Back to Journals » Clinical Ophthalmology » Volume 16
Vision Quality Questionnaire Assessment in Patients After Topography-Guided Photorefractive Keratectomy for Irregular Astigmatism Secondary to Radial Keratotomy
Authors Colombo-Barboza GN , Colombo-Barboza MN , Colombo-Barboza LR, Colombo-Barboza MM, Colombo-Barboza FDP, Lui-Netto A, Dolci JEL, Moscovici BK , de Freitas D
Received 20 August 2022
Accepted for publication 7 October 2022
Published 19 October 2022 Volume 2022:16 Pages 3491—3501
DOI https://doi.org/10.2147/OPTH.S386009
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Guilherme Novoa Colombo-Barboza,1– 4 Marcello Novoa Colombo-Barboza,1– 3 Luiz Roberto Colombo-Barboza,1 Maria Margarida Colombo-Barboza,1 Fernanda Daroz Paulo Colombo-Barboza,1 Adamo Lui-Netto,2 José Eduardo Lutaif Dolci,2 Bernardo Kaplan Moscovici,1– 3 Denise de Freitas3
1Department of Ophthalmology, Hospital Visão Laser, Santos, Brazil; 2Department of Ophthalmology, Santa Casa de São Paulo, São Paulo, Brazil; 3Department of Ophthalmology and Vision Sciences, Universidade Federal de São Paulo (UNIFESP), São Paulo, Brazil; 4Department of Ophthalmology, Universidade Metropolitana de Santos (UNIMES), Santos, Brazil
Correspondence: Guilherme Novoa Colombo-Barboza, Av. Conselheiro Nebias 355, Santos, SP, CEP 11015-001, Brazil, Tel +55 13 2104-5000, Email [email protected]
Aim: To evaluate the vision-related quality of life with the National Eye Institute Refractive Error Quality of Life (NEI-RQL) questionnaire in patients with astigmatism secondary to radial keratotomy surgery who underwent topography-guided photorefractive keratectomy.
Methods: Prospective non-randomized clinical trial. This study included 15 patients (30 eyes) aged > 21 years, mean age 55.1 (SD, 3.5) years, 53.3% female, with astigmatism ≤ - 6.00 D resulting from radial keratotomy, which could have been associated with hyperopia ≤ + 6.00 D. Photorefractive keratectomy with topography-guided custom ablation treatment was used in all cases. The patients answered the NEI-RQL questionnaire preoperatively and at 4 and 48 months after topography-guided photorefractive keratectomy. The following data were collected: age, sex and education level, pre-operative refraction data, visual acuity with or without correction, pachymetry, and keratometry.
Results: There was a significant difference between pre-and postoperative NEI-RQL scores for the domains clarity of vision, near vision, far vision, diurnal fluctuation, activity limitations, glare, symptoms, correction dependence, appearance, and satisfaction with correction (p < 0.001).
Conclusion: Topography-guided photorefractive keratectomy improved vision-related quality of life in patients with a history of irregular astigmatism secondary to radial keratotomy.
Keywords: quality of life, radial keratotomy, NEI-RQL, topography-guided photorefractive keratectomy
Plain Language Summary
What is already known on this topic?
Topography-guided PRK is a safe and effective procedure in patients with irregular astigmatism secondary to radial keratotomy.
What this study adds.
Topography-guided PRK improved vision-related quality of life in patients with a history of irregular astigmatism secondary to radial keratotomy.
How this study might affect research, practice or policy.
Patients with irregular astigmatism due to RK fear performing new procedures to improve visual quality. With the results of this study, we have more concrete data to present to them.
Introduction
Many patients suffer from reduced vision quality due to corneal surface irregularities, irregular astigmatism, and hyperopia secondary to radial keratotomy (RK). In recent years, surgical techniques have been discussed to improve these patients’ vision quality, including topography-guided custom refractive surgery.1–3
Photorefractive keratectomy (PRK) is a corneal surface ablation procedure involving the corneal epithelium’s mechanical removal followed by excimer laser ablation.4–6
Topography-guided surgery is performed to regularize the cornea in patients after RK and decrease ametropia. The results of the T-CAT study8,9 highlighted the importance of corneal topography for accurate refraction results.
The National Eye Institute Refractive Error Quality of Life (NEI-RQL) was developed to estimate the vision-related quality of life in refractive surgery patients.7,10–12 This questionnaire was translated and validated into Portuguese and was a valuable and reliable tool for assessing the vision-related quality of life in refractive surgery candidates.10–24
Therefore, this study aimed to assess the vision-related quality of life with the NEI-RQL questionnaire, which was applied to patients with irregular astigmatism due to RK 4 and 48 months after topography-guided PRK.
Material and Methods
The Research Ethics Committee of Santa de Casa de São Paulo approved this single experimental study (number 1,730,182). The patients included in this study were informed about the nature of the research and provided written informed consent before inclusion. Our study complies with the Declaration of Helsinki.
Patient Selection
We included men and women aged > 21 years with irregular astigmatism (≤ - 6.00 D) resulting from previous RK surgery, which could have been associated with hyperopia ≤ + 6.00 D, whose surgery and follow-up had taken place at the Refractive Surgery Outpatient Clinic of Santa Casa de São Paulo, São Paulo, Brazil. Exclusion criteria were diabetes, current pregnancy or breastfeeding, amblyopia, previous ocular surgeries besides RK, keratoconus, scars or open incisions from RK, thin corneas (below 460 microns at the thinnest point), crystalline lens opacities, or other ocular diseases.
Surgical Procedure
The surgical technique used in all cases was PRK, with topography-guided custom ablation treatment, associated with mitomycin C 0.02% for 20 to 40s. This system uses maps of each cornea’s height and axial curvature profiles, analyzed with a Topolyzer device (Alcon Wavelight, Fort Worth, TX, USA), which calculates the ablation pattern required to transform the cornea into a spherical surface within the 6-mm optical zone.
This device provides pre-operative topography and a topographic map illustrating the programmed point-by-point ablation. To avoid refractive error, we performed the necessary mapping for the topography-guided ablation and neutralized corneal aberrations Z12 and Z4 according to manufacturer instructions.
The data were then transferred to an Allegretto EX500 excimer laser (Alcon Wavelight, Fort Worth, TX, USA) with eye-tracking control. Finally, we treated the previously obtained cycloplegic refraction.
All surgeries were performed by the same surgeon and involved the same postoperative medications. We prescribed glasses for presbyopic correction for all patients three months after surgery.
Data Collection
The primary variable analyzed in this study was the vision-related quality of life according to the NEI-RQL. This questionnaire consists of 42 multiple-choice questions that evaluate 13 domains: clarity of vision, expectations, near vision, far vision, diurnal fluctuation, activity limitations, glare, symptoms, dependence on correction, worry, suboptimal correction, appearance, and satisfaction with correction. The score for each domain ranges from 0 to 100, and according to the original questionnaire, the higher the score, the better the result. The patients answered the NEI-RQL questionnaire preoperatively and again 4 and 48 months postoperatively.
All patients answered the pre-operative questionnaire with updated glasses.
Data were also collected on patient age, sex, education level, pre-operative refraction and visual acuity with or without correction, pachymetry, and keratometry in the pre-and postoperative periods.
Statistical Analysis
After data collection, descriptive statistical analysis was performed to demographically characterize the patients, pre-and postoperative data related to refractive error (spherical equivalent), and NEI-RQL scores. All continuous data were presented as mean and standard deviation. Data comparisons were performed using Wilcoxon’s and Friedman tests (Kendall’s W value). For all analyses, 95% confidence intervals were used. The analyses were performed in Stata v. 14 (StataCorp, College Station, TX, USA) and SPSS package 26 (IBM SPSS Statistics, Armonk, NY, USA).
The sample size was calculated based on the expected pre- and postoperative differences in NEI-RQL scores. Sample sizes were calculated with an alpha error of 5%, a power of 80%, and a correlation of 0.1 for the main domains of the questionnaire.10,13 The final sample size was 30 eyes, considering a power of 80% and an alpha error of 5%. The calculation was performed in Stata v. 14 (StataCorp, College Station, TX, USA).
The 21 outcomes (13 NEI-RQL domains and eight clinical outcomes) were described in terms of mean and standard deviation according to pre- and postintervention. To compare pre- and early postoperative (four months) scores, the Wilcoxon signed-rank test was used, and Friedman test (Kendall’s W value) was used for pre-and all postoperative scores. The significance level was set at 0.0023 (ie, 0.05/21 outcomes) to reduce the false discovery rate.
Along with the corrected significance level, we assessed the magnitude of the pre-and postintervention differences via the standardized effect size, called DZ, which is calculated by dividing the absolute (positive) standardized Wilcoxon test statistic, z, by the square root of the number of pairs (15). We ranked the magnitude of the effect sizes according to Cohen’s classification: 0.1 (small), 0.3 (moderate), and ≥ 0.5 (large).14
Results
We evaluated 15 patients (30 eyes) with a mean age of 55.1 (SD, 3.5) years, of whom 53.3% were female and 60% had completed university. Tables 1 and 2 show the baseline patient characteristics.
 |
Table 1 Initial Characteristics of the Sample |
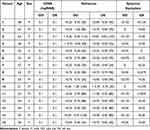 |
Table 2 Post-Operative Characteristics of the Sample After 48 Months |
Questionnaire
Regarding the NEI-RQL items, when comparing the pre-and postoperative assessments with the Wilcoxon signed-rank test, there was a significant difference in clarity of vision, near vision, far vision, diurnal fluctuation, activity limitations, glare, symptoms, dependence on correction, appearance, and satisfaction with correction. The mean pre- and postoperative scores for satisfaction with correction were 44.00 and 85.33, respectively, while those for expectations were 5.00 and 51.67, respectively (Figure 1).
 |
Figure 1 Differences between pre- and postoperative means (4 and 48 months) of each domain of the National Eye Institute Refractive Error Quality of Life questionnaire. |
The domains with the most significant variations in the mean score were: activity limitations, clarity of vision, dependence on correction, satisfaction with correction, appearance, and glare. Those with the slightest variations were: diurnal fluctuation, far vision, near vision and symptoms. Expectations, worry, and suboptimal correction were insignificant after statistical analysis (Table 3).
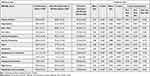 |
Table 3 Comparison of Pre- and Postoperative National Eye Institute Refractive Error Quality of Life (NEI-RQL) Scores (4 and 48 Months) |
A comparison between pre- and postoperative scores (Table 3) showed significant differences for most items (p < 0.0023). However, there were no significant differences between postoperative scores (4 months vs 48 months)(p > 0.0023). It should be pointed out that all items with a p-value < 0.0023 had increased means after four months except the symptoms domain, which reduced from 79.67 (pre-operative) to 72.78 at four months and 72.21 at 48 months).
Regarding the magnitude of the effect sizes (Table 3), all domains had a large effect size postoperatively (> 0.5) except worry (0.503), which was moderate. Those with the most significant effect size were glare and dependence on correction (both 0.897), followed by activity limitations and appearance (0.888 and 0.873, respectively). The domains with the smallest effect size were worry and symptoms (0.503 and 0.562, respectively). Suboptimal correction had a small effect size (0.356), which was non-significant after correction for false discovery rate (p > 0.0023). Thus, all outcomes differed after the intervention except for suboptimal correction and worry.
Visual Outcomes
The mean best corrected visual acuity was 0.144 (SD, 0.04) preoperatively and 0.1 postoperatively, without significant difference. After the refractive surgery, none of the patients lost lines of vision, as shown in Figure 2.
The mean spherical equivalent was 1.76 (SD, 1.14) preoperatively and 0.28 (SD, 0.19) postoperatively (p = 0.045). Since surgery corrected the irregularities and ametropia, uncorrected visual acuity improved or did not change in most eyes (26 of 30 eyes). No patient had visual acuity line loss, and 16 eyes presented improvement in 1 line of best corrected visual acuity (BCVA) (Table 2 and Figure 2).
We also compared our data with normative data from another study with 39 hyperopes who had refractive surgery (Tables 4 and 5).22
 |
Table 4 Comparison of Pre Operative Values of NEI-RQL Items Between Our Data and Normative Data |
 |
Table 5 Comparison of Post Operative Values of NEI-RQL Items Between Our Data and Normative Data |
Discussion
Visual Outcomes
The BCVA, UDVA, astigmatism change and spherical equivalent improvements were probably reflected in the questionnaire, pointing out that either topography-guided or optimized corrections would benefit post-RK patients. Nevertheless, the improved line of vision and increased scores for the glare and clarity of vision domains should encourage surgeons to perform corneal wavefront-guided procedures.
Analyzing the visual outcomes, Ghoreishi et al performed transepithelial topography-guided PRK with a Schwind Amaris laser platform (Schwind eye-tech-solutions GmbH, Kleinostheim, Germany), finding similar visual outcomes in RK patients. The mean BCVA change was similar: < 5% gained 1 line of vision, almost 25% gained two lines of vision, and < 10% gained > 2 lines of vision. However, some of their patients lost vision lines, although none of ours did. In our study, the percentage of eyes that gained 1 line of vision was more significant. The visual acuity of more than 50% of the eyes in our study improved. However, the change in spherical equivalent was very similar between our study and Ghoreishi et al. Nevertheless, they did not apply a visual quality questionnaire.15 Camellin et al performed TG-guided PRK with the same equipment as Ghoreishi et al, but they treated RK and post-keratoplasty patients; both had similar results in the RK groups.16
Ghanem et al performed TG-guided PRK with a different laser platform (MEL-70) but found similar results: 68.4% gained more than 1 line of vision and two eyes lost 1 line of vision. More eyes gained vision lines in this study, although more eyes also lost vision (probably due to corneal haze, which did not occur in our sample). The mean BCVA and spherical equivalent changes were similar. Their study did not involve a visual quality questionnaire.17
Questionnaire Results
To our knowledge, this is the first study of quality of vision assessment, after TG-guided surgery, through the NEI-RQL in irregular corneas secondary to RK. Patients with previous RK surgery commonly report visual satisfaction in their daily lives, although they describe high visual aberrations that vary with ambient light or even the time of day. In contrast, others with the same visual aberrations report continuous dissatisfaction with their vision. Thus, subjective patient opinions must be considered and can be suitably measured in the NEI-RQL.
In the present study, the data from each domain were analyzed separately, rather than the total questionnaire scores, since the items evaluate daily situations and difficulties. Globalizing scores with significant results and those that do not have the same significance level may mask the importance of some domains since all parameters increased, but not all did so significantly. We should also point out that we could find no standards identifying which scores or domain increases can be considered average, above average, or excellent. An increased score does not necessarily express effective clinical improvement.
Analyzing the scores separately, we can draw uncertain conclusions. For example, the score change in the expectations domain was non-significant (p = 0.005), despite varying almost 50 points between the pre-and postoperative measurements (5.00 [SD, 10.35] vs 51.67 [SD, 42.75], respectively). The suboptimal correction domain, which did not change significantly (p = 0.20), increased by 10 points (70.83 [SD, 9.05] vs 80.00 [SD, 34.00], pre- and postoperatively, respectively). So, the higher questionnaire scores do not necessarily indicate significant effects in particular domains.
The higher the scores, the better the quality of life in the population through the NEI-RQL questionnaire. In our study, only symptoms and worry had lower values postoperatively. We think patients were more concerned that the visual improvement could decrease with time, such as with the RK surgery. We also hypothesized that symptoms increased after surgery because it was the second refractive surgery, and the decreased corneal sensibility could be responsible for this result.
Our results were similar to those of Nunes & Schor10 regarding overall score increase. However, their study was performed in a different population: patients that underwent standard refractive procedures without previous surgeries or irregular astigmatism. Nichols et al studied regular myopic patients before and after LASIK surgery. They found that compared to patients who were not seeking surgery, some domains such as satisfaction, appearance, activity limitations and expectations were lower in patients seeking surgery, indicating that the mentality of patients seeking surgery could influence some items of this test.18,23
Some studies compared this questionnaire in patients who use contact lenses, spectacles and refractive surgery and found some differences, but these data were difficult to compare with our results since the population studied was different.20,21
McDonnell et al studied the questionnaire in myopic and hyperopic patients who underwent refractive correction. In the total population, all the scores improved except for clarity of vision and glare. In our study, these domains improved, probably due to the correction of irregular astigmatism. When he studied hyperopic patients, only the domains appearance, dependence on correction and expectations improved, indicating that the hyperopic correction in typical cases does not produce the same satisfaction that myopic patients and pointing that the significant improvement in the questionnaire should be due to the irregular astigmatism correction.22
We also performed statistical analysis with the normative data from the McDonnell study. It has limitations because the normative data was composed of normal eyes without irregular astigmatism, reflecting on lower values of almost all pre operative values. Comparing the questionnaire scores in pre-operative values, only the domains expectations, symptoms and dependence on correction did not have statistically significant differences. Comparing the postoperative values, we found statistically significant differences in expectations, far vision, symptoms, diurnal fluctuations, worry and satisfaction with correction. Our sample’s only domains that had superior values were satisfaction with correction, diurnal fluctuations, and expectations. This difference could be because we performed surgery with irregular corneas with worse vision than usual, as evidenced by the worst quality of vision preoperatively, so this comparison is extremely limited. When we look at the improvement of the scores between these two samples, we can observe that the improvement was far superior in some domains as clarity of vision, far vision, activity limitations and glare, suggesting significant improvement in quality of life in patients with irregular astigmatism secondary to RK with TG guided surgery.22
Sia et al studied the same questionnaire in militaries who underwent refractive surgery and found significant improvement in the questionnaire: scores were significantly higher postoperatively for the subscales clarity of vision, expectations, near vision, far vision, diurnal fluctuations, activity limit, glare, dependence on correction, worry, appearance, and satisfaction with correction (all P < 0.001), but not for symptoms after refractive surgery (P = 0.403). This studied population consisted of regular myopic patients, and in this population, the surgery was proved to improve the domain score. The difference in our study is that this is the first study in hyperopic patients with a significant improvement, especially in patients with irregular astigmatism secondary to RK who underwent TG-guided surgery.23
We must look deeper at the visual outcomes to analyze the questionnaire results. More than half of the eyes (16/30) had improvement in 1 line of vision so we would expect improvement in the domains glare, clarity of vision, activity limitations, far vision, satisfaction with correction, and symptoms. Moreover, since BCVA, UDVA, astigmatism correction and spherical equivalent improved in most eyes, we should expect improvement in the dependence on the correction domain.
Based on these reflections, we found the questionnaire data similar to our assumptions except for the diurnal fluctuation domain, which was not expected to show significant improvement. Because we performed topography-guided surgery to improve visual quality and acuity, successful treatment was expected to improve glare and clarity of vision due to decreased high-order aberrations.
Although there were postoperative improvements in BCVA and vision line gains, they were not statistically significant, suggesting that isolated parameters do not represent an objective alteration in patient vision, which is usually analyzed quantitatively using the Snellen table or through refraction. Thus, we suggest alternative paths to demonstrate improvement in the quality of vision through a questionnaire or qualitative vision assessment, such as ocular aberrometry or a contrast sensitivity test.
Our study was limited by its small sample size because this procedure had not been performed for refractive correction for more than 30 years. Many patients who underwent RK had already undergone cataract or laser refractive surgery, which made meeting the study’s inclusion and exclusion criteria very difficult. Randomized clinical trials can more accurately show these surgeries’ clinical outcomes and safety, and the NEI-RQL can be used to measure vision quality in future trials. Studies with a control group and comparing topography-guided with optimized procedures should bring more information in the future.
Conclusion
Regarding the vision-related quality of life of patients with irregular astigmatism due to RK surgery, there was a significant improvement in the majority of NEI-RQL scores between assessments before and after (4 and 48 months) topography-guided PRK.
Ethics Approval Statement
The Research Ethics Committee of Santa de Casa de São Paulo approved this single experimental study (number 1,730,182) and UNIFESP number 1189924/2020.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; they took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Choi DM, Thompson RW, Price FW. Incisional refractive surgery. Curr Opin Ophthalmol. 2002;13(4):237–241. doi:10.1097/00055735-200208000-00009
2. Bates WH. A suggestion of an operation to correct astigmatism. Refract Corneal Surg. 1989;5(1):58–59. doi:10.3928/1081-597X-19890101-20
3. Hjortdal JO, Olsen H, Ehlers N. Prospective randomized study of corneal aberrations 1 year after radial keratotomy or photorefractive keratectomy. J Refract Surg. 2002;18(1):23–29. doi:10.3928/1081-597X-20020101-03
4. Ghanem VC, Ghanem RC, Ghanem EA, Souza DC, Souza GC. Ceratectomia fotorrefrativa baseada em topografia para correção da hipermetropia secundária à ceratotomia radial[Topographically-guided photorefractive keratectomy for the management of secondary hyperopia following radial keratectomy]. Arq Bras Oftalmol. 2007;70(5):803–808. Portuguese. doi:10.1590/s0004-27492007000500014
5. Applegate RA, Hilmantel G, Howland HC. Corneal aberrations increase with the magnitude of radial keratotomy refractive correction. Optom Vis Sci. 1996;73(9):585–589. doi:10.1097/00006324-199609000-00004
6. Waring GO, Lynn MJ, McDonnell PJ. Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery. Arch Ophthalmol. 1994;112(10):1298–1308. doi:10.1001/archopht.1994.01090220048022
7. Hays RD, Spritzer KL. National Eye Institute Refractive Error Quality of Life Instrument (NEI-RQL-42™), Version 1.0: A Manual for Use and Scoring [Internet]. Los Angeles (CA): RAND Corporation; 2002:1–4.
8. Netto MV, Ambrosio R, Chalita MR, Krueger RR, Wilson SE. Resposta cicatricial corneana em diferentes modalidades de cirurgia refrativa[Corneal wound healing response following different modalities of refractive surgical procedures]. Arq Bras Oftalmol. 2005;68(1):140–149. Portuguese. doi:10.1590/s0004-27492005000100027
9. Jankov MR, Panagopoulou SI, Tsiklis NS, Hajitanasis GC, Aslanides M, Pallikaris G. Topography-guided treatment of irregular astigmatism with the wavelight excimer laser. J Refract Surg. 2006;22(4):335–344. doi:10.3928/1081-597X-20060401-07
10. Nunes LM, Cortizo V, Schor P. Validação de versão em língua portuguesa do questionário NEI-RQL como instrumento de avaliação da qualidade de vida relacionada à visão, em candidatos a cirurgia refrativa[Validation of a Portuguese-language version of the NEI-RQL (National Eye Institute Refractive Error Quality of Life) instrument in refractive surgery candidates]. Rev Bras Oftalmol. 2004;63(2):110–118. Portuguese.
11. Berry S, Mangione CM, Lindblad AS, McDonnell PJ. Development of the National Eye Institute refractive error correction quality of life questionnaire: focus groups. Ophthalmology. 2003;110(12):2285–2291. doi:10.1016/j.ophtha.2003.08.021
12. Hays RD, Mangione CM, Ellwein L, Lindblad AS, Spritzer KL, McDonnell PJ. Psychometric properties of the national eye institute-refractive error quality of life instrument. Ophthalmology. 2003;110(12):2292–2301. doi:10.1016/j.ophtha.2002.07.001
13. Nehls SM, Ghoghawala SY, Hwang FS, Azari AA. Patient satisfaction and clinical outcomes with laser refractive surgery performed by surgeons in training. J Cataract Refract Surg. 2014;40(7):1131–1138. doi:10.1016/j.jcrs.2013.11.042
14. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Academic Press; 2013.
15. Ghoreishi M, Peyman A, Koosha N, Golabchi K, Pourazizi M. Topography-guided transepithelial photorefractive keratectomy to correct irregular refractive errors after radial keratotomy. J Cataract Refract Surg. 2018;44(3):274–279. doi:10.1016/j.jcrs.2017.12.015
16. Camellin M, Arba Mosquera S. Simultaneous aspheric wavefront-guided transepithelial photorefractive keratectomy and phototherapeutic keratectomy to correct aberrations and refractive errors after corneal surgery. J Cataract Refract Surg. 2010;36(7):1173–1180. doi:10.1016/j.jcrs.2010.01.024
17. Ghanem RC, Ghanem VC, de Souza DC, Kara-José N, Ghanem EA. Customized topography-guided photorefractive keratectomy with the MEL-70 platform and mitomycin C to correct hyperopia after radial keratotomy. J Refract Surg. 2008;24(9):911–922.
18. Nichols JJ, Twa MD, Mitchell GL. Sensitivity of the national eye institute refractive error quality of life instrument to refractive surgery outcomes. J Cataract Refract Surg. 2005;31(12):2313–2318. doi:10.1016/j.jcrs.2005.04.033
19. Sia RK, Ryan DS, Rivers BA, et al. Vision-related quality of life and perception of military readiness and capabilities following refractive surgery among active duty U.S. Military Service Members. J Refract Surg. 2018;34(9):597–603. doi:10.3928/1081597X-20180723-01
20. Shams N, Mobaraki H, Kamali M, Jafarzadehpour E. Comparison of quality of life between myopic patients with spectacles and contact lenses, and patients who have undergone refractive surgery. J Curr Ophthalmol. 2015;27(1–2):32–36. doi:10.1016/j.joco.2015.10.004
21. González-Pérez J, Sánchez García Á, Villa-Collar C. Vision-specific quality of life: laser-assisted in situ keratomileusis versus overnight contact lens wear. Eye Contact Lens. 2019;45(1):34–39. doi:10.1097/ICL.0000000000000538
22. McDonnell PJ, Mangione C, Lee P, et al. Responsiveness of the National Eye Institute Refractive Error Quality Of Life instrument to surgical correction of refractive error. Ophthalmology. 2003;110:2302–2309. doi:10.1016/j.ophtha.2003.02.004
23. Nichols JJ, Mitchell GL, Saracino M, Zadnik K. Reliability and validity of refractive error-specific quality-of-life instruments. Arch Ophthalmol. 2003;121:1289–1296. doi:10.1001/archopht.121.9.1289
24. Berry S, Mangione CM, Lindblad AS, McDonnell PJ. Development of the National Eye Institute refractive error correction quality of life questionnaire; focus groups; the NEI-RQL Focus Group Investigators. Ophthalmology. 2003;110:2285–2291.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

