Back to Journals » Journal of Pain Research » Volume 9
Words that describe chronic musculoskeletal pain: implications for assessing pain quality across cultures
Authors Sharma S , Pathak A, Jensen MP
Received 7 August 2016
Accepted for publication 15 October 2016
Published 16 November 2016 Volume 2016:9 Pages 1057—1066
DOI https://doi.org/10.2147/JPR.S119212
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Enrica Santarcangelo
Saurab Sharma,1 Anupa Pathak,2 Mark P Jensen3
1Department of Physiotherapy, Kathmandu University School of Medical Sciences, Dhulikhel Hospital Kathmandu University Hospital, Dhulikhel, 2Department of Physiotherapy, Kathmandu University School of Medical Sciences, Dhulikhel, Kavre, Nepal; 3Department of Rehabilitation Medicine, University of Washington, Seattle, WA, USA
Background: People from different cultures who speak different languages may experience pain differently. This possible variability has important implications for evaluating the validity of pain quality measures that are directly translated into different languages without cultural adaptations. The aim of this study was to evaluate the impact of language and culture on the validity of pain quality measures by comparing the words that individuals with chronic pain from Nepal use to describe their pain with those used by patients from the USA.
Methods: A total of 101 individuals with chronic musculoskeletal pain in Nepal were asked to describe their pain. The rates of the different pain descriptor domains and phrases used by the Nepali sample were then compared to the published rates of descriptors used by patients from the USA. The content validity of commonly used measures for assessing pain quality was then evaluated.
Results: While there was some similarity between patients from Nepal and the USA in how they describe pain, there were also important differences, especially in how pain quality was described. For example, many patients from Nepal used metaphors to describe their pain. Also, the patients from Nepal often used a category of pain descriptor – which describes a physical state – not used by patients from the USA. Only the original McGill Pain Questionnaire was found to have content validity for assessing pain quality in patients from Nepal, although other existing pain quality measures could be adapted to be content valid by adding one or two additional descriptors, depending on the measure in question.
Conclusion: The findings indicate that direct translations of measures that are developed using samples of patients from one country or culture are not necessarily content valid for use in other countries or cultures; some adaptations may be required in order for such measures to be most useful in new language and culture.
Keywords: pain quality, pain assessment, chronic pain, cross-cultural adaptation, musculoskeletal pain
Background
Chronic pain is a significant problem worldwide that is associated with tremendous personal and societal costs.1,2 In order to address this problem, valid and reliable measures of pain are required. One pain domain that is commonly assessed in clinical and research settings is pain quality. Whereas pain intensity can be defined as the magnitude or intensity of felt pain, pain quality refers to how the pain feels.3 The most commonly used pain quality measures in research with patients with a variety of chronic pain conditions are the McGill Pain Questionnaire (MPQ)4 and its modifications,5,6 the Pain Quality Assessment Scale (PQAS),7 and the Revised Pain Quality Assessment Scale (PQAS-R).8 Two of these, the PQAS and the PQAS-R, have demonstrated content validity as measures of pain quality in the US chronic pain populations.9,10 However, even though the PQAS has been directly translated into 17 different languages (www.mapi-trust.org), to our knowledge, the content validity of the PQAS – or any existing pain quality measure that was developed in Western countries – has been evaluated only in English-speaking patients in the USA.9,10 Although the results of this research support the content validity of the PQAS in patients from the USA, this does not ensure its content validity in patients from other countries, including patients from Asian countries.
A number of guidelines for translation of patient-reported outcome measures to different languages highlight the important contribution of cultural factors that can affect the validity of the translated measure. Therefore, consideration of cultural issues during the translation process is extremely important before we can determine that the translated measure is valid.11–14
For example, people living in Nepal differ from individuals living in the USA on a number of important factors, including socioeconomic status, culture, ethnicity, and education status. They may also differ with respect to their beliefs about their cause of pain. These factors could in turn influence how people in Nepal describe their pain. Thus, before existing measures of pain quality can be recommended for use in non-English-speaking populations – in particular, perhaps in populations who differ culturally from individuals in the USA – research is needed to evaluate their content validity in the new populations.11
To address this need, here we sought to better understand the role that language and culture may play in how people describe their pain by 1) determining the words that individuals with chronic musculoskeletal pain from Nepal use to describe their pain and comparing these with those most commonly used by patients from the USA and 2) evaluating the validity of pain quality measures developed for use in patients from Western countries and comparing them with those developed for use in patients from a non-Western country. We hypothesized that while patients from Nepal would likely use some of the descriptors used by patients from the USA to describe their pain, 1) some differences would emerge in the rates of the most commonly used descriptors used by patients from both countries, 2) there would be some descriptors commonly used by patients from one country but not in the other, and 3) some of the pain quality measures developed and validated in Western countries and population would not be content valid for assessing pain quality in Nepal because of the anticipated differences in how pain is described.
Materials and methods
Overview of study design
The study used an observational design in which 1) participants were asked two open-ended questions (“Participant interview” section) to describe their pain; 2) participant responses to the questions were classified into specific pain-related domains and subdomains; 3) the rates of responses in the domains and subdomains in the current Nepalese sample were compared with the published rates of these responses from patients with chronic pain in the USA; and 4) the content validity of four pain quality measures for assessing pain in Nepal was evaluated.
Participants
The participants in this study (N=101) represented a convenience sample of individuals with chronic musculoskeletal pain from Nepal who were recruited from 1) an urban community (n=80) and 2) a tertiary care hospital that serves patients from rural areas (n=21). Study inclusion criteria included 1) being a citizen of Nepal who can speak Nepali fluently; 2) aged 18 years or older; 3) reporting that they experienced pain for more than half of the days in past 3 months; 4) having pain in muscles or bones or joints for at least 3 months; and 5) reporting an average pain intensity of at least “4” on a 0–10 Numerical Pain Rating Scale, where 0 is “No pain” and 10 is “Maximum pain”. The exclusion criteria included 1) having an acute medical problem that could explain the pain (such as infection or metastatic cancer) and 2) an inability to communicate in Nepali to answer the questions in the interview. The study procedure was approved by the institutional review committee of Kathmandu University School of Medical Sciences, Dhulikhel, Nepal, and the study participants provided signed informed consent (or a witness signed for them if they could not read Nepali).
Participant recruitment
Advertisements about the study were made available in the social media for potential participants with chronic pain living in the community. Ten community participants responded to these advertisements and were found eligible. An additional 70 community participants learned about the study by word of mouth and consented to participate. These 80 community participants were then interviewed by a study research assistant at a location convenient for the participants. Twenty-one participants with chronic musculoskeletal pain were recruited from a population of patients who were treated at the Department of Physiotherapy at Dhulikhel Hospital, Kathmandu University Hospital, for pain. These participants were interviewed at Dhulikhel Hospital. All participants provided signed informed consent. Data collection for this study was performed between September 2015 and January 2016.
Participant interviews
All the participants were interviewed by one of the study investigators (SS) or research assistants supervised by him. Sociodemographic variables collected included age, sex, occupation, religion, and ethnicity. Pain history information collected included the site(s) of pain and cause of pain (such as trauma, diabetes, other diagnosed neurological problems, or arthritis), if known. To address the primary research questions, the participants were then asked two open-ended questions to describe their pain:
- “Please describe your pain to me. What specific words would you use to describe how this pain feels?” and
- “Are there any other words that describe your pain?”
The participants’ responses to these questions were written down verbatim and later coded for analysis (“Pain descriptors coding” section).
Pain descriptors coding
After the study data were collected, one of the study investigators (SS) listed each individual concept (single word or phrase in Nepali) used by each participant to describe their pain in an excel spreadsheet. These words and phrases were then translated to English by SS. A professional translator along with a physician, three nurses, and a subset of patient participants were contacted if the translation required a second opinion. Each of the words or phrases (in English) was then coded by an investigator (SS) into specific global domains (eg, Sensory Quality) and subdomains (eg, Burning) using procedures similar to those used in previous studies.9,10 To make this coding easier, the coding system used began with the global domains and subdomains used by Jensen et al9 in a previous study of English-speaking patients that used similar procedures. For the global domains, these included the domains of Sensory Quality, Spatial Characteristics, Cause/Correlate of Pain, Pain Interference/Effect of Pain, Temporal Characteristics, Pain Affect, Pain Magnitude, and Other.
In addition, and as was done in previous studies, new global domains and subdomains were created as needed (ie, when or if a word or phrase used by a participant could not be classified into an existing domain).9,10 As a result of this process, two new global domains were created that were not used by the US participants in the previous studies.
1) A large number of the Nepalese sample used metaphors to describe their sensory experience; these usually began with the stem, “My pain is like …”. As a result, a new global domain (“Sensory Metaphor”) was created for these responses.
2) A large number of participants used a category of words to describe their pain that were not easily translated into English. These words describe a state that is mostly associated with a sensory experience but does not translate directly into a word that means that sensory experience. Similar types of state words also exist in English but are not usually used to describe pain. For example, the words “Blah” or “Yeechy” are sometimes used to describe a state of malaise. However, while the states described by these two words in English might be associated with the physical experience of fatigue, they are not usually associated with specific sensory pain experiences in the same way that the Nepali words do.
In Nepali, these state words are often associated with painful sensations. For example, jham-jham (or jhum jhum)15 describes a condition that often includes the sensation of feeling a “tingling” pain. Similarly, the kat-kat state often includes the sensation of “achy” pain, that is often made worse by cold, and is sometimes, but not always, associated with a feeling of cold pain that is deep. Chasakka is the word describing a state often associated with a feeling of “piercing” pain, katakka a state similar to kat-kat is associated with an “achy” deep pain, but more variable or intermittent and intense, tanak-tanak is a state associated with a sensation of “swelling” and/or “inflammation” pain, and bhat-bhat is a state associated with a sensation of “burning” pain. The state words, katakka and chasakka, are also associated with having “sudden” pain, although these words do not translate directly into “sudden” in English. Because most of the state words have specific sensory qualities almost always associated with them, as described earlier, we both double-coded most as a Sensory State descriptor and used the Nepali word itself as the label for the subdomain. We also double-coded most of these words as representing the associated Sensory Quality (as having the quality associated with that state, ie, jham-jham was also coded as representing the “Tingling” subdomain). Because kat-kat is often (but importantly not necessarily) associated with a “cold”, “deep”, and “achy” pain, we elected not to double-code kat-kat as indicating any of the Sensory Quality subdomains.
Once SS completed the initial coding of the concepts used by the study participants, a second investigator (MPJ) reviewed these codes. Any questions he had about the classifications were discussed with SS until a consensus agreement was obtained. As we had done when we had questions about the translations, in the event that there were further questions (which occurred primarily with respect to the sensory state words, which required some discussion to determine how best to code) concerning how best to classify a descriptor, SS and MPJ consulted with a professional translator, a physician, a third investigator (AP), and three nurses along with individuals who reported these pain-related states. Discussion continued until a consensus was reached.
Data analysis
We first computed descriptive statistics (mean and standard deviations for continuous variables and rates and percentages for categorical variables) of the demographic and pain history variables to describe the sample. Next, in order to address the first objective of the study (to identify the most common words and phrases used by the sample to describe their pain), we computed the frequency and rates of each global domain and each subdomain. As was done in previous research using samples of patients with chronic pain from the USA,9 we included in these analyses those words and phrases that were mentioned by 3% or more of the sample. To address the second aim of the study (to compare the frequency of descriptors used by the current sample of patients from Nepal with those used by two samples of patients from the USA), we identified and included for comparison with the findings from the present Nepalese sample the descriptors mentioned by at least 3% of the six US samples of individuals with chronic pain, as reported by Jensen et al9 and Lin et al.10 In particular, we were interested to determine if the rate that a subdomain was mentioned by the current Nepalese sample was within the range of the rates reported in the six samples of patients we previously examined. This included samples of patients with spinal cord injury and nociceptive pain, spinal cord injury and neuropathic pain, and multiple sclerosis and chronic pain, reported in Lin et al,10 and samples of patients with chronic low back pain, fibromyalgia, and headache, reported in Jensen et al.9 Finally, to address the third study aim (to evaluate the content validity of pain quality measures developed in Western countries for assessing pain quality in patients from Nepal), we determined the number of the pain quality descriptors mentioned most often by the current study sample which were assessed by the existing pain quality measures. As we had done with respect to this study question in the US samples,9,10 in order to be deemed as assessing the pain quality in question, the measure needs to only include one or more descriptors within a general category. For example, in order to be deemed as providing an assessment of “burning” pain, a measure does not necessarily need to ask the respondent to rate the presence or severity of “burning” pain but could instead ask the respondent to rate the presence or severity of “hot” pain. For the analyses related to the third aim, we limited the pain quality measures examined to five measures that were examined in the previous studies9,10 that both 1) had demonstrated the most content validity in those studies and 2) have been used in research published in the past decade. These included the MPQ,4 the PQAS,7 the PQAS-R,8 the Short-form MPQ (SF-MPQ),6 and the Revised Short-form MPQ-2 (revised SF-MPQ-2).5
Results
Description of the study sample
Descriptive information regarding the study sample is presented in Table 1. As can be seen, the majority of the participants were women (72%) and primarily represented three ethnicities, specifically Newar (53%), Brahmin (25%), and Chettri (15%). Almost half of the sample (49%) had education level <10 years. Most of the participants reported musculoskeletal pain, primarily in the low back and knee.
  | Table 1 Participant descriptive information Abbreviation: SD, standard deviation. |
Frequency of the pain domains and subdomains in the Nepalese sample relative to those used by the US samples
The 101 Nepalese participants in this study mentioned a total of 652 individual concepts when asked to describe their pain. The most common (mentioned by 3% or more of the sample) of these are listed in Table 2, in order of frequency, and classified under their respective global domains. In addition, Table 2 presents the most common (mentioned by 3% or more of at least one US sample) concepts mentioned by the US samples.
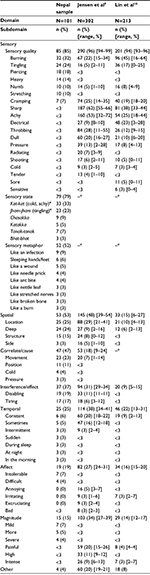  | Table 2 Frequencies of pain domains and subdomains in the current Nepal sample and two US samples Notes: Only descriptors mentioned by 3% (n = 3) or more of the Nepalese sample or at least one of the US samples are listed. *Not coded. #These sensory quality descriptors are often, but not always, associated with these state words. Italics have been used for all “State words”. Reproduced from Lin CP, Kupper AE, Gammaitoni AR, Galer BS, Jensen MP. Frequency of chronic pain descriptors: implications for assessment of pain quality. Eur J Pain. 2011;15(6):628–633. Copyright ©2011.10 Jensen MP, Johnson LE, Gertz KJ, Galer BS, Gammaitoni AR. The words patients use to describe chronic pain: implications for measuring pain quality. Pain. 2013;154(12):2722–2728. Promotional and commercial use of the material in print, digital or mobile device format is prohibited without the permission of the publisher Wolters Kluwer. Please contact [email protected] for further information.9 |
Sensory quality subdomains
As can be seen, the most frequent global domain in the Nepalese sample was the sensory quality of pain, mentioned by 85 (85%) of these participants. This was also the most frequent global domain mentioned by the US samples (range, 93%–99% across the different US samples).9,10 Only four sensory quality descriptors were used by 3% or more of the Nepalese sample and at least one of the US samples: burning, tingling, numb, and cramping. For three of these (burning, tingling, and numb), the rate of use by the Nepalese sample was within the range of that used by the US samples. However, cramping was used less often (7%) by the Nepalese patients than the US patients (range, 14%–35%). Three sensory descriptors were used by >3% of the Nepalese sample and that were not mentioned by 3% or more of any of the US samples: piercing, heavy, and stretching. There were also a fairly large number (12) of descriptors used by at least 3% of one of the US samples that were not mentioned at all, or mentioned only very rarely, by the Nepalese. The most striking differences in the frequency of use were for sharp (US sample range, 33%–66%), achy (US sample range, 18%–72%; but note the use of “kat-kat” by the Nepalese sample in the “Sensory state subdomains” section), throbbing (US sample range, 9%–55%), dull (US sample range, 6%–27%), and electrical (US sample range, 3%–28%). All the other remaining descriptors listed in Table 2 also had at least one US sample who, like the Nepalese, mentioned these <3% of the time (pressure, radiating, shooting, cold, tender, sore, and sensitive).
Sensory state subdomains
The second most common global domain mentioned by the Nepalese sample was the Sensory State domain, mentioned by 79% of the participants. As described previously, this global domain was unique to the Nepali sample; English speakers do not use a similar category of descriptor or phrase to describe their sensory experience of pain, so sensory state subdomains were not mentioned (and therefore not coded) in any of the US samples. However, as described in the “Materials and methods” section, most (all but kat-kat) of these state words were double-coded under the global domains of Sensory Quality and Sensory State (eg, when participants described their pain using jham-jham, this was coded as the Sensory State of jham-jham and the Sensory Quality of Tingling).
If we were to consider every kat-kat word as describing cold and achy pain, then the percent of participants in the current sample who describe their pain as cold and achy would be 33% which is substantially more than the frequency that cold is used in the US samples (range, 2%–5%), but well within the range that achy is used in the US samples (range, 18%–72%).
Sensory metaphor subdomains
Close to half (52%) of the Nepalese sample also used a metaphor to describe their sensory experience of pain. The most common metaphors used were “Like an infection”, “Like sleeping hands/feet”, “Like an ant bite”, and “Like a wound”. While the US samples occasionally described their pain experience using a metaphor (eg, “Like someone is running a spear through me”),10 most of the US sample participants used single-word descriptors when describing their pain. In fact, metaphors were used so infrequently by the US samples that separate global domain and subdomain codes were not developed for classifying these responses in the previous studies.9,10
Other domains and subdomains
While some differences between the Nepalese sample and the US samples were noted for the other domains and subdomains classified, these differences were usually less striking than those observed for the sensory domain descriptors. For the spatial, temporal, affect, and magnitude global domains, the rate of mention by the Nepalese sample fell within the ranges of rates for the US samples. The primary exception to this was for the Correlation/Cause global domain, mentioned by 47% of the Nepalese sample, but only 9%–24% of the six US samples in one of the previous studies9 (the other US study did not code for this global domain). The two most common correlates/causes of pain mentioned by the Nepalese sample were movement (23% mentioned this; in the US sample, the range was 1%–14%) and position (11% mentioned this; <3% mentioned this in the US sample).
With respect to the subdomains within these non-sensory global domains, different words tended to be used by the Nepalese sample (translated into “intolerable” [7%] and “difficult” [4%]) than the US samples (“annoying”, range: <3%–7%; “irritating”, range: 1%–7%; “excruciating”, range: <3%–4%; and “bad”, range: <3%–3%). However, neither the US nor the Nepalese sample tended to use Affect global domain descriptors often (ie, never more often than 7% for any one word). Similarly, the Nepalese tended to use different Magnitude descriptors (eg, translated into “mild”, “more”, and “severe”) than the US samples (eg, “painful” and “intense”), but both the Nepalese and the US samples used at least some Magnitude global domaindescriptors.
Content validity of existing measures for assessing pain quality in patients with chronic pain from Nepal
Table 3 presents the content validity of five measures of pain quality designed for assessing pain in a variety of chronic pain conditions (not just neuropathic pain) for assessing pain quality in patients from Nepal. As can be seen, only one of these measures – the original MPQ, which includes 78 specific pain descriptors – assesses the seven pain qualities mentioned most often by the Nepalese patients as well as a sensory state subdomain commonly associated with an “achy” quality of pain that is a common component of kat-kat, the word used by 33% of the Nepalese sample (Table 2). However, two of the measures – the PQAS and the revised SF-MPQ-2 – assess all but one of the most common sensory quality subdomains used by the Nepalese sample: “stretching” pain. The PQAS-R assesses all but two subdomains (“piercing” and “stretching”), and the SF-MPQ assesses only four of the subdomains.
Discussion
The findings from this study indicate not only overlap but also important differences between how patients with chronic pain from the USA and Nepal describe their pain. They support the idea that directly translated measures of pain quality developed in one country (eg, USA) and/or using a single language (eg, English) should not be assumed to be content valid for use in samples of patients from another country or who speak another language. Therefore, the evaluation of the content validity of such measures should be established for each country or culture in which the measure will be used.11–14
A number of guidelines for translation, adaptation, and validation of patient-reported outcome measures strongly advocate the need of consideration of cultural aspects while performing the translation of a measure and adapting the measure to a different language.11–14 This is because a problem associated with the direct translation of a patient-reported measure to a different language is the possibility that the meaning of the directly translated word or phrase may not be applicable or appropriate for use in that new context. For example, during translation of Oswestry Disability Index to Nepali, an item assessing walking describes distance in terms of miles and yards; distance units not understood by the Nepalese. Thus, during the translation of this item to Nepali, miles and yards were converted to meters so that participants in Nepal could respond appropriately to the items.16 Likewise, during a recent translation of Numerical Rating Scale (NRS) to Nepali by the group (unpublished report), the anchor on the right side “Worst imaginable pain” when translated directly into Nepali sounded odd to native Nepalese. As a result, the anchor was changed to “Maximum pain” in order to make it valid for use in the Nepalese samples.17 However, the process of adapting patient-reported outcome measures to a new language or culture in these examples was completed only after the translation was completed, and the expert team or patients during pretesting of the translated measure learned that the items as directly translated were not necessarily culturally appropriate or valid. The procedure adapted in this study provides a model for developing a valid translated measure concurrently with an evaluation of the content validity of the measure.
In this study, only four pain quality descriptors – five if one considers the Nepali word kat-kat as representing “achy” pain – were common among both the Nepalese and US patients. There were 12 words used by 3% or more of at least one US sample that were rarely, if ever, mentioned by the Nepalese participants, with “sharp”, “throbbing”, and “dull” pain being among the most common of these. In addition, there were three descriptors used by the Nepalese sample – translated as “piercing”, “heavy”, and “stretching” – that were rarely used by any of the US samples. Thus, merely translating one of the common pain quality measures into Nepali and administering such a measure to a Nepalese sample of patients with chronic pain would mean 1) many of the items would not be useful, so the measures would add assessment burden with little benefit and 2) important pain quality descriptors used by the Nepalese patients would not be assessed, that is; a direct translation would not be valid.
The current findings provide some preliminary guidance regarding how to make a Nepali measure of pain quality more valid and efficient. Specifically, the findings suggest that such a measure needs only to measure “burning”, “tingling”, “piercing”, “heavy”, “numb”, “stretching”, and “cramping” qualities. Such a measure could also be made even more valid by including items assessing kat-kat, jham-jham, chasakka, katakka, tanak-tanak, and bhat-bhat pain. If kat-kat pain is not included, then the Nepali measure should also include an item asking about the severity of achy pain; however, this would be difficult to ask in Nepali using any other words other than kat-kat (or kar-kar), because the Nepalese rarely directly use the Nepali word that is translated as “achy” to describe any pain condition. Thus, if a study involves an international (cross-cultural) multi-site design that includes samples from both the USA and Nepal, then investigators might consider using either the PQAS or the SF-MPQ-2, adding an item that assesses “stretching” pain (tankeko jasto dukhai, used by 10% of the Nepalese sample) and adding kat-kat to ensure that these qualities are covered.
Another interesting (and unexpected) cross-cultural difference that emerged in this study was the fact that the Nepalese participants used metaphors to describe their pain much more often than US patients do. This finding suggests the possibility that many people in Nepal may think about pain differently than people in the USA. Specifically, they appear to be more likely to think about their pain metaphorically by comparing it to experiences that they might have experienced or imagined themselves as experiencing, rather than merely as a sensation that can be described using single-word descriptors. For example, one of the participants described his pain “Like cancer pain”, even though he had never been diagnosed with cancer, although he may have known someone who had cancer. Of course, individuals from all over the world, including individuals in the USA, can and do use metaphors to describe their pain. However, the between-country difference in frequency of this that we observed is striking.
Whether this difference has important clinical implications remains to be seen, but the finding suggests the possibility that this should be explored further. For example, there are chronic pain treatments that involve the use of clinician-provided metaphors for helping patients alter their thinking about pain, including hypnotic procedures,18–24 and Explain Pain.25–28 It would be interesting to see if patients from Nepal respond more to such treatments than treatments that have been shown to be effective in Western populations, but that do not make as much of a use of metaphors, for example, cognitive behavioral therapy.29–33
We found fewer differences between the current Nepalese sample and the US samples we previously studied for the other global domains and subdomains examined. For the most part, patients from both countries described their pain similarly in terms of its spatial characteristics, its interference, its temporal characteristics, its affective characteristics, and its magnitude. Perhaps the primary difference with respect to non-sensory global domains is the greater frequency with which the Nepalese samples mentioned the correlates and causes of their pain. This suggests the possibility that individuals with chronic pain from Nepal might be particularly responsive to treatments that explain the cause of their condition in a way that both makes sense to them and allows them to function well, despite pain.26–28 This possibility should be explored. In any case, and as a group, the findings suggest both that 1) measures of these other (non-sensory quality) domains should be considered when researchers and clinicians wish to obtain a thorough assessment of pain and 2) perhaps measures of these domains developed using patients from one country or culture may be more likely to be content valid for assessing these domains in different countries or cultures than pain quality measures are.
There are a number of limitations of this study that should be considered when interpreting the results. 1) To our knowledge, this is the first time that patients with chronic pain in Nepal were asked to describe their pain, and their responses were coded by a single investigator (SS) to determine the rates with which different domains were mentioned. It would have been ideal if two independent researchers had translated the participants’ responses in order to be able to evaluate the reliability of the translation. 2) The majority of the study participants came from the community and were not specifically seeking pain treatment, even though they had to rate their usual pain intensity as at least 4 of 10 on a 0–10 NRS. The findings might have been different if more participants had been recruited from the hospital who were seeking treatment for pain or who might have had more severe pain. Therefore, the current findings should be replicated in additional samples of patients from Nepal to determine their reliability. 3) The sample size, while adequate for obtaining good estimates of the rates that different pain domains are used for those domains that are fairly common, might be considered low for estimating the rates of descriptors that are less commonly used. Thus, subdomains that were mentioned only twice in the sample (2%) might in fact be used more (≥3%) in the population. This is another reason for replicating the current findings in additional samples of patients; ideally, samples that are even larger than the sample size used for this study. 4) We did not compare the findings of this study to data from a sample from the USA collected at the same time as the data collected here. Instead, we compared the words used by individuals with chronic pain in the Nepalese sample with the words used by the participants in the studies that were completed in 2011 and 2013.9,10 Although it seems unlikely that there would be systematic differences in how individuals from the USA describe their pain after 3 or 5 years have passed, we cannot be certain of this. However, to help address this issue, we used the same methods here as were used in the previous studies in order to make the results obtained as comparable as possible. Finally, it should be noted that the US and Nepalese samples differed on a number of important variables not specifically related only to culture. For example, people in Nepal earn much less and have much less education, on average, than people from the USA, which may influence the expression of pain. Moreover, even though one of the US samples had primarily musculoskeletal pain (specifically, low back pain), as did the current Nepalese sample, the US studies also included individuals with primarily neuropathic pain and other pain conditions (eg, spinal cord injury and neuropathic pain, and multiple sclerosis and chronic pain, fibromyalgia, and headache). These other non-cultural differences in the US and Nepalese samples may have explained some of the differences found in the rates of descriptors chosen – although we think it unlikely that they explain the very high rates of metaphors used in the Nepalese sample relative to the US sample, as well as the use of state descriptors in the Nepalese sample only, given the lack of equivalent state words in the English language. Still, research that directly compares individuals from the USA who match a Nepalese sample in terms of demographics (education level, salary) and pain type would help to identify those differences that are primarily due to cultural differences.
Conclusion
Despite the limitations of this study, the findings clearly indicate that pain quality measures developed using samples of patients from only one country or perhaps even from only one culture (eg, western cultures or eastern cultures only) are not necessarily content valid for assessing pain quality in other countries or other cultures. It is also possible that this might also be true for measuring other important pain-related domains. This points to the need to evaluate the content validity of such measures in different countries and cultures before using them in that culture and then adapting the measure as needed. The findings from this study provide a model for how such validity testing could be done, as well as providing empirical guidance for how existing measures of pain quality could be adapted to increase their validity for use in the Nepalese samples.
Acknowledgments
This project was supported in part by a Developing Countries Collaborative Research Grant from the International Association for the Study of Pain awarded to MPJ and SS in 2015. The authors would like to thank the physiotherapy students at Kathmandu University School of Medical Sciences for their help in subject recruitment and data collection for this study.
Author contributions
SS – conception, study design, data collection, coding of descriptors, data analysis, manuscript writing, and final revision. AP – data collection, coding of descriptors, data analysis, and final approval of manuscript. MPJ – conception, study design, coding of descriptors, data analysis, manuscript writing, and final revision.
Disclosure
One of the authors (MPJ) is a co-developer of two of the measures discussed in this article (the Pain Quality Assessment Scale and Revised Pain Quality Assessment Scale) and receives royalties for sponsored use of these measures. The other authors (SS and AP) report no conflicts of interest in this work.
References
Henschke N, Kamper SJ, Maher CG. The epidemiology and economic consequences of pain. Mayo Clin Proc. 2015;90(1):139–147. | ||
Jensen MP, Turk DC. Contributions of psychology to the understanding and treatment of people with chronic pain: why it matters to ALL psychologists. Am Psychol. 2014;69(2):105–118. | ||
Jensen MP, Karoly P. Handbook of Pain Assessment. 3rd edition ed. New York: Guilford Press; 2011. | ||
Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1(3):277–299. | ||
Dworkin RH, Turk DC, Revicki DA, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain. 2009;144(1–2):35–42. | ||
Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. | ||
Jensen MP, Gammaitoni AR, Olaleye DO, Oleka N, Nalamachu SR, Galer BS. The pain quality assessment scale: assessment of pain quality in carpal tunnel syndrome. J Pain. 2006;7(11):823–832. | ||
Jensen MP, Lin CP, Kupper AE, Galer BS, Gammaitoni AR. Cognitive testing and revision of the pain quality assessment scale. Clin J Pain. 2013;29(5):400–410. | ||
Jensen MP, Johnson LE, Gertz KJ, Galer BS, Gammaitoni AR. The words patients use to describe chronic pain: implications for measuring pain quality. Pain. 2013;154(12):2722–2728. | ||
Lin CP, Kupper AE, Gammaitoni AR, Galer BS, Jensen MP. Frequency of chronic pain descriptors: implications for assessment of pain quality. Eur J Pain. 2011;15(6):628–633. | ||
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000;25(24):3186–3191. | ||
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–1432. | ||
Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8(2):94–104. | ||
Eremenco SL, Cella D, Arnold BJ. A comprehensive method for the translation and cross-cultural validation of health status questionnaires. Eval Health Prof. 2005;28(2):212–232. | ||
Kohrt BA, Schreiber SS. Jhum-jhum: neuropsychiatric symptoms in a Nepali village. Lancet. 1999;353(9158):1070. | ||
Acharya RS, Al-Oraibi S, Adhikari SP, Parajuli N, Limbu H, Enezi FA. Validation in the cross-cultural adaptation of the Nepali Version of the Oswestry Disability Index. Indian J Physiother Occup Ther. 2014;8:158–163. | ||
Sharma S, Palanchoke J, Reed D, Abbott HJ. Translation, Cross-Cultural Adaptation and Psychometric Properties of the Nepali Versions of Numerical Pain Rating Scale and Global Rating of Change. Dhulikhel: Kathmandu University School of Medical Sciences; 2016. | ||
Jensen MP, Adachi T, Tome-Pires C, Lee J, Osman ZJ, Miro J. Mechanisms of hypnosis: toward the development of a biopsychosocial model. Int J Clin Exp Hypn. 2015;63(1):34–75. | ||
Tan G, Rintala DH, Jensen MP, Fukui T, Smith D, Williams W. A randomized controlled trial of hypnosis compared with biofeedback for adults with chronic low back pain. Eur J Pain. 2015;19(2):271–280. | ||
Jensen MP. Hypnosis for chronic pain management: a new hope. Pain. 2009;146(3):235–237. | ||
Jensen MP, Barber J, Romano JM, et al. Effects of self-hypnosis training and EMG biofeedback relaxation training on chronic pain in persons with spinal-cord injury. Int J Clin Exp Hypn. 2009;57(3):239–268. | ||
Jensen MP, Barber J, Romano JM, et al. A comparison of self-hypnosis versus progressive muscle relaxation in patients with multiple sclerosis and chronic pain. Int J Clin Exp Hypn. 2009;57(2):198–221. | ||
Jensen MP, Ehde DM, Gertz KJ, et al. Effects of self-hypnosis training and cognitive restructuring on daily pain intensity and catastrophizing in individuals with multiple sclerosis and chronic pain. Int J Clin Exp Hypn. 2011;59(1):45–63. | ||
Patterson DR, Jensen MP. Hypnosis and clinical pain. Psychol Bull. 2003;129(4):495–521. | ||
Louw A, Puentedura EJ, Zimney K, Schmidt S. Know pain, know gain? A perspective on pain neuroscience education in physical therapy. J Orthop Sports Phys Ther. 2016;46(3):131–134. | ||
Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–813. | ||
Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–330. | ||
Moseley L. Combined physiotherapy and education is efficacious for chronic low back pain. Aust J Physiother. 2002;48(4):297–302. | ||
Archer KR, Devin CJ, Vanston SW, et al. Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J Pain. 2016;17(1):76–89. | ||
Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153–166. | ||
Finan PH, Buenaver LF, Coryell VT, Smith MT. Cognitive-behavioral therapy for comorbid insomnia and chronic pain. Sleep Med Clin. 2014;9(2):261–274. | ||
Gatchel RJ, Rollings KH. Evidence-informed management of chronic low back pain with cognitive behavioral therapy. Spine J. 2008;8(1):40–44. | ||
Kerns RD, Otis JD, Marcus KS. Cognitive-behavioral therapy for chronic pain in the elderly. Clin Geriatr Med. 2001;17(3):503–523. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

