Back to Journals » Clinical Ophthalmology » Volume 13
Visual Outcomes, Visual Quality and Patient Satisfaction: Comparing a Blended Bifocal Approach to Bilateral Extended Depth of Focus Intraocular Lens Implantation
Authors Hammond MD, Potvin R
Received 28 September 2019
Accepted for publication 14 November 2019
Published 27 November 2019 Volume 2019:13 Pages 2325—2332
DOI https://doi.org/10.2147/OPTH.S232800
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Matthew D Hammond,1 Richard Potvin2
1Swagel Wootton Eye Institute, Mesa, AZ, USA; 2Science in Vision, Akron, NY, USA
Correspondence: Richard Potvin 6197 Dye Road, Akron, NY 14001, USA
Tel +1 407-697-6008
Email [email protected]
Purpose: To compare visual outcomes, quality of vision and patient satisfaction between a blended apodized diffractive bifocal lens combination and bilateral implantation of an extended depth of focus intraocular lens (IOL).
Patients and methods: Subjects implanted with either the blended bifocal (Blended) or bilateral extended depth of focus (EDOF) IOL combinations were examined 3 to 24 months after second eye surgery. The primary outcome measure was the patient’s best distance-corrected near visual acuity (VA) at 40cm. The secondary outcome measures were scores on the Quality of Vision Survey, the Catquest-9SF and the Visual Functioning Questionnaires, uncorrected binocular intermediate and near VA at 4–6m, 60cm and 40cm, the manifest refraction and the best-corrected monocular and binocular distance VA.
Results: Twenty-five EDOF subjects and 23 blended subjects were analyzed. The uncorrected and best-distance corrected intermediate VA was statistically significantly better in the EDOF group (p < 0.05); no other significant differences were noted at distance or near. The EDOF group had significantly higher percentage of patients having no difficulty with hobbies and handicrafts (p < 0.05). Eighty-seven percent of the blended subjects and 79% of the EDOF subjects were “very” or “fairly” satisfied with their vision (p = 0.52). The frequency, severity and degree of bother from visual disturbances were comparable between the two groups; however, more subjects in the EDOF group reported severe disturbances (36% vs 4%).
Conclusion: Distance and near VA are similar with both IOL designs, but intermediate VA was better with the EDOF IOL resulting in lower difficulty with intermediate tasks such as hobbies and handicrafts. Despite the difference at intermediate VA, satisfaction was similar between the two groups and there were greater reports of severe visual disturbances in the EDOF group.
Keywords: ReSTOR, Symfony, multifocal, extended range of vision, cataract surgery
Plain Language Summary
This study was designed to compare two groups of patients who had cataract surgery that was designed to provide distance, intermediate and near vision after cataract surgery. The “blended bifocal” group included patients who had a low addition bifocal implanted in one eye, for intermediate vision such as computer work, and a higher addition bifocal implanted in the other eye for near work. The “extended depth of focus” or EDOF group had the same lens implanted in both eyes. The EDOF lens uses optical principles to try to increase the depth of focus in the eye such that the patient can see well at distance and intermediate, but generally not quite as well at near. This is because there is a limit to how much one can extend the optical focus without introducing other problems. Of interest in this study was the patients’ ability to see at distance, intermediate and near in both groups. Also, of interest was their perception of the quality of their vision and their overall satisfaction. We found that overall satisfaction and quality of vision were generally good, with the EDOF group having better computer viewing distance but a slightly higher rate of severe disturbances.
Introduction
Success after multifocal lens implantation is determined by the satisfaction of the patient with their uncorrected vision; the goal is clear and comfortable vision across a range of distances with no restrictions to the patient’s daily activities and minimal visual disturbances. A systematic review by Wang et al in 2017 noted high patient satisfaction with 68% (in 1994) to 94% (in 2004) very/highly satisfied or satisfied with their multifocal intraocular lens (IOL).1,2 A meta-analysis by Rosen et al noted that visual clarity as well as photic phenomena due to residual refraction, opacification of the posterior capsule, large pupil diameter and dry eye most significantly impacted patient satisfaction after multifocal lens implantation.3
One of the most commonly used multifocal intraocular lens is the bifocal ReSTOR IOL (SN6AD1, Alcon, Fort Worth, Texas, USA); it corrects distance and near vision using a +3.00 D add at the IOL plane or about 2.25D at the corneal plane. Satisfaction with these IOLs when binocularly implanted has been reported to be at a mean of about 7/10.4 The most common visual quality complaints were related to haloes, glare and focusing difficulties in 10%, 15% and 8% of the patients, respectively.5 Part of this could be attributed to reduced intermediate vision; more than half of the patients implanted with this bifocal IOL had intermediate vision worse than 20/25.4 Another ReSTOR bifocal IOL (SV25T0, Alcon, Fort Worth, Texas, USA) provides a lower +2.50 D add (about 1.6D at the corneal plane), improving intermediate visual acuity (VA).6 The ReSTOR +3.00 D add lens provides good near VA and the ReSTOR +2.5 add provides good intermediate VA; combining the two lenses (blended bifocal) without taking into account eye dominance has been noted to significantly improve intermediate vision with only nominal effects on near vision.7 A study by Nuijts et al8 compared implanting the lower add lens bilaterally with the blended implantation (the +2.50 D add lens in the dominant eye and the +3.00 D add lens in the non-dominant eye) and found that visual distortions were slightly less in the blended group. This is despite the fact that previous studies noted that the ReSTOR +2.5 had slightly lower higher-order aberrations and less reported glare when compared to the +3.0D lens when implanted binocularly.6,7
Another lens option that aims at extending the depth of focus while minimizing visual distortions is the Tecnis Symfony IOL (Johnson & Johnson Vision, Santa Ana, CA, USA). Results have shown that when both eyes had a near plano refraction postoperatively, the percentage of eyes with no or occasional halos and glare were 93% and 96%, respectively.9 In the same study, the median satisfaction score was 9/10 for distance and intermediate and 8/10 for near.9 In another published study where the target was emmetropia in both eyes, 94% reported minimal or no photic phenomena at 4–6 months postop with a median satisfaction score of 9/10 for distance vision and near and 10/10 for intermediate vision.10 A study of the same lens by Tarib et al noted that halos and glare were observed by 70% and 30% of the patients, respectively.11 Mean VA has also been reported in the literature. Uncorrected distance visual acuity (UDVA) ranged from −0.0411 to 0.08 logMAR12 with a target of emmetropia. Distance-corrected intermediate VA (DCIVA) was 0.19 logMAR12 and the best distance-corrected near VA (DCNVA) ranged from 0.3211 to 0.33 logMAR.12
A previous meta-analysis compared EDOF with other multifocal lenses and noted similar objective results in terms of UDVA, with more variability at intermediate and near.2 The purpose of the current study was to evaluate near vision and patient satisfaction with the ReSTOR +2.5/+3.0 “blended vision” modality vs bilateral implantation of the Tecnis Symfony® IOL, and to check for correlations between satisfaction and uncorrected vision (at distance, intermediate and near) and refractive error.
Patients and Methods
This was a non-interventional two-arm comparative study of visual outcomes after successful bilateral cataract surgery or refractive lens exchange surgery. The study was approved by Salus IRB (Austin, TX) and all eligible subjects signed an approved informed consent document. The study was conducted in a manner consistent with the requirements of the Declaration of Helsinki.
Subjects were assessed during a single visit between 3 and 24 months after their surgery. The primary measure of interest was the patient’s best distance-corrected near vision at 40cm. Also, of interest were scores on the Quality of Vision Survey, which measures the frequency, severity and degree of bother associated with ten different visual phenomena (e.g. glare, halos, double vision). Data from two other patient satisfaction questionnaires (the Catquest-9SF questionnaire and the National Eye Institute Visual Functioning Questionnaire–25 (NEI VFQ-25)) were also collected, along with uncorrected binocular distance, intermediate and near visual acuity (measured at 4–6m, 60cm and 40cm), the manifest refraction, and the best-corrected monocular and binocular distance visual acuity.
Eligible subjects had previous uncomplicated bilateral cataract surgery or refractive lens exchange surgery with one of the following intraocular lens types: ReSTOR +2.5/+3.0 “blended vision” modality (blended group) or bilateral implantation of the Tecnis Symfony® IOL (EDOF group). Surgery must have been performed from 3 to 24 months prior to their study visit. Subjects had to have good ocular health, with no pathology that could compromise visual acuity (outside of residual refractive error), a spherical equivalent manifest refraction from −1.00 to +1.00 with ≤1.25 of the cylinder and a binocular best-corrected distance visual acuity of 0.32 logMAR or better. Subjects with previous surgery or conditions that would confound the results of this investigation were excluded.
The statistical analyses were performed using Statistica, version 12 or higher. All statistical tests of hypotheses employed a level of significance of alpha=0.05. The sample size was calculated for detecting a half-line difference in best distance-corrected near VA, with an alpha of 0.05 and a power of 0.90. A standard deviation in visual acuity of 0.08 logMAR units was presumed, based on previous data analyses for a study of this type. To detect a 3-letter difference in visual acuity (0.06 logMAR units), or just over half a line, will take 39 patients in each group. No dropout is expected because this is a single visit non-interventional study.
Results
A total of 48 subjects were successfully recruited for the study, with 25 EDOF subjects and 23 blended subjects. All surgeries were cataract surgeries except for one blended subject who had a refractive lens exchange. Table 1 summarizes the relevant demographic and pre-examination data. The EDOF subjects had a significantly longer time after surgery, about 6 months longer on average, but all subjects were evaluated between 3 months and 21 months after their second eye surgery, so this difference was not expected to be clinically important. The best distance-corrected near and intermediate visual acuities were collected incorrectly for some subjects (9 EDOF, 7 blended), so the summary data were calculated from the remaining 16 patients in each group. As can be seen, the groups were statistically significantly different in terms of the uncorrected and best distance-corrected intermediate visual acuity, where the EDOF group had an average binocular logMAR acuity around 1.5 lines better than the blended group. There was no correlation between any VA measures and time of follow up (p > 0.05).
 |
Table 1 Demographic and Examination Data by Group |
While mean values are included in Table 1, the distribution of the uncorrected acuity is potentially important in the context of patient satisfaction and quality of vision. Figure 1 shows the cumulative uncorrected binocular visual acuity distribution at distance, intermediate and near, by the IOL group. Using 20/32 (0.2 logMAR) visual acuity as a cutoff point, it can be seen that there were significantly more subjects who had that level of acuity at intermediate in the EDOF group (p = 0.002). The percentage of eyes with 20/32 or better vision at near was higher in the blended group (52% to 32%), but the difference was not statistically significant (p = 0.15). The study inclusion criteria ensured that all eyes had 20/32 or better BCDVA.
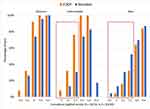 |
Figure 1 Cumulative binocular uncorrected acuity at distance, intermediate and near, by the IOL group. |
The reported satisfaction and overall difficulty with vision responses to the CATQuest questionnaire are shown in Table 2. Eighty-seven percent of the blended subjects and 79% of the EDOF group were “very” or “fairly” satisfied with their vision. The difference was not statistically significant (p = 0.52). Only 4% of both groups reported “great” overall difficulty with their vision, with one EDOF subject not sure. Figure 2 shows the percentage of subjects in each group reporting “No” difficulty with the different tasks listed in the CATQuest questionnaire. There were no statistically significant differences between groups in the percentage having no difficult except for “Hobbies” and “Handicrafts”, where the EDOF group had a significantly higher percentage (p = 0.04 in both cases).
 |
Table 2 Summary of CATQuest Results |
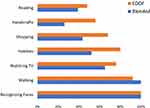 |
Figure 2 CATQuest questionnaire: percentage of subjects reporting “No” difficulty by task and group. |
The Visual Function Questionnaire (VFQ) asks respondents about difficultly with overall visual function and specific tasks; task includes driving and driving at night as well as near and intermediate activities. Figure 3 shows the percentage of subjects in each group who reported “No” or “Little” difficulty with the tasks that appeared most challenging. There were no statistically significant differences between the two groups with regard to any of the tasks; 72% of EDOF subjects and 70% of blended subjects reported “No” or “Little” difficulty with their overall visual function.
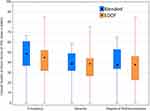 |
Figure 3 VFQ questionnaire: percentage of subjects reporting “No” or “Little” difficulty by task and group. |
Finally, the Quality of Vision Questionnaire reports on the frequency, severity and degree of bother associated with various visual disturbances. Figure 4 shows a box plot of the Rasch-scored results overall. The box contains the middle 50% of subjects and the black central point is the value for the median patient. There was no statistically significant difference in either the frequency (p = 0.85), severity (p = 0.90) or degree of bother (p =0.65) of the aggregate visual disturbances. Table 3 shows the number of subjects reporting higher frequencies of Glare, Haloes and Starbursts, and the associated severity of the complaints. While the numbers are generally similar, only one subject in the blended group reported severe Haloes and none reported severe Glare or Starbursts while there were nine reports of severe disturbances in the EDOF group in these three categories. This difference was statistically significant (p = 0.01).
 |
Table 3 Glare, Haloes and Starburst Frequency and Severity by Group |
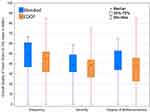 |
Figure 4 Quality of Vision questionnaire: aggregate results by group. |
Discussion
While binocular distance and near VA were similar between the two groups, the average and the distribution of uncorrected intermediate VA was better for the EDOF lens. The visual acuity results in the current study for the blended group are lower than those reported by Nuijts et al,8 who noted similar UDVA but better intermediate and near VA (BDIVA of 0.10 vs 0.28 and BDNVA of 0.11 vs 0.25); it is not clear why the results in the current study are worse at intermediate and near when compared with other studies.7,8 The visual acuity results for the EDOF lens at distance and intermediate are reasonably consistent with previous studies.11,12
In terms of satisfaction, visual function and the difficulty in performing certain tasks, both groups had similar results but the EDOF group had more subjects reporting no difficulty for “Hobbies” and “Handicrafts.” Both hobbies and handicrafts are likely to be performed at arms’ length, thus favoring the lens with the better VA at intermediate. Despite the lower VA at intermediate in the blended group, their overall satisfaction was slightly higher, with 8% more reporting being “very” or “fairly” satisfied with their vision when compared to the EDOF group. Similar satisfaction results have been reported previously for the blended IOL.7 A small percentage of subjects reported difficulty with their vision. This highlights the fact that multifocal and EDOF lenses are not a perfect solution; appropriate patient selection remains important to ensure high levels of satisfaction with their use.
Figure 4 illustrates that the frequency, severity and degree of bother from visual disturbances were comparable between the two groups; however, more subjects in the EDOF group reported severe disturbances (36% or 9/25 vs 4% or 1/23). The level of visual disturbances in both groups appears somewhat higher than has been previously reported for the blended IOL modality8,13 and the EDOF lens.9,10 These much lower previously reported results for the blended implantation modality were both from studies in Europe, while the current data are from a site in the southwest United States. It is possible that there is a cultural component to these findings.
There are limitations to the current study. There was a relatively low number of subjects in each group. In addition, while exclusion and inclusion criteria were used to qualify subjects, the data were collected from subjects that had surgery in the past. It was therefore not possible to match subjects preoperatively. Finally, the postoperative follow-up time was slightly longer in the EDOF subjects. However, as noted, all subjects were seen between 3 months and 21 months after surgery, so we do not believe this was a significant clinical difference, particularly given the inclusion and exclusion criteria applied. There is the potential that subjects with longer follow-up times might have greater neuroadaptation to the multifocal/EDOF lens modalities, though we saw no correlation between follow up time and any visual acuity measure. A larger sample size might have shown differences. Subsequent studies of subjects with follow-up around 12 months post-surgery, with less variability in follow-up time, might be interesting in this regard.
Conclusion
Outcomes of the current study suggest that while distance and near VA are similar with both IOL designs, intermediate VA was better with the EDOF IOL. The improvement in intermediate VA resulted in lower difficulty with intermediate tasks such as hobbies and handicrafts. Despite the difference in intermediate VA, satisfaction was similar between the two groups, though there were greater reports of severe visual disturbances in the EDOF group.
Acknowledgments
Amy Crump, OD of Swagel Wooten Eye Institute, assisted in the data collection for this study. Sarah Makari, OD of Science in Vision aided in the preparation of this manuscript.
Disclosure
Swagel Wootton Eye Institute (Hammond) received an investigator-initiated trial grant from Alcon (Fort Worth, TX) to conduct the study: IIT#41669787. Science in Vision received funding from Swagel Wootton Eye Institute to assist in preparing the study and the resulting manuscript. Dr Richard Potvin reports personal fees from Alcon, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27(4):387–401. doi:10.5301/ejo.5000978
2. Negishi K, Hayashi K, Kamiya K, Sato M, Bissen-Miyajima H, Survey Working Group of the Japanese Society of Cataract and Refractive Surgery. nationwide prospective cohort study on cataract surgery with multifocal intraocular lens implantation in Japan. Am J Ophthalmol. 2019;208:133–144. doi:10.1016/j.ajo.2019.07.019
3. Rosen E, Alió JL, Dick HB, Dell S, Slade S. Efficacy and safety of multifocal intraocular lenses following cataract and refractive lens exchange: metaanalysis of peer-reviewed publications. J Cataract Refract Surg. 2016;42(2):310–328. doi:10.1016/j.jcrs.2016.01.014
4. Guo X, Sun Y, Zhang B, Zheng D. Medium-term visual outcomes of apodized diffractive multifocal intraocular lens with +3.00 d addition power. J Ophthalmol. 2014;2014:247829.
5. Maurino V, Allan BD, Rubin GS, Bunce C, Xing W, Findl O, Moorfields IOL Study Group. Quality of vision after bilateral multifocal intraocular lens implantation: a randomized trial–AT LISA 809M versus AcrySof ReSTOR SN6AD1. Ophthalmology. 2015;122(4):700–710. doi:10.1016/j.ophtha.2014.10.002
6. Pedrotti E, Mastropasqua R, Passilongo M, Parisi G, Marchesoni I, Marchini G. Comparison of two multifocal intraocular lens designs that differ only in near add. J Refract Surg. 2014;30(11):754–760. doi:10.3928/1081597X-20141021-07
7. Mastropasqua R, Pedrotti E, Passilongo M, Parisi G, Marchesoni I, Marchini G. Long-term visual function and patient satisfaction after bilateral implantation and combination of two similar multifocal IOLs. J Refract Surg. 2015;31(5):308–314. doi:10.3928/1081597X-20150423-04
8. Nuijts RM, Jonker SM, Kaufer RA, et al. Bilateral implantation of +2.5 D multifocal intraocular lens and contralateral implantation of +2.5 D and +3.0 D multifocal intraocular lenses: clinical outcomes. J Cataract Refract Surg. 2016;42(2):194–202. doi:10.1016/j.jcrs.2016.02.009
9. Cochener B. Influence of the level of monovision on visual outcome with an extended range of vision intraocular lens. Clin Ophthalmol. 2018;12:2305–2312. doi:10.2147/OPTH
10. Sachdev GS, Ramamurthy S, Sharma U, Dandapani R. Visual outcomes of patients bilaterally implanted with the extended range of vision intraocular lens: a prospective study. Indian J Ophthalmol. 2018;66(3):407–410. doi:10.4103/ijo.IJO_813_17
11. Tarib I, Kasier I, Herbers C, et al. Comparison of visual outcomes and patient satisfaction after bilateral implantation of an EDOF IOL and a mix-and-match approach. J Refract Surg. 2019;35(7):408–416. doi:10.3928/1081597X-20190417-02
12. Pedrotti E, Bruni E, Bonacci E, Badalamenti R, Mastropasqua R, Marchini G. Comparative analysis of the clinical outcomes with a monofocal and an extended range of vision intraocular lens. J Refract Surg. 2016;32(7):436–442. doi:10.3928/1081597X-20160428-06
13. Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol. 2016;10:455–461. doi:10.2147/OPTH.S103375
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
