analyses were performed in a large population-based sample and various sociodemographic factors that could act as potential confounders in the associations between cognitive function and sleep quality were controlled for.
Conclusion
The current study suggested that sleep quality is related to attention and processing speed in a Greek population with mainly middle-aged participants. No heterogeneity of associations by sex and age were observed. Given the evidence linking poor sleep quality to cognitive dysfunction, and considering the rising number of sleep problems, it is necessary to conduct further population and intervention studies using both objective and subjective measures to examine the association of sleep quality with specific cognitive domains, which can lead to the design of targeted strategies for public health promotion.
Data Sharing Statement
Data may be available upon reasonable request to the corresponding authors.
Acknowledgments
The authors thank Konstantinos Chaliasos and Ntotsikas Evangelos for collecting data in the Epirus Health Study.
Funding
This work was funded by the projects: 1) “Understanding pathways of healthy ageing (in health and disease) through integration of high resolution omics data – pathAGE” (MIS 5047228) which is implemented under the Action “Regional Excellence in R&D Infrastructures”, funded by the Operational Programme “Competitiveness, Entrepreneurship and Innovation” (NSRF 2014–2020) and co-financed by Greece and the European Union (European Regional Development Fund), and 2) the Operational Programme Epirus 2014–2020 of the Prefecture of Epirus (MIS HΠ1AB-0028180).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kiely KM. Cognitive function. Encycl Qual Life Well Being Res. 2014;2014:974–978.
2. Lo JC, Groeger JA, Cheng GH, Dijk DJ, Chee MW. Self-reported sleep duration and cognitive performance in older adults: a systematic review and meta-analysis. Sleep Med. 2016;17:87–98. doi:10.1016/j.sleep.2015.08.021
3. Xu W, Tan CC, Zou JJ, Cao XP, Tan L. Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. J Neurol Neurosurg. 2020;91(3):236–244.
4. Hudon C, Escudier F, De Roy J, et al. Behavioral and psychological symptoms that predict cognitive decline or impairment in cognitively normal middle-aged or older adults: a meta-analysis. Neuropsychol Rev. 2020;30(4):558–579. doi:10.1007/s11065-020-09437-5
5. Bubu OM, Brannick M, Mortimer J, et al. Sleep, Cognitive impairment, and alzheimer’s disease: a systematic review and meta-analysis. Sleep. 2017;40(1). doi:10.1093/sleep/zsw032
6. Spira AP, Chen-Edinboro LP, Wu MN, Yaffe K. Impact of sleep on the risk of cognitive decline and dementia. Curr Opin Psychiatry. 2014;27(6):478–483. doi:10.1097/YCO.0000000000000106
7. Jackson CL, Redline S, Emmons KM. Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health. 2015;36(1):417–440. doi:10.1146/annurev-publhealth-031914-122838
8. Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch. 2012;463(1):121–137. doi:10.1007/s00424-011-1044-0
9. Stich FM, Huwiler S, D’Hulst G, Lustenberger C. The potential role of sleep in promoting a healthy body composition: underlying mechanisms determining muscle, fat, and bone mass and their association with sleep. Neuroendocrinology. 2022;112(7):673–701. doi:10.1159/000518691
10. Walker MP. The role of sleep in cognition and emotion. Ann N Y Acad Sci. 2009;1156(1):168–197. doi:10.1111/j.1749-6632.2009.04416.x
11. Frank MG, Heller HC. The function(s) of sleep. Handb Exp Pharmacol. 2019;253:3–34.
12. Brown BM, Rainey-Smith SR, Bucks RS, Weinborn M, Martins RN. Exploring the bi-directional relationship between sleep and beta-amyloid. Curr Opin Psychiatry. 2016;29(6):397–401. doi:10.1097/YCO.0000000000000285
13. Van Egroo M, Narbutas J, Chylinski D, et al. Sleep-wake regulation and the hallmarks of the pathogenesis of Alzheimer’s disease. Sleep. 2019;42(4). doi:10.1093/sleep/zsz017
14. Winer JR, Mander BA, Kumar S, et al. Sleep disturbance forecasts beta-amyloid accumulation across subsequent years. Curr Biol. 2020;30(21):4291–4298 e4293. doi:10.1016/j.cub.2020.08.017
15. Maski KP. Sleep-dependent memory consolidation in children. Semin Pediatr Neurol. 2015;22(2):130–134. doi:10.1016/j.spen.2015.03.008
16. Tarokh L, Saletin JM, Carskadon MA. Sleep in adolescence: physiology, cognition and mental health. Neurosci Biobehav Rev. 2016;70:182–188. doi:10.1016/j.neubiorev.2016.08.008
17. Pace-Schott EF, Spencer RM. Sleep-dependent memory consolidation in healthy aging and mild cognitive impairment. Curr Top Behav Neurosci. 2015;25:307–330.
18. Klinzing JG, Niethard N, Born J. Mechanisms of systems memory consolidation during sleep. Nat Neurosci. 2019;22(10):1598–1610. doi:10.1038/s41593-019-0467-3
19. Cellini N. Memory consolidation in sleep disorders. Sleep Med Rev. 2017;35:101–112. doi:10.1016/j.smrv.2016.09.003
20. Chambers AM. The role of sleep in cognitive processing: focusing on memory consolidation. Wiley Interdiscip Rev Cogn Sci. 2017;8(3). doi:10.1002/wcs.1433
21. Amer MS, Hamza SA, El Akkad RM, Abdel Galeel YI. Does self-reported sleep quality predict poor cognitive performance among elderly living in elderly homes? Aging Mental Health. 2013;17(7):788–792. doi:10.1080/13607863.2013.790930
22. Chang-Quan H, Bi-Rong D, Yan Z. Association between sleep quality and cognitive impairment among Chinese nonagenarians/centenarians. J Clin Neurophysiol. 2012;29(3):250–255. doi:10.1097/WNP.0b013e3182570f2e
23. Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ. Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: results from the Study on Global Ageing and Adult Health (SAGE). J Clin Sleep Med. 2014;10(6):613–621. doi:10.5664/jcsm.3782
24. Brachem C, Winkler A, Tebrugge S, et al. Associations between self-reported sleep characteristics and incident mild cognitive impairment: the Heinz Nixdorf recall cohort study. Sci Rep. 2020;10(1):6542. doi:10.1038/s41598-020-63511-9
25. Lai VKY, Fung AWT, Lam LCW, Lee ATC. Is sleep quality a potential predictor of neurocognitive disorders? A 6-year follow-up study in Chinese older adults. Int J Geriatr Psychiatr. 2022;37(8). doi:10.1002/gps.5783
26. Potvin O, Lorrain D, Forget H, et al. Sleep quality and 1-year incident cognitive impairment in community-dwelling older adults. Sleep. 2012;35(4):491–499. doi:10.5665/sleep.1732
27. Virta JJ, Heikkila K, Perola M, et al. Midlife sleep characteristics associated with late life cognitive function. Sleep. 2013;36(10):1533–1541, 1541A. doi:10.5665/sleep.3052
28. Cruz T, Garcia L, Alvarez MA, Manzanero AL. Sleep quality and memory function in healthy ageing. Neurologia. 2022;37(1):31–37. doi:10.1016/j.nrl.2018.10.001
29. Rana BK, Panizzon MS, Franz CE, et al. Association of sleep quality on memory-related executive functions in middle age. J Int Neuropsychol Soc. 2018;24(1):67–76. doi:10.1017/S1355617717000637
30. Saint Martin M, Sforza E, Barthelemy JC, Thomas-Anterion C, Roche F. Does subjective sleep affect cognitive function in healthy elderly subjects? The Proof Cohort Sleep Med. 2012;13(9):1146–1152. doi:10.1016/j.sleep.2012.06.021
31. Blackwell T, Yaffe K, Laffan A, et al. Associations of objectively and subjectively measured sleep quality with subsequent cognitive decline in older community-dwelling men: the MrOS sleep study. Sleep. 2014;37(4):655–663. doi:10.5665/sleep.3562
32. Grumbach P, Opel N, Martin S, et al. Sleep duration is associated with white matter microstructure and cognitive performance in healthy adults. Hum Brain Mapp. 2020;41(15):4397–4405. doi:10.1002/hbm.25132
33. Adam AM, Potvin O, Callahan BL, et al. Subjective sleep quality in non‐demented older adults with and without cognitive impairment. Int J Geriat Psychiatr. 2014;29(9):970–977. doi:10.1002/gps.4087
34. Jaussent I, Bouyer J, Ancelin ML, et al. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep. 2012;35(9):1201–1207. doi:10.5665/sleep.2070
35. Ma XQ, Jiang CQ, Xu L, et al. Sleep quality and cognitive impairment in older Chinese: Guangzhou Biobank Cohort Study. Age Ageing. 2019;49(1):119–124. doi:10.1093/ageing/afz120
36. Tsapanou A, Gu Y, O’Shea DM, et al. Sleep quality and duration in relation to memory in the elderly: initial results from the Hellenic longitudinal investigation of aging and diet. Neurobiol Learn Mem. 2017;141:217–225. doi:10.1016/j.nlm.2017.04.011
37. Tsapanou A, Vlachos GS, Cosentino S, et al. Sleep and subjective cognitive decline in cognitively healthy elderly: results from two cohorts. J Sleep Res. 2019;28(5):e12759. doi:10.1111/jsr.12759
38. Kanellopoulou A, Koskeridis F, Markozannes G, et al. Awareness, knowledge and trust in the Greek authorities towards COVID-19 pandemic: results from the Epirus health study cohort. BMC Public Health. 2021;21(1):1125. doi:10.1186/s12889-021-11193-x
39. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
40. Vlahou CH, Kosmidis MH. The Greek trail making test: preliminary normative data for clinical and research use. Psychology. 2002;9(3):336–352.
41. Kosmidis MH, Vlahou CH, Panagiotaki P, Kiosseoglou G. The verbal fluency task in the Greek population: normative data, and clustering and switching strategies. J Int Neuropsychol Soc. 2004;10(2):164–172. doi:10.1017/S1355617704102014
42. Kokkinis N, Kosmidis MH, Kiosseoglou G, Aretouli E. Neuropsychological Assessment Battery (Synepsy): Normative Data and Investigation of Diagnostic Validity in Mixed Neurological Population [Master’s]. Thessaloniki, Greece: Aristotle University of Thessaloniki; 2019.
43. Kosmidis MH, Bozikas V, Vlahou CH, Giaglis G. Neuropsychological Battery (Unpublished Work). Thessaloniki, Greece: Cognitive Neuroscience Laboratory, Aristotle University of Thessaloniki; 2011.
44. Jutten RJ, Sikkes SAM, Amariglio RE, et al. Identifying sensitive measures of cognitive decline at different clinical stages of alzheimer’s disease. J Int Neuropsychol Soc. 2021;27(5):426–438. doi:10.1017/S1355617720000934
45. Posner MI. Orienting of attention. Q J Exp Psychol. 1980;32(1):3–25. doi:10.1080/00335558008248231
46. Koutsonida M, Aretouli E, Kosmidis MH, Ioannidis P. Emotional Memory in Patients with Neurodegenerative Disorders [Master’s]. Thessaloniki, Greece: Aristotle University of Thessaloniki, Aristotle University of Thessaloniki; 2018.
47. Corsi PM Human memory and the medial temporal region of the brain. [Dissertation Abstracts International]; 1973;34:891.
48. Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18(6):643–662. doi:10.1037/h0054651
49. Stoet G. PsyToolkit: a software package for programming psychological experiments using Linux. Behavior Research Methods. 2010;42(4):1096–1104. doi:10.3758/BRM.42.4.1096
50. Stoet G. PsyToolkit: a novel web-based method for running online questionnaires and reaction-time experiments. Teach Psychol. 2017;44(1):24–31. doi:10.1177/0098628316677643
51. Pilcher JJ, Band D, Odle-Dusseau HN, Muth ER. Human performance under sustained operations and acute sleep deprivation conditions: toward a model of controlled attention. Aviat Space Environ Med. 2007;78(5 Suppl):B15–24.
52. Cheng W, Rolls ET, Ruan H, Feng J. Functional connectivities in the brain that mediate the association between depressive problems and sleep quality. JAMA psychiatry. 2018;75(10):1052–1061. doi:10.1001/jamapsychiatry.2018.1941
53. Sexton CE, Storsve AB, Walhovd KB, Johansen-Berg H, Fjell AM. Poor sleep quality is associated with increased cortical atrophy in community-dwelling adults. Neurology. 2014;83(11):967–973. doi:10.1212/WNL.0000000000000774
54. Benitez A, Gunstad J. Poor sleep quality diminishes cognitive functioning independent of depression and anxiety in healthy young adults. Clin Neuropsychol. 2012;26(2):214–223. doi:10.1080/13854046.2012.658439
55. Smith L, Shin JI, Jacob L, et al. Sleep problems and mild cognitive impairment among adults aged >/=50 years from low- and middle-income countries. Exp Gerontol. 2021;154:111513. doi:10.1016/j.exger.2021.111513
56. Perantoni E, Steiropoulos P, Siopi D, et al. Validation of the Greek version of Pittsburgh sleep quality questionnaire in a sleep lab population. Eur Respir Soc. 2012;40:P903.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.