Back to Journals » Journal of Blood Medicine » Volume 12
Value of the Direct Antiglobulin Test in Predicting the Need for Phototherapy in Newborns
Authors AlKhater SA , Albalwi RA, Alomar SA , Alsultan AA, Almuhaidib HR, Almousa RA, Alanezi SM, Alghamdi RK, Shash HA
Received 13 November 2020
Accepted for publication 11 January 2021
Published 29 January 2021 Volume 2021:12 Pages 53—61
DOI https://doi.org/10.2147/JBM.S291606
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Suzan A AlKhater,1,2 Rana A Albalwi,2 Sara A Alomar,1 Anfal A Alsultan,1 Halah R Almuhaidib,1 Rahaf A Almousa,1 Sarah M Alanezi,1 Raghad K Alghamdi,1 Hwazen A Shash1,2
1College of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2Department of Pediatrics, King Fahad Hospital of the University, Al-Khobar, Saudi Arabia
Correspondence: Hwazen A Shash
Department of Pediatrics, King Fahd Hospital of the University, Al Khobar 31952, Saudi Arabia
Tel +966540353333
Email [email protected]
Purpose: Guidelines for managing neonatal hemolytic disease of the newborn (HDN) recommend a selective approach in the use of direct antiglobulin test (DAT). In Saudi Arabia, many hospitals still perform routine DAT for all newborns. This study assessed the need for phototherapy in relation to DAT results in full-term healthy newborns.
Patients and Methods: A retrospective analysis of all healthy newborns admitted during 2018 was performed. The primary outcome was the association of positive DAT results with phototherapy.
Results: There were 1463 newborns born during the study period. The DAT was positive at 4.4%. The 24-hour bilirubin levels were higher in DAT-positive cases (P=0.06); however, peak bilirubin levels were not correlated with the DAT results (P=0.717). Thirty-six neonates (2.46%) required phototherapy, and the need was similar among DAT-positive and DAT-negative cases (P=0.271). The most common indication for phototherapy was clinical jaundice in 22 neonates (61.1%), followed by DAT positivity in 12 (33.3%) and hospital protocol in 2 patients (5.6%) (P < 0.01 by chi-square overall comparison).
Conclusion: Our results indicate that factors other than DAT positivity are important in assessing the need for phototherapy in newborns. Clinical signs of jaundice were indicators of high serum bilirubin levels and subsequent phototherapy, further indicating that the DAT test was overused in predicting the need for phototherapy.
Keywords: hemolytic disease of the newborn, neonatal jaundice, neonatology, screening
Plain Language Summary
The direct antiglobulin test (DAT) is still used in many centers as a screening test to assess for the risk of hemolytic disease of the newborn. In this retrospective study of all healthy neonates admitted over a one-year period in a university teaching hospital, we correlated, in maternal-neonate pairs, the positive DAT results with the need for phototherapy in the neonates. The results of the study showed that the clinical evaluation of jaundice is more indicative of a need for phototherapy than the DAT result. In a multivariate analysis, only peak bilirubin and 24-hour bilirubin values were statistically significant for phototherapy. We suggest using American and European guidelines, which call for selective use of the DAT for the management of neonatal jaundice. Eliminating overuse will also result in considerable cost savings.
Introduction
The direct antiglobulin test (DAT), also known as the direct Coombs test, is a screening test used primarily to assess whether antibodies are attached to the patient’s red blood cells (RBCs), which can lead to destruction of the cell and subsequent immune hemolytic anemia.1 The predominant causes of positive DAT results in neonates are fetal-maternal ABO incompatibility, maternal alloimmunization and, less frequently, maternal autoimmune hemolytic anemia.2 Hemolytic disease of the newborn (HDN) arises when the mother is exposed to foreign antigens present on fetal RBCs. The mother’s immune system recognizes them as foreign antigens and starts producing immunoglobulin G (IgG) antibodies that are able to cross the placenta. Consequently, these antibodies can destroy and shorten the lifespan of fetal RBCs, resulting in clinical consequences.3 The clinical manifestations of hemolysis in newborns can range from mild anemia and hyperbilirubinemia to severe hemolysis and severe hyperbilirubinemia.4 Although neonatal jaundice is common and usually harmless, high levels of unconjugated bilirubin may place the infant at risk of developing a form of neurotoxicity known as kernicterus.4
For many years, blood typing and DAT testing of cord blood samples were considered standard procedures and performed in many hospitals for all infants. A positive DAT result has been considered a component of the diagnosis of HDN for many years.5 However, Levine and Meyer6 found that DAT was not diagnostic and did not predict the severity of hemolytic disease and was therefore unwarranted for routine screening. Madlon-Kay7 concluded that a selective approach limited to significantly jaundiced infants might be preferable in infants not discharged early. Dinesh8 reported that clinical jaundice, rather than a positive DAT result, alerted the physician to the possible need for phototherapy. Early onset and the rapid progression of bilirubinemia are the clearest indications of potential HDN and the need for phototherapy.5
Given the evidence in favor of a more selective approach to screening, our objective was to determine the need for DAT screening in full-term healthy newborns by correlating clinical signs and DAT results with the need for phototherapy. We also intended to describe the current practices at our institution with the goal of assessing whether changes should be instituted to reduce the costs of newborn screening. We determined the one-year incidence of DAT positivity and studied the relationships between risk factors and the need for phototherapy. We also evaluated the indications for starting phototherapy within the first 48 hours of life and prior to discharge.
Patients and Methods
This study was a retrospective cohort chart review of all newborns admitted to the nursery between January 1 and December 31, 2018, at King Fahad Hospital of the University, Al-Khobar, Saudi Arabia. The study was approved by the University Institutional Review Board (lRB) Committee (lRB UGS‐2019‐01‐349). Data were obtained for both the mothers and newborns from electronic medical records as well as blood bank records. The ABO/Rh status evaluation, DAT results and strength, and antibody identification were performed by the DiaMed gel testing method (Bio-Rad Laboratories, Cressier, Switzerland).
The data extracted for the mothers were age, parity, ABO group, and Rh status. The data collected for the newborns included gender, gestational age in weeks, birthweight in kilograms, ABO group, Rh status, and DAT results. The ABO/Rh type and DAT were determined from the cord blood for all babies and when a sample was clotted from the serum. Bilirubin levels were determined from the serum for all DAT-positive infants, or as per hospital protocol, which requires serum bilirubin to be assessed in infants of diabetic mothers and in infants small for gestational age, regardless of their clinical condition. In addition, the serum bilirubin level may have been assessed for clinical jaundice.
We compared the blood types of the mother with that of the neonate to determine ABO and RhD compatibility. In the newborns with a positive DAT result, we further determined the strength of DAT positivity. The strength of DAT positivity is graded on a scale from 0 to 4+ depending on the degree of agglutination, where 0 indicates no agglutination and 4+ indicates solid agglutination.
The bilirubin levels were determined from the serum in neonates at 3 hours of age if they were DAT positive, at 24 hours of age as per the hospital protocol for infants small for gestational age and infants of diabetic mothers, and at various ages as part of the evaluation for clinical jaundice. The neonates with clinical jaundice were included in analysis if the first bilirubin level was done at an age less than 48 hours and prior to discharge from the nursery. Additional bilirubin level assessments were performed as needed in follow-ups. We plotted bilirubin levels with neonatal age in hours. The need for phototherapy and the selection of the type (single phototherapy, double phototherapy, exchange transfusion) were decided after plotting the bilirubin levels according to an hour-specific bilirubin nomogram based on the National Institute for Health and Clinical Excellence (NICE) guidelines.9 The assessment of the need for phototherapy was limited to that subset of patients.
Statistical Analysis
Categorical variables are expressed as frequencies and percentages. Continuous variables are summarized as the mean (standard deviation) or median (interquartile range), as appropriate, depending on the normality of the data distribution. Cross tabulation and statistical significance of variables were assessed by independent t-test or chi-square test. A separate multivariate logistic regression with possible phototherapy requirement as the dependent variable was performed to explore which variables were associated with the need for phototherapy. A p value of <0.05 was considered to indicate statistical significance. The software package used in the multivariate analysis was jamovi, version 1.1.9.0 (retrieved from https://www.jamovi.org). The data were plotted with the R package ggplot2 3.2.1.
Results
Sixty-five neonates (65/1463, 4.4%) were DAT positive and 59 of those (90.8%) were born to mothers with blood group O. ABO incompatibility was more frequent in cases with a positive DAT result (P <0.001), but there was no difference in relation to Rh incompatibility (P=0.239). The serum bilirubin level was assessed in 251 neonates for the following reasons: 65 (25.9%) due to DAT positivity, 106 (42.2%) due to hospital protocol, and 80 (31.9%) due to clinical jaundice. The median (25th percentile, 75th percentile, range) maternal age of the 251 mothers was 32.0 (28.0, 36.0, 19–49) years. The mean parity was 3.0.
The bilirubin levels in neonates with clinical jaundice were more commonly obtained after 24 hours of age, which was likely related to the timing of discharge examination. The 24-hour bilirubin levels were higher in DAT-positive cases (P=0.06); however, peak bilirubin levels were not correlated with the DAT results (P=0.717). The median age for the first bilirubin level for neonates with DAT positive results was 3.5 hours, while neonates assessed due to hospital protocol and neonates with clinical jaundice were tested at a median of 24 and 36 hours, respectively. The 24-hour bilirubin level was measured in 170 patients for the following reasons: 61 (35.9%) neonates were DAT positive, 10 (5.9%) neonates had clinical jaundice, and 99 (58.2%) neonates were assessed per hospital protocol. There were 4 patients who were DAT positive without 24-hour serum bilirubin data, as the treating physician deemed it not necessary to obtain these data because the 3-hour serum bilirubin level was <59.85 µmol/L, and there were 9 patients in the hospital protocol group for whom testing was performed at variable times by request of the treating physician. The bilirubin levels in neonates with clinical jaundice were more commonly obtained after 24 hours of age, which was likely related to the timing of discharge examination.
Phototherapy was initiated in 36 (14.3%) of the 251 neonates in whom the need was assessed. The assessment was based on serum bilirubin levels and the hospital nomogram (based on the NICE guidelines) (Table 1). The most common indication for phototherapy was clinical jaundice in 22 neonates (61.1%), followed by DAT positivity in 12 (33.3%) and hospital protocol in 2 patients (5.6%) (P <0.01 by chi-square overall comparison). There was no difference in gender, gestational age, or birthweight between the groups (Table 1). There was also no difference in ABO/Rh incompatibility between the groups (Table 2). The need for phototherapy was similar in the DAT-positive cases and DAT-negative cases (P=0.271), with a sensitivity of 33.3% (95% CI 19.1–51.0) and positive predictive value of 18.5% (95% CI 10.3–30.4) for predicting phototherapy need. Phototherapy requirement did not differ in relation to the strength of DAT positivity (P=0.333) (Table 3). The lack of statistical significance emphasizes that DAT should not guide clinicians in their evaluation for the need of obtaining bilirubin levels to evaluate the need of phototherapy.
 |
Table 1 Demographics of the Patients Assessed for the Need for Phototherapy (n=251) |
 |
Table 2 Maternal and Neonatal ABO Blood Groups of the Patients Assessed for the Need for Phototherapy (n=251) |
 |
Table 3 The DAT Results and Bilirubin Levels in Patients Assessed for Phototherapy (n=251) |
The 24-hour and first serum bilirubin levels were significantly higher in infants who were deemed to require phototherapy (Table 3) (P <0.001 for both comparisons). There were only two babies in which serum bilirubin was assessed for hospital protocol reasons and required phototherapy, indicating the possibility that the bilirubin level is assessed excessively per our hospital protocols.
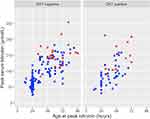
The type of phototherapy was single in most cases (91.7%, n=33), and none required exchange transfusion. In the comparisons of the peak bilirubin level by age at sampling, the serum bilirubin values for neonates who underwent phototherapy clearly clustered among the neonates with higher peak bilirubin levels, regardless of the DAT results (Figure 1). Figure 1 reflects the difference in bilirubin levels by phototherapy requirement in Table 3. When neonates with a gestational age less than 38 weeks were compared with the others, the peak bilirubin levels for the neonates who underwent phototherapy were generally higher than in those who did not undergo phototherapy (Figure 2) (P=0.947).
Several factors were assessed to explore relationships with the need for phototherapy. In the univariate analyses, the serum bilirubin values were the only statistically significant variables. Other variables, such as ABO compatibility, gestational age, birthweight, and DAT results, were included in the multivariate analysis for clinical reasons or because of known or suspected associations with the need for phototherapy. However, only the peak bilirubin and 24-hour bilirubin values were statistically significant.
A total of 64 eluates were detected in the DAT-positive neonates. The most commonly detected antibodies were anti-B (45.3%) followed by anti-A (32.8%). There were 13 DAT-positive neonates with a positive maternal antibody screen. The most common maternal antibody detected was anti-D in 5 mothers (38.5%). The remaining antibodies detected included anti-E (n=3), anti-M (n=1), and anti-c (n=1) antibodies. There was no antibody titer reported for the mothers or newborns. Eleven (84.6%) of the neonatal eluates had antibodies that were the same as in the mothers. The two newborns that had different eluates than the mothers were a nonspecific antibody in a neonate born to a mother with anti-D antibody, and anti-B antibody detected in a mother with anti-M.
Discussion
Our results indicate that factors other than a positive DAT are important in assessing the need for phototherapy in Saudi newborns potentially at risk for HDN. As expected, clinical signs of jaundice were found to be an indicator of high serum bilirubin levels. The neonates with positive DAT results did not have higher peak bilirubin levels or any other indication for phototherapy requirement compared to those with a negative DAT.
Our results are consistent with other reports in the literature. As noted by Keir et al1, hyperbilirubinemia alone does not indicate a need for the DAT in the absence of anemia, reticulocytosis, or other signs of hemolysis. The positive predictive value of the test for significant hyperbilirubinemia was poor, ranging from 12 to 53%, as shown in our results.8,10,11 A third of neonates of ABO incompatible mothers may have a positive DAT result, but few develop HDN.12
Studies have shown that unselective DAT testing for all infants is not cost-effective.12,13 The authors of these studies concluded that selective newborn cord testing of neonates born to mothers with blood group O is feasible and can decrease hospital costs without increasing the risk of HDN. Resources and costs, as a result, would be saved without increasing the risk of clinically significant hyperbilirubinemia.12 Such selective testing in fact has been implemented in many institutions, and many recommendations advocate for testing according to the clinical evaluations of newborns.14,15 In Saudi Arabia, there is no unified approach in screening for HDN. While some centers are performing routine DAT testing for all neonates, others perform only selective testing for blood group O or testing of symptomatic neonates only.
In our study, we examined the issue in terms of the need for phototherapy and found that the decision to use phototherapy in neonates did not differ between DAT-positive and DAT-negative infants. As expected, serum bilirubin levels, regardless of the age of testing, were significantly higher in neonates who required phototherapy and unrelated to DAT results. In the plot of the peak serum bilirubin levels as a function of the DAT results, the bilirubin levels are similar in the infants who did and did not undergo phototherapy. In the DAT-negative neonates, clinical signs of jaundice were indicators of high serum bilirubin levels, further indicating that the DAT test is not of value in predicting which infants might be in need of phototherapy. The neonates requiring phototherapy were more commonly identified by clinical evaluations, emphasizing the importance of clinical assessments and the likelihood that serum bilirubin assessments and the DAT are being overused in our institution.
Studies that evaluated the effectiveness of the DAT in predicting hyperbilirubinemia demonstrated sensitivity values ranging from 15% to 64%, which is consistent with our results.8,10,11 Maisels and Watchko16 suggested in 2013 that routine testing for blood type and the DAT in infants of blood group O mothers “can safely be abandoned”. The recommendations of the American Academy of Pediatrics (AAP) published in 2004 considered the tests optionally provided optimal follow-up.14 In multivariable analyses,17,18 bilirubin levels were the one factor most predictive of the need for phototherapy and future development of hyperbilirubinemia. Our multiple logistic regression results were consistent with these findings.
There are some limitations in our studies that warrant future follow-up investigations. Although we included all maternal-neonate pairs over one year, the size of the sample was relatively small, being from one institution. However, we had sufficient data to evaluate the important variables in univariate analyses, namely, the serum bilirubin levels in the early ages of life, and associate those data with the need for phototherapy to prevent potential severe hyperbilirubinemia. We were not able to evaluate other factors that may cause an increased risk of HDN, such as hemoglobin H disease or glucose-6-dehydrogenase deficiency, as they are not assessed as part of neonatal screening and not routinely evaluated in neonates started on phototherapy. In addition, one aspect we were unable to evaluate was the strength of DAT positivity in relation to the need for phototherapy. Strength was measured in only 58 patients (89.2% of DAT-positive neonates), and of those patients, high values for strength were observed in only two patients who had DAT strength values of 3+, and neither required phototherapy. We did not observe any patients with DAT values of 4+, which has been reported to be strongly associated with the need for a prolonged duration of phototherapy.8,19 The NICE guidelines recommend that when the DAT is performed in infants who undergo a formal assessment for significant hyperbilirubinemia, the strength of the reaction is considered.9 The results should be interpreted with consideration of whether the mother has received anti-D prophylaxis during pregnancy, as maternal anti-D is associated with positive DAT in neonates.20 Furthermore, there may have been selection bias regarding the infants from whom a serum bilirubin sample was taken after clinical evaluation, since the practice was to assess the bilirubin level in all DAT-positive infants. As the results show, clinical jaundice rather than DAT positivity was indicative of the need for phototherapy. We also do not have the complete records of the post discharge follow-ups of babies who may have later required phototherapy since some neonates may have gone to other hospitals. Of the 27 babies that presented to our emergency department for the assessment of clinical jaundice, all of them were DAT negative, and five (18.5%) required phototherapy.
Despite these shortcomings, our study supports the notion that unselective DAT testing in newborns should not be the standard care for HDN prevention and management. In this regard, the NICE guidelines also recommend against the use of DAT and provide a set of nomograms and guidance for initiating phototherapy based solely on the serum bilirubin level.9 For neonates of gestational age 38 weeks or more, they recommend that phototherapy be considered when bilirubin levels are higher than 250 µmol/L at 24 hours of age. In many cases, this recommendation is followed but is not universally applied in our institution. All newborns in our study underwent direct antiglobulin testing. We recommend a change from this unselective use of the DAT to a policy that follows the American and European guidelines for managing neonatal jaundice to avoid the costs of routine DAT testing for all full-term healthy newborns. A prospective study evaluating selective DAT and bilirubin testing in cases of clinical jaundice in our center is warranted, and follow-ups post discharge are necessary to study the risk factors that may indicate an increased risk of readmission for neonatal jaundice.
Conclusions
Our paper confirmed that the DAT is not useful alone for screening for HDN, and there are other factors important in assessing the need for phototherapy. The test is overused in our center due to unselective testing. The most useful indicator for the need for phototherapy is clinical jaundice. A clinical evaluation of neonates is essential and will likely provide the first indication for the need for phototherapy.
Abbreviations
DAT, direct antiglobulin test; NICE, National Institute for Health and Clinical Excellence; HDN, hemolytic disease of the newborn; RBC, red blood cells; NICU, neonatal intensive care.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the University Institutional Review Board (lRB) and Ethical Committee (lRB UGS‐2019‐01‐349). This is a retrospective study conducted on electronic records of patients with no patient identity being disclosed. Therefore, informed consent was not applicable. This study was conducted in accordance with the Declaration of Helsinki.
Funding
No funding sources.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Keir A, Agpalo M, Lieberman L, Callum J. How to use: the direct antiglobulin test in newborns. Arch Dis Child Educ Pract Ed. 2015;100(4):198–203. doi:10.1136/archdischild-2013-305553
2. Valsami S, Politou M, Boutsikou Τ, Briana D, Papatesta M, Malamitsi-Puchner A. Importance of Direct Antiglobulin Test (DAT) in cord blood: causes of DAT (+) in a cohort study. Pediatr Neonatol. 2015;56(4):256–260. doi:10.1016/j.pedneo.2014.11.005
3. Klein HG, Anstee DJ. Mollison’s Blood Transfusion in Clinical Medicine. Oxford: Wiley-Blackwell; 2014.
4. Hendrickson JE, Delaney M. Hemolytic disease of the fetus and newborn: modern practice and future investigations. Transfus Med Rev. 2016;30(4):159–164. doi:10.1016/j.tmrv.2016.05.008
5. Murray NA, Roberts IA. Haemolytic disease of the newborn. Arch Dis Child Fetal Neonatal Ed. 2007;92(2):F83–F88. doi:10.1136/adc.2005.076794
6. Levine DH, Meyer HB. Newborn screening for ABO hemolytic disease. Clin Pediatr. 1985;24(7):391–394. doi:10.1177/000992288502400707
7. Madlon-Kay DJ. Identifying ABO incompatibility in newborns: selective vs automatic testing. J Fam Pract. 1992;35(3):278–280.
8. Dinesh D. Review of positive direct antiglobulin tests found on cord blood sampling. J Paediatr Child Health. 2005;41(9–10):504–507. doi:10.1111/j.1440-1754.2005.00692.x
9. National Institute for Health and Care Excellence (NICE). Jaundice in newborn babies under 28 days; 2020. Available from: https://www.nice.org.uk/guidance/cg98/evidence.
10. Herschel M, Karrison T, Wen M, Caldarelli L, Baron B. Evaluation of the direct antiglobulin (Coombs’) test for identifying newborns at risk for hemolysis as determined by end-tidal carbon monoxide concentration (ETCOc); and comparison of the Coombs’ test with ETCOc for detecting significant jaundice. J Perinatol. 2002;22(5):341–347. doi:10.1038/sj.jp.7210702
11. Meberg A, Johansen KB. Screening for neonatal hyperbilirubinaemia and ABO alloimmunization at the time of testing for phenylketonuria and congenital hypothyreosis. Acta Paediatr. 1998;87(12):1269–1274. doi:10.1111/j.1651-2227.1998.tb00950.x
12. Shahid R, Graba S. Outcome and cost analysis of implementing selective Coombs testing in the newborn nursery. J Perinatol. 2012;32(12):966–969. doi:10.1038/jp.2012.26
13. Leistikow EA, Collin MF, Savastano GD, de Sierra TM, Leistikow BN. Wasted health care dollars. Routine cord blood type and Coombs’ testing. Arch Pediatr Adolesc Med. 1995;149(10):1147–1151. doi:10.1001/archpedi.1995.02170230101015
14. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114(1):297–316. doi:10.1542/peds.114.1.297
15. Newman J. Guidelines for detection, management and prevention of hyperbilirubinemia in term and late preterm newborn infants (35 or more weeks’ gestation) - Summary. Paediatr Child Health. 2007;12(5):401–418. doi:10.1093/pch/12.5.401
16. Maisels MJ, Watchko JF. Routine blood typing and DAT in infants of group O mothers. J Perinatol. 2013;33(7):579. doi:10.1038/jp.2013.6
17. Bhutani VK, Stark AR, Lazzeroni LC, et al. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J Pediatr. 2013;162(3):477–482.e1. doi:10.1016/j.jpeds.2012.08.022
18. Maisels MJ, Deridder JM, Kring EA, Balasubramaniam M. Routine transcutaneous bilirubin measurements combined with clinical risk factors improve the prediction of subsequent hyperbilirubinemia. J Perinatol. 2009;29(9):612–617. doi:10.1038/jp.2009.43
19. Oztekin O, Kalay S, Tezel G, et al. Is the strength of direct antiglobulin test important for the duration of phototherapy? J Matern Fetal Neonatal Med. 2014;27(5):534–536. doi:10.3109/14767058.2013.819335
20. Dillon A, Chaudhari T, Crispin P, Shadbolt B, Kent A. Has anti-D prophylaxis increased the rate of positive direct antiglobulin test results and can the direct antiglobulin test predict need for phototherapy in Rh/ABO incompatibility? J Paediatr Child Health. 2011;47(1–2):40–43. doi:10.1111/j.1440-1754.2010.01888.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.