Back to Journals » Clinical Interventions in Aging » Volume 12
Which is preferable for orthostatic hypotension diagnosis in older adults: active standing test or head-up tilt table test?
Authors Aydin AE, Soysal P , Isik AT
Received 9 December 2016
Accepted for publication 5 January 2017
Published 25 January 2017 Volume 2017:12 Pages 207—212
DOI https://doi.org/10.2147/CIA.S129868
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Ali Ekrem Aydin,1 Pinar Soysal,2 Ahmet Turan Isik1
1Center for Aging Brain and Dementia, Department of Geriatric Medicine, Faculty of Medicine, Dokuz Eylul University, Izmir, Turkey; 2Kayseri Education and Research Hospital, Geriatric Center, Kayseri, Turkey
Background: Correct evaluation of orthostatic hypotension (OH) is crucial in geriatric practice, since OH is associated with mortality and morbidity. The study aimed to determine the most appropriate method for measuring blood pressure in transition from supine to upright position in order to diagnose OH in older adults.
Methods: Active standing test (AST) and head-up tilt table (HUT) test as well as comprehensive geriatric assessment (CGA), including mini-mental state examination or the cognitive state test, mini-nutritional assessment, basic and instrumental activities of daily living, and Tinetti performance-oriented mobility assessment indexes, were performed in 290 geriatric patients.
Results: The prevalence of OH during HUT and AST was 19% and 37%, respectively. In patients with OH during HUT, the frequency of dementia and recurrent falls were higher (P<0.05); on the other hand, the levels of serum vitamin D and albumin and estimated glomerular filtration rate were lower (P<0.05). However, all these parameters for OH during AST were not significant (P>0.05). Comparison of the groups according to CGA measurements revealed significant differences in terms of cognition, nutritional status, activities of daily life, and balance function in patients with OH only during HUT (P<0.05), but not during AST (P>0.05). The sensitivity, specificity, positive predictive value, and negative predictive values of AST were 49.0%, 65.5%, 25.0%, and 84.6% respectively, according to HUT.
Conclusion: The results suggest that orthostatic blood pressure changes determined by HUT might be of higher clinical significance than that by AST in older adults. It might be important that the evaluation of OH by HUT should be included in daily geriatric practice.
Keywords: active standing test, head-up tilt table, orthostatic hypotension, diagnosis
Introduction
Orthostatic hypotension (OH) is a common clinical problem among older adults, which affects nearly 25%–30% of this population.1,2 Common comorbidities, such as diabetes mellitus (DM), dehydration, and malnutrition, and frequent use of diuretics, antihypertensive drugs, levodopa, and benzodiazepines might lead to OH3 that may cause dizziness, blackouts, blurred vision, balance impairment, recurrent falls, dyspnea, angina pectoris, paracervical and lumbar pain, weakness, and nausea.4,5 However, one-third of elderly adults with OH are asymptomatic.6 The correct diagnosis of OH in the elderly is of great importance; previous studies demonstrated association of OH with mortality, ischemic stroke, falls, cognitive failure, impaired sleep quality, depression, renal failure, and cognitive impairment in older adults.2,7–12 Therefore, evaluation of orthostatic blood pressure (BP) changes should be a part of the comprehensive geriatric assessment (CGA).13
According to the consensus statement on the detection of OH published in 1996, the diagnosis of OH is made in the event of at least 20 mmHg decrease in systolic blood pressure and/or at least 10 mmHg decrease in diastolic blood pressure within the first 3 min after standing.14 However, there is no consensus on the optimum method for diagnosis of OH.
Active standing test (AST) has been used in the majority of studies;15–18 however, many older adults cannot change their positions easily during transition from supine to upright position, because of existing comorbidities and immobility. Therefore, the BP change during the AST may not be evaluated objectively. On the other hand, an acceptable alternative to AST is head-up tilt table (HUT) test, which may be a more convenient method to detect OH in the elderly,19 but the data are limited.
The aim of this study was to determine the optimum evaluation of measurement of orthostatic BP changes in older adults by comparing the results of AST and HUT.
Patients and methods
Patients
A total of 290 elderly patients, who were admitted to the geriatric clinic in a university hospital between January 2014 and May 2015, were included in this prospective and cross-sectional observational study. In addition to CGA, HUT and AST were performed in those geriatric patients after obtaining their informed written consents.
Inclusion criteria
All patients in the age group of 65 years or older admitted to the geriatric outpatient clinic for any reason were included in the study.
Exclusion criteria
Patients with the following conditions were excluded: severe anemia (<10 g/dL), severe metabolic acidosis, electrolyte imbalance, severe kidney or heart failure, hypotensive shock, coma, severe mitral valve or aortic valve stenosis, tachycardia, severe proximal cerebral artery stenosis, severe coronary artery disease, prior stroke or myocardial infarction in the past 7 days, lower extremity fractures, all of which are the contraindications of HUT, were excluded.20 Additionally, patients who cannot stand up actively by themselves or who were immobile were not included in the study. Consequently, 290 patients were available for study analysis.
BP measurements
AST measurements
The first BP measurement was taken following 5 min of rest at the lying position; afterward the patients were raised upright and the measurement was repeated on the same arm, at the 3rd minute, using a mercury sphygmomanometer with an appropriately sized cuff.14
HUT measurements
Standardized tilt table was used during HUT (G-71 Tilt table; Gemesan, Istanbul, Turkey). BP measurement was taken following 5 min of rest at the lying position; afterward the patients were raised upright at 60°–80° and the measurement was repeated on the same arm at the 3rd minute using a patient monitor with an appropriately sized cuff (M69S Patient monitor; Biolight, Zhuhai, People’s Republic of China). During HUT, the patients were asked for OH symptoms.14
OH diagnosis was defined as a drop of at least 20 mmHg in systolic blood pressure and/or 10 mmHg in diastolic blood pressure upon the change in position in both AST and HUT.14
Comprehensive geriatric assessment
Demographic data (age, gender, and education status) of the patients, history of falls (according to the information obtained from the patient or patient’s relatives, presence of more than one fall not associated with seizure or acute stroke within the past year), and personal history of chronic diseases (hypertension, DM, coronary artery disease, congestive heart failure, peripheral vascular disease, dementia, hyperlipidemia, cerebrovascular disease, depression, polypharmacy, and tobacco use) were questioned in detail. In addition, for each patient, scores of the mini-mental state examination or the cognitive state test,21 mini-nutritional assessment, basic and instrumental activities of daily living, and Tinetti performance-oriented mobility assessment indexes were also recorded. Body mass index was calculated as body weight in kilograms divided by the squared value of body height in meters (kg/m2).
Laboratory findings
Certain laboratory tests were performed to assess the biochemical, metabolic, and nutritional status of patients in our geriatric department. Thus, hospital laboratory records were also obtained for complete blood count, kidney and liver functions, cholesterol levels, thyroid-stimulating hormone, glycated hemoglobin, vitamin B12, folic acid, and vitamin D levels. All these biochemical tests were carried out on Diagnostic Modular Systems autoanalyzer (E170 and P800 Diagnostic modular systems; Roche, Basel, Switzerland).
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and evaluated by the Kolmogorov–Smirnov test for normal distribution. Continuous variables with normal distribution were evaluated with independent sample t-test whereas those with abnormal distribution were post hoc evaluated by the Mann–Whitney U test. Differences in proportions were evaluated by the chi-square test and Fisher’s exact test. The differences between dependent categorical variables were evaluated by McNemar’s test. Kappa value was used for consistency. Probabilities <0.05 were considered significant. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) 15.0 (SPSS Inc., Chicago, IL, USA). Adequate sample size was calculated (244 patients for 95% confidence interval).
Ethics
The investigation conformed to the Declaration of Helsinki and was approved by the local ethics committee (Dokuz Eylul University Ethics Committee, Izmir, Turkey, 2013/23-08).
Results
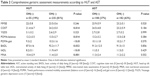
The prevalence of OH during HUT and AST was 19% and 37%, respectively. The differences between the groups with and without OH during HUT and AST are demonstrated in Table 1.
The frequency of dementia and recurrent falls were higher in the group with OH during HUT (P<0.05). The serum levels of vitamin D and albumin and estimated glomerular filtration rate were lower in those with OH during HUT (P<0.05). It was determined that all these parameters for OH during AST were not significant (P>0.05; Table 1). Comparison of the groups according to CGA measurements revealed no differences in terms of cognition, mood, nutritional status, activities of daily life, and balance function in patients with OH only during AST (P>0.05), whereas the cognitive state test, Tinetti performance-oriented mobility assessment, mini-nutritional assessment, basic activity of daily living, and instrumental activity of daily living were lower in patients with OH during HUT (P<0.05; Table 2).
The AST had a specificity of 65.5% and a sensitivity of 49.0% for identifying OH according to HUT. The positive predictive value and negative predictive value of AST were 25% and 84.6%, respectively.
Discussion
Orthostatic BP changes determined by HUT might be of higher clinical significance than those determined by AST in older adults. It might be important that the evaluation of OH by HUT should be included in daily geriatric practice.
OH is a major geriatric syndrome, but it may be overlooked despite numerous complications such as mortality, ischemic stroke, falls, cognitive deficit, depression, and sleep disorders.12,22–25 Therefore, accurate diagnosis of OH is crucial in older adults. The prevalence of OH, which is reported as 9.5%–37% by AST and 21%–51% by HUT in the current literature, varies according to the method used and patients’ characteristics.19,26–31 However, in most of these studies, the prevalence was obtained by using either AST or HUT. Only two studies in the literature have compared AST and HUT as a method in the same sample of patients.19,32 Although Faraji et al obtained twofold higher OH prevalance during HUT than AST, the retrospective nature of the study, the lack of methods following one after another (AST and HUT), and extending HUT to the 40th minute may lead to different outcomes.32 Cooke et al retrospectively evaluated the cases between the age of 22 and 93 years,19 whereas in the present study, only older adults were included and revealed two different prevalances by two different methods in the same sample of patients. Furthermore, Rickards et al compared HUT with the squat-stand test and emphasized that active joint and muscle movements induce vasoconstriction in the blood vessels, causing an increase in transient ischemia and vasoactive metabolites in the muscles, which reduce venous return with compensatory vasodilatation in the lower extremity, resulting in more BP drop at baseline compared to HUT.33 The effort exerted by a number of older adults during transition from supine to upright position due to existing comorbidities and immobility may reduce venous return with similar mechanisms. Physiopathologic changes such as aging-induced decreased baroreflex sensitivity and renin angiotensin aldosterone levels may also have been associated with more OH prevalence for AST than HUT.34,35
Previous studies reported that OH might be associated with age, cognitive decline, malnutrition, renal failure, gait-balance disorders and recurrent falls, decline in daily living activities, hypoalbuminemia, and hypovitaminosis D.2,5,7–12,29,36,37 In the present study, most of these findings were similar to the results obtained by only HUT but not by AST. Based on the outcomes, it can be speculated that clinical reflection of OH during HUT might be more valuable in older adults. Furthermore, when the clinical importance of OH as a geriatric syndrome and the fact that the majority of patients with OH are asymptomatic are taken into account,4 the importance of reaching the correct diagnosis of OH by HUT is obvious in geriatric practice.
On the other hand, when HUT was used as the gold standard for comparison, the lower sensitivity, specificity, and positive predictive value of the AST method were determined. In this case, to strengthen the diagnosis of OH, older adults should be verified with HUT, even in the presence of OH diagnosed by AST. To avoid overdiagnoses of OH by AST, auscultatory measurements of BP should be taken by a physician skilled in the technique recommended by the American Heart Association,38 or a digital blood sphygmomanometer can be preferred for BP measurements. In addition, large majority of older adults cannot change their positions easily and they exert efforts to sit and stand up from supine position during AST on account of existing comorbidities and mobility problems. Therefore, HUT seems to be a more objective method to diagnose OH.
Our study has several limitations. The first is the absence of measurements with a digital BP-measuring device during AST to compare with HUT. The second is the exclusion of some elderly patients in view of contraindications for HUT. The powerful aspects of our study, however, include its prospective design, adequate sample size, and the use of HUT test for diagnosis and comparison with AST. Besides, all the participants are older adults, so our study population represents geriatric patients vigorously.
Conclusion
These results suggest that orthostatic BP changes determined by HUT seem to have higher clinical significance than those determined by AST in older adults. It is important that the evaluation of OH by HUT should be included in daily geriatric practice.
Acknowledgment
The authors thank Hulya Ellidokuz for statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
Feldstein C, Weder AB. Orthostatic hypotension: a common, serious and underrecognized problem in hospitalized patients. J Am Soc Hypertens. 2012;6(1):27–39. | ||
Chen SY, Chen CH, Chang CM. [Management of orthostatic hypotension in the elderly]. Hu Li Za Zhi. 2010;57(5):89–95. Chinese [with English abstract]. | ||
Press Y, Punchik B, Freud T. Orthostatic hypotension and drug therapy in patients at an outpatient comprehensive geriatric assessment unit. J Hypertens. 2016;34(2):351–358. | ||
Fedorowski A, Melander O. Syndromes of orthostatic intolerance: a hidden danger. J Intern Med. 2013;273(4):322–335. | ||
Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120(10):841–847. | ||
Arbogast SD, Alshekhlee A, Hussain Z, McNeeley K, Chelimsky TC. Hypotension unawareness in profound orthostatic hypotension. Am J Med. 2009;122(6):574–580. | ||
Galizia G, Convertino G, Testa G, Langellotto A, Rengo F, Abete P. Transient ischemic attack caused by delayed orthostatic hypotension in an elderly hypertensive patient. Geriatr Gerontol Int. 2012;12(3):565–567. | ||
McHugh JE, Fan CW, Kenny RA, Lawlor BA. Orthostatic hypotension and subjective sleep quality in older people. Aging Ment Health. 2012;16(8):958–963. | ||
Soysal P, Yay A, Isik AT. Does vitamin D deficiency increase orthostatic hypotension risk in the elderly patients? Arch Gerontol Geriatr. 2014;59(1):74–77. | ||
Richardson J, Kerr SR, Shaw F, Kenny RA, O’Brien JT, Thomas AJ. A study of orthostatic hypotension in late-life depression. Am J Geriatr Psychiatry. 2009;17(11):996–999. | ||
Mehrabian S, Duron E, Labouree F, et al. Relationship between orthostatic hypotension and cognitive impairment in the elderly. J Neurol Sci. 2010;299(1–2):45–48. | ||
Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc. 2011;59(3):383–389. | ||
Soysal P, Isik AT, Buyukaydin B, Kazancioglu R. A comparison of end-stage renal disease and Alzheimer’s disease in the elderly through a comprehensive geriatric assessment. Int Urol Nephrol. 2014;46(8):1627–1632. | ||
Schatz IJ, Bannister R, Freeman RL, et al. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. Neurology. 1996;46(5):1470. | ||
Weiss A, Grossman E, Beloosesky Y, Grinblat J. Orthostatic hypotension in acute geriatric ward: is it a consistent finding? Arch Intern Med. 2002;162(20):2369–2374. | ||
Isik AT, Soysal P, Usarel C. Effects of acetylcholinesterase inhibitors on balance and gait functions and orthostatic hypotension in elderly patients with Alzheimer disease. Am J Alzheimers Dis Other Demen. 2016;31(7):580–584. | ||
Lampela P, Lavikainen P, Huupponen R, Leskinen E, Hartikainen S. Comprehensive geriatric assessment decreases prevalence of orthostatic hypotension in older persons. Scand J Public Health. 2013;41(4):351–358. | ||
Luukinen H, Koski K, Laippala P, Kivelä SL. Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med. 1999;159(3):273–280. | ||
Cooke J, Carew S, O’Connor M, Costelloe A, Sheehy T, Lyons D. Sitting and standing blood pressure measurements are not accurate for the diagnosis of orthostatic hypotension. QJM. 2009;102(5):335–339. | ||
Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS), Moya A, Sutton R, Ammirati F, et al. Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J. 2009;30(21):2631–2671. | ||
Babacan-Yildiz G, Isik AT, Ur E, et al. COST: cognitive state test, a brief screening battery for Alzheimer disease in illiterate and literate patients. Int Psychogeriatr. 2013;25(3):403–412. | ||
Chou RH, Liu CJ, Chao TF, et al. Association between orthostatic hypotension, mortality, and cardiovascular disease in Asians. Int J Cardiol. 2015;195:40–44. | ||
Jodaitis L, Vaillant F, Snacken M, et al. Orthostatic hypotension and associated conditions in geriatric inpatients. Acta Clin Belg. 2015;70(4):251–258. | ||
Soysal P, Aydin AE, Koc Okudur S, Isik AT. When should orthostatic blood pressure changes be evaluated in elderly: 1st, 3rd or 5th minute? Arch Gerontol Geriatr. 2016;65:199–203. | ||
Angelousi A, Girerd N, Benetos A, et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens. 2014;32(8):1562–1571. | ||
Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006;67(1):28–32. | ||
Gurevich T, Machmid H, Klepikov D, Ezra A, Giladi N, Peretz C. Head-up tilt testing for detecting orthostatic hypotension: how long do we need to wait? Neuroepidemiology. 2014;43(3–4):239–243. | ||
Kim HA, Lee H, Park KJ, Lim JG. Autonomic dysfunction in patients with orthostatic dizziness: validation of orthostatic grading scale and comparison of Valsalva maneuver and head-up tilt testing results. J Neurol Sci. 2013;325(1–2):61–66. | ||
Fedorowski A, Burri P, Melander O. Orthostatic hypotension in genetically related hypertensive and normotensive individuals. J Hypertens. 2009;27(5):976–982. | ||
Hartog LC, Cimzar-Sweelssen M, Knipscheer A, et al. Orthostatic hypotension does not predict recurrent falling in a nursing home population. Arch Gerontol Geriatr. 2017;68:39–43. | ||
Enrique Asensio L, Andrea Aguilera C, Maria de los Angeles Corral C, et al. Prevalence of orthostatic hypotension in a series of elderly Mexican institutionalized patients. Cardiol J. 2011;18(3):282–288. | ||
Faraji F, Kinsella LJ, Rutledge JC, Mikulec AA. The comparative usefulness of orthostatic testing and tilt table testing in the evaluation of autonomic-associated dizziness. Otol Neurotol. 2011;32(4):654–659. | ||
Rickards CA, Newman DG. A comparative assessment of two techniques for investigating initial cardiovascular reflexes under acute orthostatic stress. Eur J Appl Physiology. 2003;90(5–6):449–457. | ||
Low PA. Prevalence of orthostatic hypotension. Clin Auton Res. 2008;18 (Suppl 1):8–13. | ||
Okada Y, Galbreath MM, Shibata S, et al. Relationship between sympathetic baroreflex sensitivity and arterial stiffness in elderly men and women. Hypertension. 2012;59(1):98–104. | ||
Ometto F, Stubbs B, Annweiler C, et al. Hypovitaminosis D and orthostatic hypotension: a systematic review and meta-analysis. J Hypertens. 2016;34(6):1036–1043. | ||
Robertson D. The pathophysiology and diagnosis of orthostatic hypotension. Clin Auton Res. 2008;18 (Suppl 1):2–7. | ||
Curb JD, Labarthe DR, Cooper SP, Cutter GR, Hawkins CM. Training and certification of blood pressure observers. Hypertension. 1983;5(4):610–614. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.