Back to Journals » Clinical Optometry » Volume 13
Wearing Pattern and Awareness About Contact Lens Wear in Secondary School Students in Kuala Lumpur
Authors Mohd-Ali B , Azmi N
Received 23 October 2020
Accepted for publication 4 May 2021
Published 20 May 2021 Volume 2021:13 Pages 155—160
DOI https://doi.org/10.2147/OPTO.S277786
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Bariah Mohd-Ali, NorAisyah Azmi
Optometry and Vision Science Program and Research Centre for Community Health, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Correspondence: Bariah Mohd-Ali
Optometry and Vision Science Program and Research Centre for Community Health, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Jalan Raja Muda Abdul Aziz, Kuala Lumpur, 50300, Malaysia
Tel +60392897602
Email [email protected]
Purpose: To investigate the wearing pattern and awareness about contact lens care among secondary school students in Kuala Lumpur.
Patients and Methods: This is a cross-sectional study using self-administered validated questionnaires. A total of 2500 questionnaires were distributed to secondary school students (aged 13 to 18 years) from 5 selected schools in Kuala Lumpur. Descriptive statistics were used to analyze the results.
Results: A total of 987 completed questionnaires were returned and analyzed. The response rate was 39.5%. Mean age of respondents was 15.5± 2.5 years with 54.6% females. Around 9.9% of the respondents were contact lens wearers with female majority (78.6%) and the main reasons for wearing contact lenses were cosmesis (42.8%) and comfort (32.7%). Majority (92.2%) were soft contact lens wearers and daily wear (monthly disposable) is the preferred modality. Nevertheless, 42.4% purchased their lenses from unlicensed vendors and 18.4% rinsed their lenses using tap water. Regarding contact lens care, more than 50% of the respondents were not aware about the correct way of handling contact lenses.
Conclusion: Soft contact lens wear is popular among the secondary school students in Kuala Lumpur but the level of practice and knowledge about CL care are unsatisfactory. Thus, health communication strategies and aggressive public ocular health education that can influence behavior changes in teenagers are needed to overcome these issues.
Keywords: teenagers, contact lens, public health
Introduction
Contact lens (CL) is a more popular option for vision correction compared with spectacles among teenagers. Several studies have highlighted the potential advantages of CLs for teenagers, particularly those who are active in sports and wish to improve self-perception or confidence and acceptance by peers.1,2 Wearing CL seemed to improve the children’s (8 to 12 years) and teenagers’ (13 to 17 years) perceptions on their appearances and participation in school activities and consequently lead to great satisfaction in their vision correction.1,2 Teenagers who wear CLs tend to require longer time for total vision correction per week compared with those who correct their vision with spectacles alone.3 In addition to these benefits, the known optical characteristics of CLs such as improvement in visual acuity, un-obstructive visual field, absence of peripheral distortions and myopia management have provided a sound justification for eye care practitioners to offer CLs for refractive error correction in the paediatric population. However, many specialists are reluctant to prescribe CLs due to concerns about safety and overall compliance for this age group. According to an earlier survey, only approximately 3% of new CL fits in the United States are performed on children between the ages of 6 and 12 years.4 Nevertheless, findings from a recent international survey indicate an increased rate of CL prescribing in children for the purpose of myopia control, specifically in Germanic countries of Austria, Germany and Switzerland.5
Susceptibility to adverse events such as microbial keratitis has often threatened the success of CL wear. Overnight wear and improper behaviours (such as poor cleaning, disinfection using reuse solution, poor lens case hygiene and infrequent lens case replacement) are known risk factors for microbial keratitis and other complications among soft CL wearers.6 Additionally, lack of understanding about proper contact lens maintenance is also an issue. In a survey about CL compliance, 30% of the respondents were not fully prepared for CL care and maintenance, thus indicating poor knowledge among CL wearers.7
Another identified risk factor for CL wear related complications is non-compliance to instructions about CL care. Around 98% of CL non-compliance is associated with problematic activities such as poor hand hygiene, CL exposure to tap water, overnight wear of unapproved lenses, delayed lens case replacement and solution misuse.8 Currently, there is no reported rate of CL-related microbial keratitis (CLMK) in Malaysia, but the following risk factors associated with CLMK have been identified from 94 cases seen in public hospitals: not washing hands before handling CL, not performing rubbing technique whilst cleaning CL, sleeping overnight with CL on the eye and overall non-compliance with lens care procedures.9 The authors concluded that public health education about CL care is important and should be conducted by local CL practitioners to minimise the occurrence of CLMK.
The precise number of CL wearers worldwide is difficult to determine but is estimated to be more than 140 million.10 In United States alone, CL is worn by approximately 3.6 million teenagers aged 12–17 years. In a 2009 survey, 67% of the annual newly prescribed CL in Malaysia were for patients aged above 21 years.11 In the International Contact Lens Prescribing report 2014, Morgan et al estimated that the mean age at fitting CL in Malaysia was 29.8 ± 10.7 years.12 To date, we believe that the age at fitting CL tends to be younger due to the growing percentage of myopia and acceptance of using CL as management for myopic children.13 Thus, teenagers must be informed about the dangers and advantages of wearing CLs prior to their purchase.
Reports about CL wear demographics in Malaysia are limited. Given that CL is an integral part of eye care and a viable market for eye care profession, local eye care practitioners must be aware of the pattern of use and knowledge level about CL wear in their country. This study aimed to investigate the wearing pattern and knowledge about CL wear among secondary school students in Kuala Lumpur (KL) by using validated questionnaires. Kuala Lumpur is the capital and largest city in Malaysia. We hypothesised that students living in KL have sufficient knowledge about CL wear and care due to good health care and internet services.
Patients and Methods
This cross-sectional study used a set of validated translated questionnaires about CL care and maintenance.14 The survey was self-administered and presented in Bahasa Malaysia (Malaysia’s national language). It has 22 questions (that cover lens cleaning and rinsing methods, lens storage, safe usage and replacement schedules) and was disseminated to secondary school children (aged 13–18 years) from around Kuala Lumpur. The technique of Krejcie and Morgan15 was used to calculate the sample size and the total number of respondents required was 2304.
Data was collected from 5 schools around Kuala Lumpur from September 2012 until May 2013. The schools were selected using stratified random sampling method from a directory provided by the Ministry of Education, and were located within 35 km radius from the city centre. The selected schools were SMK Seksyen 5, Wangsa Maju, SMK Padang Tembak, SMK Danau Kota, SMK Menjalara and SMK Taman Bukit Maluri. Written consents and permissions were acquired from the Ministry of Education, Malaysia (KP(BPPDP) 603/5/JLD.10), the Federal territory education office (JPNWP. 900–6/1/7JLD.4(56), schools’ principles, parents and students prior to data collection. The research ethical approval was obtained from the UKM Research Ethics Committee (UKM 1.5.3.5/244/NN-133-2012), and the protocol followed the tenets of the Declaration of Helsinki in using human subjects for research purposes.
This study was initially explained by the researchers to the school teachers and relevant authorities. Due to the school’s regulations, researchers were not allowed to meet with the students and therefore, the study protocol was explained to them by their respective teachers using written instructions given by the researchers. The students were given 7 days for completion and reminded by their respective teachers twice. The questionnaires were then collected by their teachers at the end of the week and later given to the researchers for analysis. Collected data were analysed descriptively using SPSS (version 20, IBM, Armonk, NY, USA).
Results
A total of 2500 sets of questionnaires were distributed, and 987 were completed and returned for analysis. The calculated response rate (based on the numbers of circulated and gathered questionnaires) was 39.5%, and many of the respondents were from 15 (20%) and 17 (21.6%) year age groups. Summary of the results is shown in Table 1. Mean age of respondents was 15.5±2.5 years, and 54.6% were females. For race, the majority of the respondents was Malay (47.3%), followed by Chinese (39.4%) and Indian (7.3%). Respondent demographics are summarised in Table 2.
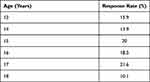 |
Table 1 Response Rate Following Age |
 |
Table 2 Demography of Respondents |
Among the 987 respondents, 98 (9.9%) were CL wearers and dominated by females (78.6%). The main factors for wearing CL were cosmesis (40.8%) and comfort compared with spectacle use (32.7%). Approximately 17.3% have been wearing their CLs for more than 1 year. Approximately 57.2% obtained their lenses from local optical/optometry practices, and 14.2% obtained their lenses from beauty accessory shops (shops that sell cosmetics and jewelleries). The majority of CL wearers (92.9%) were wearing soft CLs, but 97.1% of them were not aware of the brand or trade name of their lenses. For the duration of lens wear, approximately 82.7% of the students wear their lenses between 8 and 10 hours daily, and 5.1% wear their lenses continuously (extended wear basis) for a week before removing them. For CL care, chemical system was the most preferred method of lens care (82.7%), followed by hydrogen peroxide (15.3%) and others (saline/tap water only) (2%). Approximately 90.8% of the wearers claimed that they clean their CL every day, but only 70.4% of them admitted soaking their lenses overnight for disinfection purposes. For lens rinsing, 49% of wearers rinse their CL with saline, followed by multipurpose solutions (32.6%) and tap water (18.4%). The majority of the CL wearers (95.9%) never share their CL with anyone, but a small percentage (4.1%) admitted that they did.
Knowledge on CL wear and care was assessed in all respondents. Around 69.2% of the respondents were not aware that saline cannot be used to disinfect lenses, and 12% thought that tap water can be used to rinse CLs. Nearly 42.4% of them were not aware that soft CL wearers are at higher risks of getting corneal infections than rigid gas permeable (RGP) CL wearers, and only 31.6% of them knew that CL wearers require follow up examination at least 12 months after wearing CL. Summary of the survey results is shown in Table 3.
 |
Table 3 Summary of Survey Results |
Discussion
The pattern and awareness of CL wear and care among secondary school students in Kuala Lumpur is demonstrated in this study. Despite being reminded twice by their respective teachers, the response rate was only 39.5% probably due to minimal interactions between students and researchers throughout the study. The low response rate in a questionnaire research indicates the respondents’ disinclination, communication barriers and inability for the investigators to contact the respondents.16 In this study, the questionnaires used were in Bahasa Malaysia, the national language, and the selected schools were located in Malay dominated areas to minimise communication barrier issues. However, researchers had limited contact with the students due to school regulations, thus influencing their understanding and willingness to participate in the survey.
The results also showed unequal distribution of respondents following age with the minimum response from the 18-year group because the number of 18 year students in secondary schools was lower than that in other age groups. In Malaysia, secondary education is compulsory for 13- to 17-year-old children. Students can choose to take a preparatory course after completion of secondary education, before pursuing high education in universities or colleges. The number of students who chose this option is small, thus influencing the outcome of this study.
In this study, the prevalence of CL wear was 9.9%. However, selection bias might have been introduced due to the low response rate (39.5%). A high prevalence might have been achieved had many CL wearers participated in the survey. The percentage of myopic school children in urban areas in Malaysia has increased over the years due to multiple factors17,18 thus, the number of teenage CL wearers is also expected to grow. For CL demographics, the majority of CL wearers were females, and this correlates well with cosmesis as the main factor of wearing CL in this survey (40.8%). Majority of the respondents wear soft CL, which is consistent with earlier survey findings indicating that Optometrists in Malaysia are likely to prescribe soft CLs rather than RGP to their patients due to shorter chair time and initial comfort.10 Daily wear (monthly disposable) was the most popular modality of CL wear among the respondents possibly due to its lower price compared with other modalities in Malaysia.
Safety is one of the major concerns among eye care practitioners about prescribing CLs to teenagers. According to a survey conducted in the US, the following reasons are given by optometrists to fit CLs in teenagers: availability of daily disposable lenses, improved CL materials, requests from child or parent and children’s participation in sporting activities.19 Nevertheless, this study showed that nearly 43% of the teenage CL wearers in Kuala Lumpur purchased their lenses from unlicensed vendors such as beauty accessory shops, night markets, internet and friends. This phenomenon is worrying because patients who acquire their CLs from unlicensed vendors might not have acquired accurate instructions on proper lens use and care and are at risks of eye inflammation and vision threatening infections.20,21 This is evident by the higher number of reported cases about ocular complications pertaining to wearing CLs purchased without valid prescription or from unlicensed vendors than patients who obtained CLs through conventional means (Optometry/Optical outlets).21,22 Nevertheless, Mingo–Botin et al23 found no differences in compliance or risk awareness between those purchasing CLs exclusively online or other CL wearers. However, the authors noted an association between the growing frequency of self-taught initiation in CL wear among online customers and decreasing frequency of eye examination, which indicates poor compliance and increased risk. Training in the safe use of CLs is an integral part of CL fitting; therefore, the unavailability of eye care practitioners whom the patient can consult in case of problems could delay the treatment and lead to aggravated complications.24,25
The results reflected the risks of getting eye inflammation due to poor lens care. Approximately 18.4% of the CL wearers admitted to rinsing their lenses using tap water, and 4.1% shared their lenses with friends. Sharing of non-corrective CLs for cosmetic purposes is one of the strong risk factors for developing CL-related keratitis.25 Although the number of cosmetic CL wearers has not been identified in this study, sharing of any type of CLs can be associated with eye abrasions due to ill-fitting lens rubbing against the eye and eye infections due to cross contamination. Infections in patients with CL-related Acanthamoeba keratitis have been associated with the use of tap water in CL handling, swimming and showering with CLs.25–27 For these reasons, the teenage CL wearers in this study are at high risk of acquiring keratitis and reduced vision due to CL wear.
In most case reports regarding CL-related inflammation, the main risk factors are the absence of lens fitting and education about lens handling, hygiene and follow up care. Lack of knowledge on CL usage and care is evident in this study. More than 50% of the respondents were not aware of the correct way of handling CLs and did not understand the importance of follow-up examination. This phenomenon is of concern. Although CL is regulated as a medical device in Malaysia and can only be prescribed by optometrists and ophthalmologists, the percentage of CL wearers who purchased their CLs from unlicensed vendors is still high. This finding implies that the strategies implemented to improve safe use of CL wear have not been fully successful. Aggressive measures are needed to address this issue. Most CL-related complications can be avoided through the acquisition of basic CL knowledge from eye care professionals.22 However, controlling illegal internet sales of CLs (without prescription) remains a global challenge. Purchasers have been able to bypass prescription verification with a large United States-based online CL retailer by exploiting the verification system.28 Therefore, improved public health education and supervision of CL users are recommended to improve this situation.
Conclusion
The prevalence of CL wear among secondary school students in Kuala Lumpur is 9.9%. Majority of the CL wearers were females, and their main reason for wearing CLs is for cosmesis purposes. Soft CL is the favourite type of CL, and daily wear (monthly disposable) is the preferred modality among wearers. However, the level of knowledge about CL wear and care is insufficient. Therefore, health communication strategies and aggressive public health education that can influence behaviour changes in teenagers are necessary.
Abbreviations
CL, contact lens; RGP, rigid gas permeable; SD, standard deviation.
Acknowledgments
Both authors would like to acknowledge the teachers and students who were involved in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Walline JJ, Lorenz KO, Nichols JJ. Long-term contact lens wear of children and teens. Eye Contact Lens. 2013;39(4):283–289. doi:10.1097/ICL.0b013e318296792c
2. Rah MJ, Walline JJ, Jones-Jordan LA, et al. Vision specific quality of life of pediatric contact lens wearers. Optom Vis Sci. 2010;87(8):560–566. doi:10.1097/OPX.0b013e3181e6a1c8
3. Jones-Jordan LA, Chitkara M, Coffey B, et al. Comparison of spectacle and contact lens wearing times in the ACHIEVE Study. Clin Exp Optom. 2010;93(3):157–163. doi:10.1111/j.1444-0938.2010.00480.x
4. Efron N, Morgan PB, Woods CA. The international contact lens prescribing survey consortium. Survey of contact lens prescribing to infants, children and teenagers. Optom Vis Sci. 2011;88(4):461–466. doi:10.1097/OPX.0b013e31820efa0f
5. Efron N, Morgan PB, Woods CA, Santodomingo-Rubido J, Nichols JJ. Survey of contact lens fitting for myopia control in children. Cont Lens Anterior Eye. 2020;43(1):4–8. doi:10.1016/j.clae.2019.06.008
6. Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci. 2016;94(96):638–646. doi:10.1097/OPX.0000000000001078
7. De Oliveira PR, Temporini-Nastari ER, Alves MR, et al. Self-evaluation of contact lens wearing and care by college students and health care workers. Eye Contact Lens. 2003;29(3):164–167. doi:10.1097/01.ICL.0000072829.76899.B5
8. Robertson DM, Cavanagh HD. Non-compliance with contact lens wear and care practices: a comparative analysis. Optom Vis Sci. 2011;88(12):1402–1408. doi:10.1097/OPX.0b013e3182333cf9
9. Ismail LA, Rampal L, Abdul Rahman H, et al. Risk factors associated with contact lens related microbial keratitis. Malaysian J Med Health Sci. 2016;12(1):1–8.
10. Cope JR, Collier SA, Nethercut H, et al. Risk behaviors for contact lens related eye infections among adults and adolescents – United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(32):841–845. doi:10.15585/mmwr.mm6632a2
11. Mohidin N, Lee TF. A survey of optometric contact lens prescribing in Malaysia. JSKM. 2009;7(2):59–72.
12. Morgan P, Woods C, Tranoudis I, et al. International contact lens prescribing 2014. Cont Lens Spectr. 2015;30:28–33.
13. Pan CW, Dirani M, Cheng CY, et al. The age specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci. 2015;92(3):258–266. doi:10.1097/OPX.0000000000000516
14. Mohidin N, Zaimuri BL. Survey of contact lens care among contact lens wearers in Kuala Lumpur. JSKM. 2012;10(1):41–48.
15. Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607–610. doi:10.1177/001316447003000308
16. Bowling A. Mode of questionnaire administration can have serious effects on data quality. Int J Public Health. 2005;27(3):281–291.
17. Saw S, Goh P, Cheng A, et al. Ethnicity-specific prevalence of refractive errors vary in Asian children in neighbouring Malaysia and Singapore. Br J Ophthalmol. 2006;90(10):1230–1235. doi:10.1136/bjo.2006.093450
18. Yahya AN, Sharanjeet-Kaur ASM, Akhir SM. Distribution of refractive errors among healthy infants and young children between the age of 6 to 36 months in Kuala Lumpur, Malaysia – a pilot study. Int J Environ Res Public Health. 2019;16(4730):2–11. doi:10.3390/ijerph16234730
19. Sindt CW, Riley CM. Practitioner attitudes on children and contact lenses. J Optom. 2011;82(1):44–45. doi:10.1016/j.optm.2010.11.001
20. Lim CHL, Carnt NA, Farook M, et al. Risk factors for contact lens related microbial keratitis in Singapore. Eye. 2015;30:477.
21. McNally JJ, Chalmers RL, McKenney CD, et al. Risk factors for corneal infiltrative events with 30-night continuous wear of silicone hydrogel lenses. Eye Contact Lens. 2003;29(1):S153–156. doi:10.1097/00140068-200301001-00042
22. Young G, Young AGH, Lakkis C. Review of complications associated with contact lenses from unregulated sources of supply. Eye Contact Lens. 2014;40(1):58–64. doi:10.1097/ICL.0b013e3182a70ef7
23. Mingo-Botin D, Zamora J, Arnalich-Montiel F, et al. Characteristics, behaviours and awareness of contact lens wearers purchasing lenses over the internet. Eye Contact Lens. 2020;46(4):208–213. doi:10.1097/ICL.0000000000000702
24. Wagner H, Richdale K, Mitchell GL, et al. Age, behaviour, environment and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014;91(3):252–261. doi:10.1097/OPX.0000000000000164
25. Lee JS, Hahn TW, Choi SH, et al. Acanthamoeba keratitis related to cosmetic contact lenses. Clin Experiment Ophthalmol. 2007;35(1):775–777. doi:10.1111/j.1442-9071.2007.01622.x
26. Anger C, Lally JM. Acanthamoeba: a review of its potential to cause keratitis, current lens care solutions disinfection standards and methodologies, and strategies to reduce patient risk. Eye Contact Lens. 2008;34(5):247–253. doi:10.1097/ICL.0b013e31817e7d83
27. Chalmers RI, Wagner H, Mitchell GI, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) Study. Invest Ophthalmol Vis Sci. 2011;52(9):6690–6696. doi:10.1167/iovs.10-7018
28. GetLenses.co.uk. No prescription? No problem. Available from: http://www.getlenses.co.uk/no-prescription/.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
