Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
Which drugs cause treatment-related problems? Analysis of 10,672 problems within the outpatient setting
Authors Al-Taani GM, Al-Azzam SI, Alzoubi KH , Aldeyab MA
Received 19 July 2018
Accepted for publication 26 September 2018
Published 16 November 2018 Volume 2018:14 Pages 2273—2281
DOI https://doi.org/10.2147/TCRM.S180747
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Ghaith M Al-Taani,1 Sayer I Al-Azzam,2 Karem H Alzoubi,2 Mamoon A Aldeyab3
1Department of Pharmacy Practice, Faculty of Pharmacy, Yarmouk University, Irbid, Jordan; 2Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 3School of Pharmacy and Pharmaceutical Science, University of Ulster, Coleraine, County Londonderry, UK
Background: Treatment-related problems (TRPs) may pose risks for patients if unaddressed. With the increased complexity of health care, it is important to target pharmacists’ efforts to patients that are at high risk for TRPs.
Objectives: The present study aimed to identify medications most commonly associated with TRPs.
Setting: Outpatient departments of five public and teaching hospitals in Jordan.
Method: TRPs and drugs most commonly implicated with TRPs were assessed for patients recruited from outpatient clinics in five major hospitals in Jordan using a standardized and validated pharmaceutical care manual.
Main outcome measure: Drugs associated with different types of TRPs.
Results: Ultimately, 2,747 patients, with a total of 10,672 TRPs, were included in the study. The medication groups most commonly associated with TRPs were cardiovascular (53.0%), endocrine (18.1%), and gastrointestinal (7.7%) drugs. The most common specific drugs associated with TRPs from any category were atorvastatin (12.5%), metformin (8.5%), simvastatin (6.2%), and enalapril (5.9%). Cardiovascular medications were the most common drugs implicated with multiple subtypes of TRPs – most commonly, allergic reaction or undesirable effect (88.5%), drug product not available (87.3%), safety interaction issues (81.8%), a need for additional or more frequent monitoring (78.0%), and more effective drugs available (77.2%). Hypertension, diabetes mellitus, and dyslipidemia were the most common diseases associated with different subtypes of TRPs.
Conclusion: The present study identified high-risk drugs for TRPs, which can be used as identification of targeting approach TRPs. Such an approach would improve care provided to patients and can inform health care policies.
Keywords: drug related problems, drug therapy problems, high alert medication, Jordan, pharmaceutical care, treatment related problems
Introduction
Treatment-related problems (TRPs) are associated with the use of medications that result in decreased therapeutic outcomes, which are usually addressed by pharmacists. The impact of such problems is significant. TRPs can lead to decreased disease control and adverse effects. Such TRPs might lead to overutilization of health care resources, with associated high costs for the health care system, in particular for elderly patients.1–9 Approximately one-tenth of hospital admissions are attributed to drugs and TRPs are common in institutionalized patients, such as those in nursing homes.2,6,8,9 TRPs are also common in primary care, particularly after hospital discharge.10,11 The high impact associated with TRP issues can provide a strong case for pharmacist service to address such important problems, particularly serious, clinically significant TRPs.
As the complexity of treatment and the number of available treatments increase, addressing TRPs might pose a challenge for the pharmacist. In direct patient care, increased emphasis should be paid to appropriate targeting or case finding for high-risk patients. A “trigger” tool that alerts the health care professional for the possibility of TRPs is an approach that can be applied in targeting. A convenient and easy trigger tools would be to formulate a list of drugs commonly associated with TRPs as a targeting mechanism. This concept has been adopted by accreditation bodies such as the Joint Commission (Oakbrook Terrace, IL, USA), which maintains a list of high-alert medications. In addition, the concept of high-alert medications is highlighted in academic curricula for pharmacy, particularly the clinical pharmacy curriculum.12 The Institution of Safe Medication Practice (ISMP) list for high-alert medications identifies drugs associated with risk in cases of error. Examples of these medications are antiretroviral agents, chemotherapeutic agents, hypoglycemic agents and insulin, immunosuppressants, opioids, carbamazepine, midazolam (liquid), propylthiouracil, warfarin, and pregnancy category X drugs.13
Internationally, as clinical pharmacy is steadily developing, such targeted drug lists can be useful especially for health care systems with limited resources. In Jordan, a number of studies have been published describing typical pharmaceutical care research and the impact of clinical pharmacy interventions.14,15 Other studies have assessed the prevalence of TRPs.16,17 The latter studies were conducted on heterogeneous settings; one study was conducted on a single health center and found the most frequent TRPs (83.3%) are the need for education and counseling.16 Another study that was based on home visits showed that the mean number of TRP is 7.4 per patient.17 In a study conducted on hospitalized patients, average TRPs were 9.35 per patient.18
Notably, previous studies were focused on certain types of TRPs, particularly adverse reactions, and have been limited to hospital admissions.19–21 Additionally, the traditional high-alert drug approach was limited to drugs that have a low safety margin in which errors associated with the use are devastating. We have previously identified the most common TRPs and their frequency in such a limited resource health care system outpatient setting.14 However, no study has linked medications/groups to TRPs in an effort to create a sort of focused TRP medication list for this health care setting. Thus, there is a need for a large, multicenter study to identify medications that are mostly associated with TRPs in such health care settings. Such an approach will be useful for pharmacists in supporting patient medication use by addressing TRPs, as opposed to medications that would be associated with serious consequences in the case of error.
Aim of the study
The present study aimed to assess medications most commonly associated with TRPs within the outpatient setting. Thus, the current study is an advanced step of our previous study,14 focusing on relating TRPs with specific medications/groups of medication in an effort to create a sort of focused TRP medication list.
Method
Setting
The present study was carried out in eleven outpatient departments including respiratory, endocrine, and cardiovascular in five hospitals in the northern, central, and southern areas of Jordan. These hospitals represent major hospitals in distinctive areas of Jordan and include King Abdullah University Hospital (KAUH), a teaching hospital affiliated with the Jordan University of Science and Technology in Irbid; Jordan University Hospital, a teaching hospital affiliated with the University of Jordan in Amman; Al-Basheer Hospital, a public hospital in Amman; Princess Basma Hospital, a public hospital in Irbid; and Al-Karak Hospital, a public hospital in Al-Karak.
Patients selection
During the study period (September 2102–December 2013), patients who attended cardiology, endocrine, and respiratory outpatient clinics and met the selection criteria were invited to take part in the study. The selection criteria included adult patients who have used at least two long-term medications (either new or long-standing) and who have one or more or chronic medical conditions. After explaining the study to those patients who agreed to participate, signed written informed consents were obtained from each patient. A parent or legal guardian of any participant under the age of 18 years also provided written informed consent. Furthermore, the study protocol was approved by appropriate research ethics committees and the institutional review board of Jordan University of Science and Technology.
Data collection
Pharmacist review for TRP determination
Recruited patients were assessed for TRPs by clinical pharmacists (n=11, one clinical pharmacist/department), who are involved in direct patient care and are licensed to practice pharmacy and hold Doctor of Pharmacy degree. The identification of TRPs was carried according to a systematic pharmaceutical care manual that the clinical pharmacists were trained on using to identify and document TRPs. The manual allowed assessment for TRPs, via evidence-based approach, which incorporates best evidence in decision making. TRPs were identified via interview of patients and referral to medical records22,23 against national and international compendiums and guidelines, where a comprehensive, full range of TRPs was identified. The TRPs classification system used was based on modified version of classification of TRPs by Aburuz et al,20 in which it was modified to be adapted for use in outpatient setting. The validity and reliability of the classification system were established on a sample of 200 patients and were found to be valid and reliable with good inter-rater agreement. Full details of validation and reliability tests have been published elsewhere.22 The classification system groups TRPs into indication, effectiveness, safety, patient related, and miscellaneous areas.18 Of the most important categories of TRPs identified is adherence-related problems, which included issues related to adherence to drugs, which was assessed indirectly by interview guided by an adherence questionnaire, and adherence to self-care activities or non-pharmacological therapy (eg, smoking abstinence and dietary recommendations), which was assessed via interview of patients. Interview with each patient took ~15 minutes.
Outcomes of the study
The following outcomes were recorded for each TRP:
- Drugs associated with TRPs.
- The disease associated with TRPs.
The implicated medications with TRPs were recorded together with the linked disease. The British National Formulary drug classification system was adopted. Assessment of most common drugs associated with TRPs of any category was carried out. For each category of TRPs, the most common drugs associated with each category of TRPs were documented. In addition, the disease linked to each type of TRPs was investigated. The present study was an advance of a previous study that assessed medication-related problems; full details are shown elsewhere.14 Data were coded using the SPSS, version 21.0 (SPSS Inc., Chicago, IL, USA) entry program. The data were summarized using frequency tables including mean values and/or percentage.
Results
General characteristics of the patients recruited
During the study period (September 2012–December 2013), the total number of patients recruited was 2,747 patients. Approximately two-thirds (68.3%) of the patients were between 18 and 64 years old, and about 60% of the patients were females. Regarding the level of education of the study sample, 16.3% of patients recruited were illiterate, with approximately one-quarter of the patients having completed primary (29.3%), secondary (29.0%), or tertiary (ie, university; 25.3%) education.
In addition, 96.5% of patients were insured. After assessing the patients, it was noted that 9.1% of the patients had a problem in medication adherence, 48.7% of the patients had a problem in illness knowledge, and 86.8% of the patients were nonadherent to self-care and nonpharmacological recommendations relevant to their disease. Table 1 summarizes the demographic, social, and clinical characteristics of the patients recruited.
  | Table 1 Demographic, social, and clinical characteristics of the patient recruited |
Most patients had cardiovascular disease and diabetes while some patients had respiratory diseases.
Drug groups associated with TRPs
After assessing the 2,747 patients recruited, it was determined that they were prescribed an average of 5.6 medications and had a total of 10,672 TRPs. This yields an average of 11.1 TRPs per patient. The medication groups most commonly associated with TRPs of any category were cardiovascular (53.0%), endocrine (18.1%), and gastrointestinal (7.7%) systems. Full details are illustrated in Table 2. Table 3 shows the specific medications associated with TRPs of any category, which were atorvastatin (12.5%), metformin (8.5%), simvastatin (6.2%), enalapril (5.9%), isosorbide dinitrate (4.6%), albuterol (4.6%), aspirin (4.5%), lansoprazole (4.2%), and insulin (any type; 4.0%).
  | Table 2 Frequency of drug groups (BNF drug class) causing any TRPs |
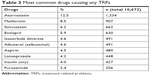  | Table 3 Most common drugs causing any TRPs |
Cardiovascular medications were the most common drugs implicated with many subtypes of TRPs, including allergic reactions or undesirable effects (88.5%), unavailable drug products (87.3%), safety interaction issues (81.8%), and more effective drugs available (77.2%). Gastrointestinal medications were the most common drugs implicated with “drugs with no indication” (70.5%) and “efficacy interaction issues” (60.0%). Central nervous system medications were most commonly implicated with “addiction or recreational drug use” (40.0%). Endocrine medications were most commonly implicated with “the DRP of being contraindicated or unsafe for the patient’s condition” (55.4%). Blood and nutrition medications were the most common drugs implicated with “a need for an additional diagnostic test” (50.0%). Regarding adherence to medications, 211 patients had a problem; of these, 48.8% were nonadherent to all medications, 20.4% to cardiovascular medications, 16.1% to respiratory medications, and 11.8% to endocrine medications (Table 4).
Diseases linked with TRPs
The present study assessed the most common diseases linked with different types of TRPs. As summarized in Table 5, hypertension, diabetes mellitus, and dyslipidemia were the most common diseases associated with different subtypes of TRPs.
Discussion
The present study identified medication groups associated with TRPs, which researchers consistently agree are common, undesirable, and costly.1–9 The identification of medications associated with TRPs can prove useful in targeting pharmacists’ efforts to patients most at risk for such problems. In addition to clinical value, such an enhanced targeting approach helps to improve the logistics of the delivery of pharmacists’ service and would be useful for documenting the value of pharmacist interventions. An interesting finding of the present study is that cardiovascular and gastrointestinal drugs were implicated with most categories of TRPs, thereby qualifying as high-risk drugs for TRPs. The present study assessed TRPs in a comprehensive manner, using a standardized and validated methodology, and included medical TRPs in addition to drug-specific problems. The present study increases the understanding of the medications associated with care issues according to different categories, suggesting that the pharmacist could play a key role in TRPs identification and care.
In the present study, ~80% of TRPs were related to endocrine, cardiovascular, nervous, or respiratory drugs. The results indicated that a limited number of drug groups are considered high-risk medications for TRPs and can qualify as a priority for pharmacists in primary care. It is well-known that cardiovascular drugs are among the drugs that have a high risk of adverse drug reactions. Diabetes mellitus is among the ambulatory care sensitive conditions were inappropriate case management in primary care, can lead to hospital admissions.9,24
When comparing the ISMP high-alert drugs list13 with the drugs suggested from the current study, some differences are noted, which could be attributed to the definition of the “risk.” In addition, the high-risk medications identified in the present study are more directed toward patient care.
The TRPs identified in this study occurred in real outpatients with routine medication use and clinical care. Insulin and metformin have contributed to the biggest share of the endocrine medication associated with TRPs. Thus, the present study highlighted that these medications are a high risk for TRPs.
Different age groups and linked outcomes can result in different high-risk medication lists. For example, in elderly patients, antipsychotics as well as some nonprescription drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs), are commonly implicated in TRPs.6,25 Initial thoughts might suggest that the use of certain medications (eg, idiosyncrasy) increases the odds for TRPs; however, care quality also appears to be an important factor. For example, if patient treatment is not stepped up by the health care professional, the patient treatment goals will remain unmet.
Cardiovascular drugs were implicated with many categories of TRPs, including indication, efficacy, safety, adherence, and miscellaneous TRPs (eg, monitoring problem), suggesting that these cardiovascular medications are a high risk, subject to many TRPs, and are commonly implicated with hospital admissions.9,26,27 As expected, gastrointestinal drugs were commonly associated with the DRP “drugs without indication,” as these drugs are commonly prescribed without a prescription by community pharmacists without formal assessment by a medical practitioner. They were also highlighted as being implicated with “drug use without an indication” within the hospital setting in Jordan.18 Blood and nutrition medications were commonly associated with “the need for additional diagnostic tests.” In Jordan, within the hospital setting, important drugs associated with DRPs were gastrointestinal drugs (indication-related problems), cardiovascular drugs (efficacy-related problems), and NSAIDs (adverse effects).16
The present study showed a major problem related to illness knowledge (48.7% of patients) and adherence to self-care and nonpharmacological recommendation (86.8% of patients) among patients. This highlights a major issue in relation to the quality of professional patient counseling delivered primarily by pharmacists and, sometimes, other health care professionals. This was the case despite the fact that most (>85%) of the study samples received primary, secondary, or tertiary education and most of the study samples were somewhat young. In the present study, 211 problems related to adherence to medication were noted; and in about half of these problems, nonadherence was related to all medications. Nonadherence figures for medications are considerably lower than those for self-care and nonpharmacological recommendations. Within the hospital setting in Jordan, 4.4% of patients had a problem with adherence to drugs and 2.9% had a problem with adherence to self-care activities, which is many folds lower than those in the outpatient setting identified in the present study (9.1% and 86.8% of patients, respectively).16 Two studies carried out in Jordan (outpatient clinics and community pharmacies) highlighted that 46.1% and 73.4% of patients, respectively, were nonadherent to medications.28,29 The differences in the percentages of nonadherence/adherence among studies might be attributed to differences in the methodology and study settings.
Limitations
Although the present study identified a multitude of TRPs, the rate of acceptance and implementation of recommendations by medical practitioners and the clinical relevance of these TRPs were unknown. Such data provide an indication about the importance of the problems identified and reflect on medical practitioners’ views of the TRPs and value they perceive for pharmacist input. Yet, the present study still provided insights regarding patients’ medication management situation in the outpatient setting, and the results can guide further research in this area and improve clinical practice. The TRPs in the present study were assessed only by one practitioner. It is unknown whether there would be any discrepancies in terms of identified TRPs if there was an input from another rater. Most of the TRPs identified were associated with drugs or diseases affecting cardiovascular, endocrine, and respiratory system, which can be related to the study that was conducted in cardiovascular, endocrine, and respiratory clinics. Results of the present study are most likely generalizable for patients from Jordan. Additionally, a wider range of patients’ selection criteria is recommended for future studies where patients with acute medical condition are to be included in the analysis of TRPs.
The present study highlights a major need for enhanced medication management for patients; such need is relevant to medical practitioners and clinical pharmacists and can be extrapolated to the community pharmacies and hospitals given the large magnitude of the TRPs and their risk potential. Thus, more is needed from pharmacists to address such an important matter. Another recommendation of the present study relevant to the major finding is that targeting high-risk medications is a key at the present limited resource health care environment. Efforts should be made to disseminate knowledge about the magnitude and risk of TRPs and important high-risk drugs to the practicing pharmacists, via professional workshops, for example. Application of the targeting approach in routine care or in robust clinical trials to assess the impact of pharmacist intervention for TRPs to facilitate routine implementation. Other targeting approach can be suggested for future research making use of “more clinical” factors associated with TRPs or use a composite targeting approach taking input from different targeting strategies.
Conclusion
The present study identified medication groups implicated and linked diseases with TRPs from an outpatient sample from a number of hospitals in Jordan. TRPs were commonly associated with cardiovascular, endocrine, or gastrointestinal drugs. Cardiovascular medications were the most common drugs implicated with multiple subtypes of TRPs. Hypertension, diabetes mellitus, and dyslipidemia were the most common diseases associated with different subtypes of TRPs. Targeting patients utilizing high-risk drugs by pharmacists can improve patient health outcomes and can be useful to prioritize pharmacists’ efforts to those most at need.
Acknowledgment
This project was supported by the Scientific Research Funds (project number: 104/2012) at The Ministry of Higher Education and Scientific Research, Amman, Jordan.
Disclosure
The authors report no conflicts of interest in this work.
References
Ernst FR, Grizzle AJ. Drug-related morbidity and mortality: updating the cost-of-illness model. J Am Pharm Assoc. 1996;41:192–199. | ||
van den Bemt PM, Egberts TC, de Jong-van den Berg LT, Brouwers JR. Drug-related problems in hospitalised patients. Drug Saf. 2000;22(4):321–333. | ||
Bond CA, Raehl CL, Franke T. Medication errors in United States hospitals. Pharmacotherapy. 2001;21(9):1023–1036. | ||
Koh Y, Kutty FB, Li SC, Sc L. Drug-related problems in hospitalized patients on polypharmacy: the influence of age and gender. Ther Clin Risk Manag. 2005;1(1):39–48. | ||
Rodrigues MCS, Oliveira CD. Drug-drug interactions and adverse drug reactions in polypharmacy among older adults: an integrative review. Rev Lat Am Enfermagem. 2016;24:e2800. | ||
Ruths S, Straand J, Nygaard HA. Multidisciplinary medication review in nursing home residents: what are the most significant drug-related problems? The Bergen District Nursing Home (BEDNURS) study. Qual Saf Health Care. 2003;12(3):176–180. | ||
Guerreiro MP, Cantrill JM, Pisco L, Martins AP. Considerations on preventable drug related morbidity in primary care part I-impact of preventable drug-related morbidity. Rev Port Clin Geral. 2005;21:269–279. | ||
da Costa FA, Silvestre L, Periquito C, et al. Drug-related problems identified in a sample of portuguese institutionalised elderly patients and pharmacists’ interventions to improve safety and effectiveness of medicines. Drugs Real World Outcomes. 2016;3(1):89–97. | ||
Chan SL, Ang X, Sani LL, et al. Prevalence and characteristics of adverse drug reactions at admission to hospital: a prospective observational study. Br J Clin Pharmacol. 2016;82(6):1636–1646. | ||
Zaman Huri H, Fun Wee H, Huri HZ, Wee HF. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord. 2013;13:2. | ||
Ahmad A, Mast MR, Nijpels G, Elders PJ, Dekker JM, Hugtenburg JG. Identification of drug-related problems of elderly patients discharged from hospital. Patient Prefer Adherence. 2014;8:155–165. | ||
The Joint Commission. Available from: https://www.jointcommission.org. Accessed August 27, 2018. | ||
Institution of a Safe Medication Practice (ISMP). Available from: https://www.ismp.org. Accessed August 27, 2018. | ||
Al-Azzam SI, Alzoubi KH, Aburuz S, Alefan Q. Drug-related problems in a sample of outpatients with chronic diseases: a cross-sectional study from Jordan. Ther Clin Risk Manag. 2016;12:233–239. | ||
Aburuz SM, Alrashdan Y, Jarab A, Jaber D, Alawwa IA. Evaluation of the impact of pharmaceutical care service on hospitalized patients with chronic kidney disease in Jordan. Int J Clin Pharm. 2013;35(5):780–789. | ||
Al-Azzam SI, Alzoubi KH, Alefan Q, Alzayadeen RN. Evaluation of the types and frequency of drug-related problems and the association with gender in patients with chronic diseases attending a primary health care center in Jordan. Int Health. 2016;8(6):423–426. | ||
Basheti IA, Qunaibi EA, Bulatova NR, Samara S, Aburuz S. Treatment related problems for outpatients with chronic diseases in Jordan: the value of home medication reviews. Int J Clin Pharm. 2013;35(1):92–100. | ||
Aburuz SM, Bulatova NR, Yousef AM, Al-Ghazawi MA, Alawwa IA, Al-Saleh A. Comprehensive assessment of treatment related problems in hospitalized medicine patients in Jordan. Int J Clin Pharm. 2011;33(3):501–511. | ||
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions as cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329(7456):15–19. | ||
Howard RL, Avery AJ, Slavenburg S, et al. Which drugs cause preventable admissions to hospital? A systematic review. Br J Clin Pharmacol. 2007;63(2):136–147. | ||
Paul E, End-Rodrigues T, Thylén P, Bergman U. Adverse drug reactions a common cause of hospitalization of the elderly. A clinical retrospective study. Lakartidningen. 2008;105(35):2338–2342. | ||
Aburuz SM, Bulatova NR, Yousef AM. Validation of a comprehensive classification tool for treatment-related problems. Pharm World Sci. 2006;28(4):222–232. | ||
Aburuz S. The case for evidence-based pharmaceutical care. Res Social Adm Pharm. 2015;11(3):e146–e147. | ||
Caminal J, Starfield B, Sánchez E, Casanova C, Morales M. The role of primary care in preventing ambulatory care sensitive conditions. Eur J Public Health. 2004;14(3):246–251. | ||
Panda A, Pradhan S, Mohapatra G, Mohapatra J. Drug-related problems associated with self-medication and medication guided by prescription: a pharmacy-based survey. Indian J Pharmacol. 2016;48(5):515. | ||
Field TS, Gurwitz JH, Harrold LR, et al. Risk factors for adverse drug events among older adults in the ambulatory setting. J Am Geriatr Soc. 2004;52(8):1349–1354. | ||
Cramer JA, Benedict A, Muszbek N, Keskinaslan A, Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: a review. Int J Clin Pract. 2008;62(1):76–87. | ||
Basheti IA, Hait SS, Qunaibi EA, Aburuz S, Bulatova N. Associations between patient factors and medication adherence: a Jordanian experience. Pharm Pract. 2016;14(1):639. | ||
Awwad O, Akour A, Al-Muhaissen S, Morisky D. The influence of patients’ knowledge on adherence to their chronic medications: a cross-sectional study in Jordan. Int J Clin Pharm. 2015;37(3):504–510. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


