Back to Journals » Risk Management and Healthcare Policy » Volume 15
Which Volunteering Settings Do Medical Students Prefer During a Novel Respiratory Virus Pandemic? A Cross-Sectional Study of Multiple Colleges in Central Saudi Arabia During the COVID-19 Pandemic
Authors AlSaif HI , Alessa MM, Alajlan AH, Alrshid AI , Aljarbou AF, Alqahtani AA, Aljumah MI, Alrshid MI, Aleisa AI, Aloufi AM, Alsaad SM
Received 13 January 2022
Accepted for publication 29 April 2022
Published 11 May 2022 Volume 2022:15 Pages 983—996
DOI https://doi.org/10.2147/RMHP.S352210
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Kyriakos Souliotis
Haytham I AlSaif,1 Mohammed M Alessa,2 Ahmed H Alajlan,2 Abdulelah I Alrshid,2 Abdulaziz F Aljarbou,2 Awadh A Alqahtani,2 Mohammad I Aljumah,2 Mansour I Alrshid,3 Aljoharah I Aleisa,4 Abdulrahman M Aloufi,5 Saad M Alsaad1
1Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 2College of Medicine, King Saud University, Riyadh, Saudi Arabia; 3College of Medicine, Imam Muhammed Ibn Saud Islamic University, Riyadh, Saudi Arabia; 4College of Medicine, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia; 5College of Medicine, Almaarefa University, Riyadh, Saudi Arabia
Correspondence: Haytham I AlSaif, Department of Family and Community Medicine, College of Medicine, King Saud University, P.O. Box 2925, Ext. 34, Riyadh, 11461, Saudi Arabia, Tel +966 114670836, Email [email protected]
Purpose: Novel respiratory virus outbreaks are a recurring public health concern. Volunteering medical students can be a valuable asset during such times. This study investigated the willingness of medical students to volunteer during the coronavirus disease of 2019 (COVID-19) pandemic and the barriers to doing so, considering the possibility of exposure to COVID-19 and mode of contact.
Patients and methods: This cross-sectional study was conducted using a self-administered online questionnaire adapted from the literature. The questionnaire comprised four parts: demographic variables, COVID-19-related variables, willingness scale, and barrier scale. The target population was medical students at four different colleges in Riyadh, Saudi Arabia.
Results: A total of 802 students participated in the study. A small proportion of students (10.6%) were willing to participate in volunteering activities that could involve contact with patients with COVID-19 as compared to other settings (39.4– 43.4%). More than one-quarter of students (26.8%) had risk factors for severe COVID-19. The main barrier to volunteering was the concern of transmitting the infection to family members (76.8%). Registration to receive the COVID-19 vaccine was positively associated with more willingness to volunteer (β=0.17, p < 0.001), whereas residing in a household with an elderly person was negatively associated (β=− 0.13, p < 0.001). Female sex was positively associated with higher barrier score (β=0.12, p < 0.001).
Conclusion: Medical students were more willing to volunteer in activities that did not involve direct contact with patients with COVID-19. A considerable proportion of participants had risk factors for severe illness. Sharing a household with an elderly person or child was associated with lower willingness to volunteer. Organizers of volunteering activities should offer various volunteering options considering the risk of infection; and be mindful of barriers to volunteering, especially risk factors for severe illness and eldercare and childcare responsibilities.
Keywords: medical students, volunteerism, health workforce, disaster, pandemic, COVID-19
Introduction
Volunteering can be defined as “any activity in which time is given freely to benefit another person, group, or organization”.1 Volunteers, especially medical students, are an asset for healthcare systems and the community under normal circumstances, as well as during pandemics and other public health emergencies.2–-5 Volunteering is a professionally and morally rewarding experience for medical students as it fosters their professional identity.6 Medical students are motivated by multiple factors, such as altruism, community service, sense of duty, and professional development.7–10
Students’ volunteering options include a wide array of activities that can involve direct contact with patients, such as patient care and clinical assistance; contact with persons in the community setting outside healthcare facilities through food and medicine delivery; and activities that can be performed without direct contact, such as attending phone helplines and raising awareness through social media.5,11–13 Nevertheless, multiple barriers to volunteering in general, including a negative impact on academic performance and lack of confidence and necessary skills, exist.5 Some barriers, such as concerns over personal or family safety, apply specifically to public health emergencies, especially with the risk of respiratory transmission.5,14
Since March 2020, the world has been in a pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a novel respiratory virus and the causative agent of COVID-19, which spreads rapidly and is associated with significant morbidity and mortality.15,16 Most countries have implemented restrictions, including movement restriction, mask use, and social distancing, to mitigate transmission of the virus.17 In Saudi Arabia, similar measures were implemented to control the transmission.18 Additionally, volunteers were an essential part of the healthcare workforce to face the increasing demand during the pandemic.19 For example, volunteers answered 20% of the calls to the nationwide hotline for medical inquiries (937) during the pandemic.20 However, the concern of infection and imposed restrictions and precautions may discourage and limit volunteering by medical students in traditional settings requiring direct contact. Therefore, virtual platforms, such as telehealth and health promotion through social media, have been suggested as alternative venues for medical students to volunteer during the COVID-19 pandemic.5,21
Several demographic factors specific to Middle Eastern countries are additional barriers to volunteering by medical students during the pandemic. For instance, the average size of households (≥5) is larger than that of other countries, except those in Africa.22 Therefore, medical students often live with elderly individuals or children. Additionally, Middle Eastern countries have an increasing population of elderly individuals,23 who are particularly vulnerable to severe COVID-19 disease.24
Although multiple studies have explored the willingness of medical students to engage in volunteering activities and the barriers to doing so before and during the COVID-19 pandemic,5,8,25–30 they have not considered different settings and modes of contact that could lead to exposure to COVID-19. Additionally, because of cultural and demographic particularities of Middle Eastern countries, specific barriers to volunteering among medical students in this region should be identified to optimize this resource both generally and during public health emergencies for the benefit of the healthcare system, patients, and community. Furthermore, demographic factors that are associated with increased willingness or barriers to volunteer should be explored. This multicenter study investigated these factors using an online questionnaire targeting medical students in Riyadh, Saudi Arabia.
Methods
Study Design and Setting
This cross-sectional study used a self-administered online questionnaire adapted from the literature,5,14,24 targeting medical students at four of the eight colleges of medicine located in Riyadh, the capital of the Kingdom of Saudi Arabia. These are the Colleges of Medicine at King Saud University (KSU), Imam Muhammad Ibn Saud Islamic University (IMISIU), the women-only Princess Nourah Bint Abdulrahman University (PNU), and AlMaarefa University (MU). KSU, IMISIU, and PNU are public universities, whereas MU is a private university. First to fifth year medical students were included in the study, whereas foundation year students, interns, and withdrawn students were excluded. A total of 3609 medical students attended the aforementioned colleges (KSU=1466, IMISIU=1005, MU=746, and PNU=392). Of the 3609 medical students, 1839 and 1770 students were female and male students, respectively. Among them, 1570 students were in the basic sciences stage, 717 students were in the preclinical stage, and 1322 students were in the clinical stage. The minimum sample size required to detect a 57.4% proportion of medical students willing to volunteer with a 95% confidence level and a 5% margin of error was determined as 341 students.25 Responses were collected during January and February 2021. At the time, due to COVID-19 precautions, lectures were provided online at KSU and PNU. However, at IMISIU, basic sciences level lectures were a hybrid of the online and in-person modes. For the clinical level at MU, lectures were taught in-person on campus. In all universities, practical sessions were conducted with limited numbers in laboratories and clinical settings.
Study Instrument
The questionnaire was divided into four parts. The first part consisted of the following demographic variables: sex, marital status, grade point average (GPA), study year, persons with whom participants live, and elderly and children in the household. GPA was categorized as excellent (≥ 90%), very good (90–75%), good (75–55%), and pass (<55%). The number of study years was categorized as stages based on the type of courses in that stage: first and second year, basic science stage; third year, preclinical stage; and fourth and fifth years, clinical stage. Elderly persons were defined as those aged ≥65 years. The second part included questions related to COVID-19, such as history of close contact with infected patients or confirmed personal infection, COVID-19 vaccination registration status, and presence of risk factors for severe COVID-19 infection. Risk factors for severe COVID-19 infection included the following: Asthma or any other chronic respiratory diseases, obesity, smoking, cardiovascular diseases including hypertension, recent admission to the hospital, pregnancy, and sickle cell disease or thalassemia.24,31 Obesity was defined as having a body mass index (BMI) ≥30 kg/m2, and recent admission was defined as being admitted to a hospital in the past 6 months.
The third part of the questionnaire was a 4-item willingness scale developed to assess students’ willingness to volunteer in different settings based on the possibility of contact with patients with COVID-19, site of volunteering (inside healthcare facilities or in the community), and the nature of contact with persons (direct or distant). Willingness to participate in these settings was measured using a 5-point Likert scale (not willing=0, somewhat not willing=1, undecided=2, somewhat willing=3, willing=4). The fourth part was the barrier scale consisting of 11 barriers adapted from the literature.5,14 Agreement with these barriers was measured on a 5-point Likert scale (strongly disagree=0, disagree=1, neutral=2, agree=3, strongly agree=4). Participants were required to complete all items, except the optional items on elderly persons and children in the household, to be able to submit the questionnaire.
A pilot study to test the questionnaire was conducted with 30 first-year medical students to ensure that the questions were comprehensible, even to the most junior students. No issues were reported regarding questionnaire access, content, and time required for completion, which averaged 5 minutes.
Data Collection
KSU, IMISIU, and MU students were classified into 10 groups based on sex and study year, whereas PNU students were classified into five groups. Data collectors contacted group leaders to send the invitation link to a Google Forms page (Google, Mountain View, CA, USA), containing the informed consent form and questionnaire. Links were sent to student electronic messaging groups where students receive course announcements and information about extracurricular activities, such as volunteering. The initial invitation was followed with two weekly reminders to encourage participation. If two or more responses were identical in responses to all items and had the same time stamp, they were labelled as duplicates.
Statistical Analysis
Spreadsheets of questionnaire responses were imported from Google Forms and coded using Excel v16.0 (Microsoft, Redmond, WA, USA). The coded data were analyzed using SPSS v24.0 (IBM, Armonk, NY, USA). Descriptive statistics (mean, standard deviation, frequencies, and percentages) were used to describe quantitative and categorical variables. Total willingness scale score was calculated by summing the scores of the four items pertaining to willingness to volunteer in different settings (minimum=0, maximum=16). A total barrier scale score was calculated by summing the scores of 11 barrier items (minimum=0, maximum=44). Cronbach’s alpha was used to measure the internal consistency of willingness and barrier scales. Differences in mean willingness and barrier scores between categories of demographic variables were assessed using the independent samples t test or one-way analysis of variance. Associations between willingness or barriers scores and continuous or ordinal variables were evaluated with Pearson’s correlation and Spearman correlation, respectively. Multiple linear regression was used to assess the association between demographic and COVID-19-related variable and willingness and barrier scale scores. The stepwise method applied a 0.05 probability of F for entry and 0.1 for removal, and missing cases were excluded pairwise. Associations between willingness to volunteer in different settings as a dependent variable and level of agreement with barriers were determined using Somers’ d. A p-value <0.05 and 95% confidence interval were used to report the statistical significance and precision of the results, respectively.
Ethical Considerations
Ethics approval (number E-21-5669) was obtained from the institutional review board at KSU College of Medicine. Participation was voluntary, and data were collected for research purposes only. The questionnaire page contained the informed consent form at the top to be viewed prior to voluntary participation. It included the purpose of the study, assurance that responses would be treated confidentially, and the contact information, if the participant had further inquiries. Self-identifying information, such as name, university number, phone number, and email, were not collected. Data were stored on the principal investigator’s computer, which was password-protected.
Results
Participant Characteristics
Overall, 805 responses (22.3% response rate) were received; three of these responses were duplicates. Therefore, 802 responses were included in the analysis. The response rates varied among different colleges; 365 students from KSU (24.9%), 156 students from IMISIU (15.5%), 149 students from PNU (38%), and 130 students from MU (17.4%) provided responses. The response rate was slightly higher for males (24%) than for females (20.5%). In addition, preclinical stage students had the highest response rate (36.1%), followed by basic sciences students (20.4%), and finally the clinical stage students (16.9%). Almost all (98.6%) of the participants were single, and most (92.4%) participants were living with their families. More than one-quarter of participants (28.1%) were living with elderly persons, and 53.1% were living in a household with children. The highest proportion of participants was in the basic sciences stage (39.9%); 53.4% had an excellent GPA and 58.7% had previously volunteered at least once. Table 1 shows the demographic characteristics of the study participants.
 |
Table 1 Sociodemographic Characteristics of the Study Participants (n=802) |
COVID-19-Relevant Characteristics
One-third of participants (33.5%) had a history of close contact with a patient with COVID-19; 10.5% were previously diagnosed with COVID-19, and 62.3% were not registered to be vaccinated (Table 2). More than one-quarter (26.8%) of participants had risk factors for severe COVID-19 disease with chronic respiratory illness, obesity, and smoking being the most prevalent (Figure 1).
 |
Table 2 Frequency of COVID-19–Related Characteristics of Study Participants (n=802) |
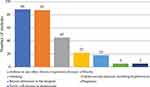 |
Figure 1 Bar chart of risk factors for severe COVID-19 disease (n=215). |
Willingness to Volunteer in Different Settings
Only 10.6% of students were willing to volunteer in activities that could involve direct contact with suspected or confirmed cases of COVID-19; higher proportions of students were willing to volunteer in other settings (39.4–43.4%) (Figure 2). The willingness scale showed acceptable internal consistency with a Cronbach’s alpha of 0.735. The mean willingness scale score was 9.32±4.3 (58.3% of the maximum willingness scale score), and the median score was 10 (interquartile range=7–12). Willingness scale means differed significantly across categories of the following demographic variables: sex, living with elderly persons or children, study stage, GPA, and number of previous volunteering activities (Table 1). Mean willingness scale scores differed significantly across the following COVID-19-related variables: history of close contact with COVID-19 patients, COVID-19 vaccine registration status, and having risk factors for severe COVID-19 disease (Table 2). Multiple linear regression model showed that living with elderly persons or children and having a risk factor for severe COVID-19 disease were significantly associated with lower total willingness scale score. Additionally, a higher GPA, higher number of previous volunteering activities, history of a close contact with a patient with COVID-19, and registration to receive the COVID-19 vaccine were significantly associated with higher total willingness scale scores (Table 3).
 |
Table 3 Multiple Linear Regression Results of Significant Demographic Characteristics for Total Willingness Scale Score |
 |
Figure 2 Bar charts of students’ willingness to volunteer in different settings (n=802). |
Barriers to Volunteering
The barrier scale showed good internal consistency with a Cronbach’s alpha of 0.795. The mean barrier scale score was 22.31±8.2 (50.7% of the maximum barrier scale score) and the median barrier score was 22 (interquartile range=17–28). The major barrier was the concern of transmitting COVID-19 to other family members (76.8%), followed by discouragement by their parents or other family members (42.8%) and increased levels of stress (42%). Figure 3 shows students’ agreement with the effect of different barriers on their willingness to volunteer. Bivariate analysis of demographic variables and barrier scale scores revealed significant differences among means of the following variables: sex, study stage, and number of previous volunteering activities (Table 1). Multiple linear regression analysis showed that female sex was significantly associated with higher barrier scale score, whereas higher number of previous volunteering activities was significantly associated with lower barrier scale score (Table 4). When the mean score for each barrier was tested for differences between females and males, the following barriers had a significantly higher mean score among females than males: acquiring the infection, inadequate pre-volunteering training, insufficient personal protective equipment (PPE), and inadequate supervision during training. However, males had a higher mean score for eldercare responsibility than females (Table 5).
 |
Table 4 Multiple Linear Regression Results of Significant Demographic Characteristics for Total Barrier Scale Score |
 |
Table 5 Mean Barrier Scores for the Study Participants (n=802) |
 |
Figure 3 Bar charts of students’ agreement with the effect of different barriers on their willingness to volunteer (n=802). |
Association Between Barriers to Volunteering and Willingness to Volunteer in Different Settings
A weak negative correlation was identified between students’ concern of acquiring COVID-19 and their willingness to volunteer in activities that could involve direct contact with patients with COVID-19 in healthcare facilities (d=−0.168, p <0.001), with a smaller correlation for activities that could involve direct contact with patients without COVID-19 (d=−0.083, p=0.006). However, no significant correlation was identified for activities that could involve direct contact with the community (d=−0.036, p=0.211). A very weak positive correlation with activities that do not involve direct contact with persons was recorded (d=0.087, p=0.004). Additionally, a weak positive correlation existed between students’ concern of transmitting COVID-19 to other family members and their willingness to volunteer in the three other settings that may not involve direct contact with patients with COVID-19 (d=0.18–0.272, p <0.001). A weak positive correlation was recorded between discouragement by parents or other family members and students’ willingness to volunteer in activities that do not involve direct contact with persons (d=0.166, p <0.001) (Table 6).
 |
Table 6 Association Between Barriers and Willingness to Volunteer in Different Settings (n=802) |
Discussion
Considerable differences existed in students’ willingness to volunteer in activities that could involve contact with patients with COVID-19 compared to other settings (10.6% vs 39.4–43.4%). Fear of being infected may partly explain this difference, as there was a weak negative correlation between this barrier and willingness to volunteer in activities that could involve contact with patients with COVID-19. This explanation is supported by the fact that willingness to volunteer in other settings was comparable despite differences in the location (healthcare facility or community) and mode of contact (direct or distant). Moreover, this is consistent with the previous finding that personal health and safety concerns were an especially large barrier to volunteering when respiratory pathogens were involved.5,8,9,28,29 Registration to receive the COVID-19 vaccine had the highest positive association with willingness to volunteer. Prosocial motives might explain the previous finding, as research showed that it is associated with volunteerism and vaccination intentions.32,33
Although we found that female sex was associated with higher barrier score, no difference existed between sexes with respect to willingness to volunteer, consistent with previous findings.26 However, most studies have reported less willingness to volunteer among females than males.29,30,34 This finding can be explained by the fact that female students in our study had higher agreement with the following concerns as barriers: acquiring COVID-19 infection, inadequate pre-volunteering training, insufficient PPE, and inadequate supervision during training.
Eldercare and childcare were previously reported as barriers for healthcare workers to respond during disasters.14 However, an important finding of our study was that even living in a household with elderly persons or children reduced students’ willingness to volunteer. First, students had less willingness because of the concern of transmitting COVID-19 to these family members who were perceived as being more vulnerable to severe illness.28,29,35 Second, they perceived that volunteering could negatively affect the care that they would be able to provide to these family members. Our results diverge from those of a study of Indonesian medical students that found no difference in willingness to volunteer between those who lived in a household with children or elderly persons and those who did not.29 This discrepancy may be attributable to a difference in the assessment of willingness, which was based on a single item in the Indonesian study, as compared to four items covering different settings and the possibility of contact with patients with COVID-19 in our study.
Family opinion is an important determinant in students’ decision to volunteer. Among Polish medical students, 59.2% indicated that they consulted their parents before volunteering.8 Likewise, 43.2% of students in our study agreed that discouragement by parents or other family members was a barrier. In addition, concern of increased stress was reported by 42% of students in our study as a barrier to volunteering. In a large study from Brazil (10,433 students), lower proportion of students (34.6%) agreed that they felt stressed at the hospital during the pandemic.9 Ensuring access to psychological support is important for the volunteers. For instance, in a study on volunteering health sciences students, 61.4% of students reported that they did not have access to supportive psychological services when needed.10
Supervision during volunteering has been reported in multiple studies.9,27 Less than half (46.8%) of the Brazilian medical students agreed that the supervision they received during practice was good.9 Michno et al27 surveyed medical students from multiple countries and found that an inadequate level of supervision was a concern for less than two-thirds (60.4%) of students. However, this was the case for less than one-third (30.1%) of students in our study. Differences in item phrasing might have contributed to this variance, as Michno et al added to the item the inability to safely perform clinical duty as a consequence of inadequate supervision.27
Distinction between the first and subsequent waves of COVID-19 regarding extracurricular participation in clinical and community work by medical students has been a matter of debate.36 During the first wave, medical students had more free time, which was not the case in subsequent waves when clinical training had fully resumed.36 Therefore, volunteering during times of full academic requirements in a setting of public health emergency may excessively burden medical students and their essential role as learners, which is typically measured by grades.36 Our study was conducted during the beginning of the second wave in Saudi Arabia,37 and 40.8% of medical students agreed that a negative effect on their grades is a concern when they consider volunteering, which is consistent with the aforementioned view point.
Although medical students may be assumed to have few risk factors for severe COVID-19 illness, our data revealed the opposite, with one-quarter of participants having at least one risk factor. Few medical students (10.6%) had chronic medical illnesses in an international study.27 However, they did not inquire about obesity and smoking, which might explain the lower proportion. In our study, having a risk factor for severe illness was associated with lower willingness to volunteer. This association was observed for activities involving direct contact with patients with and without COVID-19 but not for activities in the community or that were performed at a distance. Having a risk factor for severe illness could explain the lower willingness to volunteer in settings with higher probability of COVID-19 transmission.
Strengths and Limitations
This study involved medical students from multiple colleges with a large sample size and comparable response rate between sexes. Additionally, it assessed students’ willingness to volunteer in four different settings during a local and global surge of the COVID-19 pandemic (Winter 2021). However, the study was limited by convenience sampling, low response rate, variability of response rate based on university attended and study stage, and the fact that data were obtained through self-report and did not actually measure volunteering activities.
Conclusion
During the COVID-19 pandemic, medical students were more willing to volunteer in activities that do not involve direct contact with probable patients with COVID-19. Notably, medical students are not without risk factors of severe illness. No significant difference in willingness existed between sexes; however, female students indicated higher agreement with barriers to volunteering. Sharing a household with and an elderly person or child was associated with lower willingness to volunteer. Recommendations for organizers of volunteering activities include considering various volunteering options in light of the risk of infection, paying attention to barriers to volunteering, especially having risk factors for severe illness, and responsibility for eldercare and childcare.
Abbreviations
BMI, body mass index; COVID-19, coronavirus disease of 2019; GPA, grade point average; IMISIU, Imam Muhammad Ibn Saud Islamic University; IQR, interquartile range; KSU, King Saud University; MU, AlMaarefa University; PNU, Princess Nourah Bint Abdulrahman University; PPE, personal protective equipment; SARS-Cov-2, severe acute respiratory syndrome coronavirus 2.
Acknowledgments
The authors thank the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Saudi Arabia for their support. Also, we thank the participating medical students, the Deanship of Scientific Research and the Researcher Support and Services Unit at King Saud University for their technical support, the peer reviewers for their valuable comments and suggestions, and the Charlesworth Group (www.cwauthors.com) for English language and graph editing services.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wilson J. Volunteering. Annu Rev Sociol. 2000;26(1):215–240. doi:10.1146/annurev.soc.26.1.215
2. US Centers for Disease Control and Prevention. QuickStats: percentage of adults who volunteered or worked in a hospital, Medical Clinic, Doctor’s Office, Dentist’s Office, nursing home, or some other health care facility, by sex, race, and hispanic origin — national health interview survey, United States, 2016–2018. MMWR Morb Mortal Wkly Rep. 2020;69(28):941. doi:10.15585/mmwr.mm6928a7.
3. Hunter P, Zacharias K, Wagner M, et al. Student volunteers at mass H1N1 vaccination clinics: addressing public health emergencies by integrating service learning within an incident command structure. In:
4. Buckland R. Medical student volunteering during COVID-19: lessons for future interprofessional practice. J Interprof Care. 2020;34(5):679–681. doi:10.1080/13561820.2020.1822790
5. Martin A, Blom IM, Whyatt G, et al. A rapid systematic review exploring the involvement of medical students in pandemics and other global health emergencies. Disaster Med Public Health Prep. 2020:1–13. doi:10.1017/dmp.2020.315
6. Beck J, Chretien K, Kind T. Professional identity development through service learning: a qualitative study of first-year medical students volunteering at a medical specialty camp. Clin Pediatr. 2015;54(13):1276–1282. doi:10.1177/0009922815571108
7. Gouda P, Kirk A, Sweeney AM, et al. Attitudes of medical students toward volunteering in emergency situations. Disaster Med Public Health Prep. 2020;14(3):308–311. doi:10.1017/dmp.2019.81
8. Domaradzki J, Walkowiak D. Medical students’ voluntary service during the COVID-19 pandemic in Poland. Front Public Health. 2021;9:618608.
9. Tempski P, Arantes-Costa FM, Kobayasi R, et al. Medical students’ perceptions and motivations during the COVID-19 pandemic. PLoS One. 2021;16(3):e0248627. doi:10.1371/journal.pone.0248627
10. Chawłowska E, Staszewski R, Lipiak A, et al. Student volunteering as a solution for undergraduate health professions education: lessons from the COVID-19 pandemic. Front Public Health. 2021;8:633888. doi:10.3389/fpubh.2020.633888
11. Johns Hopkins Medicine. Johns Hopkins medical students mobilize to volunteer for the community during COVID-19 pandemic. Available from: https://www.hopkinsmedicine.org/news/articles/johns-hopkins-medical-students-mobilize-to-volunteer-for-The-community-during-covid-19-pandemic.
12. Klasen JM, Meienberg A, Nickel C, et al. SWAB team instead of SWAT team: medical students as a frontline force during the COVID-19 pandemic. Med Educ. 2020;54(9):860. doi:10.1111/medu.14224
13. Saudi Red Crescent Authority. Volunteering system. Available from: https://volunteer.srca.org.sa/#!/home.
14. Chaffee M. Willingness of health care personnel to work in a disaster: an integrative review of the literature. Disaster Med Public Health Prep. 2009;3(1):42–56. doi:10.1097/DMP.0b013e31818e8934
15. World Health Organization Regional Office for Europe. WHO announces COVID-19 outbreak a pandemic; 2020. Available from: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-A-pandemic.
16. Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi:10.1016/S0140-6736(20)30251-8
17. International Monetary Fund. Policy responses to COVID-19. Available from: https://www.imf.org/en/Topics/imf-and-covid19/Policy-Responses-to-COVID-19.
18. Adly HM, AlJahdali IA, Garout MA, et al. Correlation of COVID-19 pandemic with healthcare system response and prevention measures in Saudi Arabia. Int J Environ Res Public Health. 2020;17(18):6666. doi:10.3390/ijerph17186666
19. Khan A, Alsofayan Y, Alahmari A, et al. COVID-19 in Saudi Arabia: the national health response. East Mediterr Health J. 2021;27(11):1114–1124. doi:10.26719/emhj.21.048
20. Alhraiwil NJ, Al-Aqeel S, AlFaleh AF, et al. Impact of COVID-19 on the 937 telephone medical consultation service in Saudi Arabia. Int J Telemed Appl. 2022;2022:4181322. doi:10.1155/2022/4181322
21. Pickell Z, Gu K, Williams AM. Virtual volunteers: the importance of restructuring medical volunteering during the COVID-19 pandemic. Med Humanit. 2020;46(4):537–540. doi:10.1136/medhum-2020-011956
22. United Nations. Household size and composition around the world; 2017. Available from: https://www.un.org/en/development/desa/population/publications/pdf/ageing/household_size_and_composition_around_the_world_2017_data_booklet.pdf.
23. Hussein S, Ismail M. Ageing and elderly care in the Arab region: policy challenges and opportunities. Ageing Int. 2017;42(3):274–289. doi:10.1007/s12126-016-9244-8
24. US Centers for Disease Control and Prevention. Underlying medical conditions associated with high risk for severe COVID-19: information for healthcare providers. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html.
25. AlSaif HI, AlDhayan AZ, Alosaimi MM, et al. Willingness and self-perceived competence of final-year medical students to work as part of the healthcare workforce during the COVID-19 pandemic. Int J Gen Med. 2020;13:653–661. doi:10.2147/IJGM.S272316
26. Mansour A, Alharbi S, Almutiri E, et al. Knowledge, attitudes, and willingness of medical students to volunteer in a disaster at Unaizah College of Medicine, Qassim University, Saudi Arabia. Int J Med Dev Ctries. 2020;4(8):1198–1207.
27. Michno DA, Tan J, Adelekan A, et al. How can we help? Medical students’ views on their role in the COVID-19 pandemic. J Public Health. 2021;43(3):479–489. doi:10.1093/pubmed/fdaa271
28. Abalkhail A, Alwashmi ASS, Alslamah T, et al. Personal and family-related factors on willingness to volunteer among undergraduate medical students during COVID-19 pandemic in Saudi Arabia: a cross-sectional study. Eur Rev Med Pharmacol Sci. 2021;25(24):7709–7716. doi:10.26355/eurrev_202112_27617
29. Lazarus G, Findyartini A, Putera A, et al. Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: a cross-sectional survey in Indonesia. BMC Med Educ. 2021;21(1):138. doi:10.1186/s12909-021-02576-0
30. AlOmar R, AlShamlan N, AlAmer N, et al. What are the barriers and facilitators of volunteering among healthcare students during the COVID-19 pandemic? A Saudi-based cross-sectional study. BMJ Open. 2021;11(2):e042910. doi:10.1136/bmjopen-2020-042910
31. Arab News. Groups exempt from workplace attendance listed in Saudi Arabia; 2022. Available from: https://arab.news/85qzu.
32. Carlo G, Okun M, Knight G, De Guzman M. The interplay of traits and motives on volunteering: agreeableness, extraversion and prosocial value motivation. Pers Individ Dif. 2005;38(6):1293–1305. doi:10.1016/j.paid.2004.08.012
33. Li M, Taylor EG, Atkins KE, Chapman GB, Galvani AP. Stimulating influenza vaccination via prosocial motives. PLoS One. 2016;11(7):e0159780.
34. Devnani M. Factors associated with the willingness of health care personnel to work during an influenza public health emergency: an integrative review. Prehosp Disaster Med. 2012;27(6):551–566. doi:10.1017/S1049023X12001331
35. Slivkoff MD, Johnson C, Tackett S. First-year medical student experiences adjusting to the immediate aftermath of COVID-19 [published online ahead of print, 2021 Jan 22]. Med Sci Educ. 2021;31(2):1–8.
36. Shibu A. Medical student engagement during the COVID-19 pandemic-A student perspective. Med Educ. 2021;55(6):768. doi:10.1111/medu.14474
37. Ministry of Health, Saudi Arabia. COVID 19 Dashboard: Saudi Arabia; 2022. Available from: https://covid19.moh.gov.sa/.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
