Back to Journals » Patient Preference and Adherence » Volume 11
Validation of the VERITAS-Pro treatment adherence scale in a Spanish sample population with hemophilia
Authors Cuesta-Barriuso R , Torres-Ortuño A , Galindo-Piñana P, Nieto-Munuera J, Duncan N, López-Pina JA
Received 6 November 2016
Accepted for publication 1 February 2017
Published 27 March 2017 Volume 2017:11 Pages 653—660
DOI https://doi.org/10.2147/PPA.S126828
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Rubén Cuesta-Barriuso,1–3 Ana Torres-Ortuño,4 Pilar Galindo-Piñana,4 Joaquín Nieto-Munuera,4 Natalie Duncan,5 José Antonio López-Pina6
1Department of Physiotherapy, School of Biomedical and Health Sciences, European University of Madrid, 2Fishemo, Centro Especial de Empleo, Spanish Federation of Hemophilia, 3Royal Foundation Victoria Eugenia, Madrid, 4Department of Psychiatry and Social Psychology, Faculty of Medicine, University of Murcia, Murcia, Spain; 5Indiana Hemophilia & Thrombosis Center, Indianapolis, IN, USA; 6Department of Basic Psychology and Methodology, Faculty of Psychology, University of Murcia, Murcia, Spain
Purpose: We aimed to conduct a validation in Spanish of the Validated Hemophilia Regimen Treatment Adherence Scale – Prophylaxis (VERITAS-Pro) questionnaire for use in patients with hemophilia under prophylactic treatment.
Patients and methods: The VERITAS-Pro scale was adapted through a process of back translation from English to Spanish. A bilingual native Spanish translator translated the scale from English to Spanish. Subsequently, a bilingual native English translator translated the scale from Spanish to English. The disagreements were resolved by agreement between the research team and translators. Seventy-three patients with hemophilia, aged 13–62 years, were enrolled in the study. The scale was applied twice (2 months apart) to evaluate the test–retest reliability.
Results: Internal consistency reliability was lower on the Spanish VERITAS-Pro than on the English version. Test–retest reliability was high, ranging from 0.83 to 0.92. No significant differences (P>0.05) were found between test and retest scores in subscales of VERITAS-Pro. In general, Spanish patients showed higher rates of nonadherence than American patients in all subscales.
Conclusion: The Spanish version of the VERITAS-Pro has high levels of consistency and empirical validity. This scale can be administered to assess the degree of adherence of prophylactic treatment in patients with hemophilia.
Keywords: hemophilia, adherence treatment, validity, reliability
Introduction
Hemophilia is a congenital coagulopathy characterized by muscle and joint bleeding. Repeated joint bleeds eventually result in hemophilic arthropathy. The development of degenerative joint lesions (hemophilic arthropathy) has been observed as a result of insufficient or nonexistent treatment.1
The introduction of clotting factor replacement therapy offers patients with hemophilia an effective treatment for the control of bleeding processes. It can be administered in prophylaxis regimens or on-demand regimens. The development and generalization of prophylactic treatments2 has helped to prevent the development of hemophilic arthropathy. Prophylactic treatment is based on the regular administration of factor concentrates in order to prevent the occurrence of bleeding episodes.3
Higher efficacy of prophylactic treatment relative to on-demand treatment has been demonstrated in the prevention of both bleeding episodes and hemophilic arthropathy.4,5 It has been proven to be effective in decreasing both the number of visits to emergency services and hospitalizations, increasing physical activity as well as improving absenteeism and school performance.6 Furthermore, there has been an improvement in patients’ quality of life, enabling them to lead a relatively normal life.7,8 Therefore, prophylactic therapy is the gold standard in the treatment of severe hemophilia A or B, according to institutions such as the Scientific Commission of the Royal Foundation Victoria Eugenia (Spain), the Medical and Scientific Advisory Council (MASAC),3 the World Health Organization (WHO)9 or the World Federation of Hemophilia.10 However, it is still common to diagnose hemarthrosis in patients with hemophilia.
Venous access, factor preparation time and long-term dependence on prophylaxis are some barriers that contribute to poor adherence with medical treatment.11–15 These factors can be influenced by the patient’s attitude to the clinical evolution process and the doctor–patient relationship.16,17
In 2010, Duncan et al18 developed and validated the first specific adherence questionnaire for patients with hemophilia receiving prophylactic treatment. The Validated Hemophilia Regimen Treatment Adherence Scale – Prophylaxis (VERITAS-Pro) questionnaire was developed in the USA and has also been validated in Dutch.19 Until then, the measures to assess adherence included frequency of joint bleeds, joint examination, hand-written logs and pharmacy records.
In a recent study, Krishnan et al20 observed how low adherence to treatment in hemophilia (as measured with VERITAS-Pro) is associated with an increased number of bleeding episodes, especially in adults. These results provided evidence of the usefulness of the VERITAS-Pro questionnaire to assess adherence to treatment and the clinical symptoms of patients with hemophilia. By contrast, adherence to prophylactic treatment is higher in pediatric patients, falling drastically when reaching adolescence.21
The aim of this study was to conduct a validation in Spanish of the VERITAS-Pro questionnaire, for use in patients with hemophilia under prophylactic treatment.
Patients and methods
Study design
This study was proposed as a correlational study of patients with hemophilia aged 13–62 years.
Patients
Seventy-three individuals were recruited to be administered the Spanish version of the VERITAS-Pro scale. The questionnaire was sent to patients for completion, along with a cover letter and the clinical record (including clinical and sociodemographic data).
Ethics and consent to participate
The study was approved by the Ethics Committee of the Universidad Católica San Antonio of Murcia and the Spanish Agency for Medicines and Health Products (Agencia Española de Medicamentos y Productos Sanitarios). The participants also consented to participating in the study by signing an informed consent document.
Measuring instrument
The VERITAS-Pro scale consists of 24 Likert-type items ranging from 1 to 5 (never or 0% of the time, rarely or 25% of the time, sometimes or at least 50% of the time, often or at least 75% of the time, and always or 100% of the time) grouped into 6 dimensions: Time, Dose, Plan, Remember, Skip and Communicate. The minimum adherence score was 24 and the maximum adherence score was 120 in the Spanish version; in each subscale, the score ranged from 4 to 20 points. Importantly, lower scores indicate better adherence and higher scores indicate poorer adherence.
Procedure
The VERITAS-Pro scale was adapted through a process of back translation from English to Spanish.22 A bilingual native Spanish translator translated the scale from English into Spanish; then a bilingual native English translator translated the scale from Spanish into English. The translators did not know each other and had no contact with the research team.
In 19 of the items, the consistency between the 2 translations was 100%; in the remaining 5 items, the inconsistencies were resolved by agreement between the research team and translators. The scale was applied twice (2 months) to evaluate the test–retest reliability.
Psychometric and statistical analysis
Evaluation of item quality was performed using the rule whereby the item–test correlations should be within the interval (0.30–0.70). The internal consistency analysis was performed using Cronbach’s alpha coefficient and score stability using the Pearson correlation coefficient.
The empirical validity was tested with Student’s t-tests or analyses of variance (ANOVAs) based on the clinical and sociodemographic characteristics presented in Table 1. The effect size (ES) was evaluated with ω2 (ES small: 0.01; ES medium: 0.06; ES large: 0.14) and Cohen’s d standardized mean difference (ES small: 0.20–0.30; medium ES: 0.50; ES large: 0.80). For all analyses, SPSS v19.0 was used.
Results
Participants
The age of patients ranged from 13 to 62 years (mean [M] =30.15 years, standard deviation [SD] =10.11). Thirty-one (42.5%) were university graduates, 28 (38.4%) had high school studies and 14 (19.2%) primary studies. Twenty (27.4%) were employers, 32 (43.8%) were employees, 18 (24.7%) were unemployed and 3 (4.1%) were students. Twenty-three (31.5%) were married and 50 (68.5%) were single (Table 1).
Sixty-one (83.6%) had type A hemophilia and 12 (16.4%) had type B hemophilia, with it being moderate in 3 cases (4.1%) and severe in the remaining 70 (95.9%). All patients (100%) followed self-treatment. Six (8.2%) had inhibitors. Forty-three (58.9%) had suffered hemarthrosis in the previous month, and 69 (94.5%) had been diagnosed with hemophilic arthropathy in at least 1 joint. Thirty-three (45.2%) had no coinfections, 19 (26%) had hepatitis C virus (HCV), 4 (5.5%) had human immunodeficiency virus (HIV) infection and 17 had both HCV and HIV. Forty (54.8%) patients had a family history of hemophilia (Table 1).
VERITAS-Pro scores
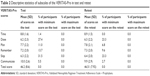
Table 2 presents the means and SDs of the items on the full scale and each of the subscales. There were no missing data, and the percentage of cases with minimum (24) or maximum (120) score in the full scale was 0%, although the floor effect was obtained (>15%) in Dose (27.4%) and Skip (31.5%) in the test and the retest (Dose: 23.3%; Skip: 23.3%). No significant differences in scores were found in the subscales of VERITAS-Pro (P>0.05).
The means of the subscales of the Spanish validation sample were compared against the means of the application validated in the USA by Duncan et al.18 No significant differences in scores were found for each subscale.
All correlations between the VERITAS-Pro subscales were significant (P<0.05), except between Skip and Communicate (P>0.05), both for the test and the retest. In the test, the highest correlations were obtained between Skip and Dose (r=0.63, P<0.001) and Skip and Remember (r=0.54, P<0.001) and the lowest was between Skip and Communicate (r=0.15, P>0.05). In the retest, the highest correlation was obtained between Skip and Dose (r=0.56, P<0.001) and the lowest between Skip and Time (r=0.13, P>0.05).
Item analysis
An analysis of means and SDs of the total score based on the categories is shown in Table 3. If the average of the total score increases in accordance with the item category, this is an indicator of the proper functioning of the item to assess adherence to treatment. Item analysis (Table 3) revealed that all item–test correlations were within the specified range, except for Items 3 (I do prophylaxis infusions in the morning as recommended), 10 (I keep close track of how much factor and how many supplies I have), 11 (I run out of factor and supplies before I order more) and 14 (Remembering to do prophylaxis is difficult). Close examination of Table 3 shows that the average of the total scores for Category 2 of Item 3 was higher than that for all other categories and the assumption that the average scores increased with the increase of the selected category was not fulfilled. The same happened for Item 14 in Category 3.
No significant differences (P>0.05) were found between the test and retest scores in the subscales of VERITAS-Pro.
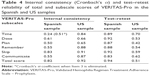
Reliability analysis
Internal consistency of the subscales and the total score were lower in the Spanish sample than in the US sample (Table 4), with special reference to the Time subscale (α=0.24), which improved substantially (α=0.51) with the elimination of Item 3. The subscale that had greatest internal consistency was Skip (α=0.83).
Overall, the test–retest reliability of the Spanish sample was high, ranging from 0.83 (Communicate) to 0.92 (Skip), while the test–retest reliability of the total scores was 0.94 (Table 4). The test–retest reliability was higher in the Spanish sample than in the US sample, which showed a lower stability between the test and retest scores in all subscales and in the total score.
Empirical validity
No significant differences were obtained in the patient sample based on the type of hemophilia suffered, the severity of hemophilia, coinfections with HCV and/or HIV, and marital status.
Patients who had inhibitors showed greater adherence to the Skip subscale (ie, less likely to skip infusions) than those without (t[13.18] =5.17, P<0.001; d=0.58) (Table 5). Hemarthrosis patients showed a greater control of the Dose (t[70.63] =3.32, P=0.001; d=0.73), Plan (t[71] =2.739, P=0.006; d=0.67) and Skip (t[70.72] =2.725, P=0.008; d=0.61) subscales. Patients with arthropathy better controlled the Time of treatment (t[71] =2.423, P=0.018; d=0.58), whereas patients with a history of hemophilia were significantly better at controlling the Dose (t[66.94] =2.35, P=0.022; d=0.54).
Depending on the type of academic studies, patients in primary studies showed the highest trend to Plan treatment (F[2,73] =4.31, P=0.017, ω2=0.08) being less likely to Skip treatment (F[2,73] =6.82, P=0.002, ω2=0.14), depending on the type of employment, the unemployed had better memory for performing prophylaxis (F[3,73] =6.48, P=0.001, ω2=0.18), while employees best communicated with the treatment center (F[3,73] =5.24, P=0.003, ω2=0.15).
Adherence rate
In general, Spanish patients showed higher rates of nonadherence than USA patients in all subscales and in the total score, except in the Communicate subscale (Table 6).
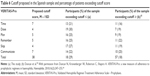  | Table 6 Cutoff proposed in the Spanish sample and percentage of patients exceeding cutoff score |
Discussion
Psychometric properties and scores
The VERITAS-Pro is a valid and reliable instrument to measure adherence to treatment among the Spanish population. However, the internal consistency of the subscales and total score were lower in the Spanish sample than in the US sample, especially in the subscale Time (α=0.24), which improved when Item 3 (α=0.51) was removed. This may be due to the inconsistency of Items 3 and 14, which do not work properly among the Spanish population. These items may not be measuring the same phenomenon, and their modification could improve the quality of the scale.
The floor effect found in the subscales Dose and Skip both in the test and the retest reveals that 27% of patients never comply with professional indications for treatment; the reasons why this happens should be addressed to improve prognosis in adherence.
With regard to the test–retest reliability in the Spanish sample (0.94), it was higher than that in the US sample (0.51), which could be due to the fact that for the latter, the questionnaires were sent after 2 weeks, and replies were voluntary. However, in this study, it was administered after 2 months, and all patients completed them again in the clinic, perhaps resulting in a greater stability of scores.
Empirical validity
Upon analysis of the empirical validity in terms of the independent variables, we find that the development of hemarthrosis in the previous month is the only variable with significant clinical results. This could be due to the importance given by the patient to prophylactic treatment in the prevention of bleeding episodes and the symptoms (pain, swelling, functional disability and muscle atrophy) with respect to the variables dosing, infusion planning, omission of infusions and full adherence to treatment.
Moreover, the educational level is associated with remembrance of the prophylactic regimen and the employment status with the omission of infusions and communication. In a significant but less noticeable manner, it is noted that the diagnosis of hemophilic arthropathy in at least 1 joint and a family history of hemophilia are related to the temporal control and dosing of the factor, respectively. It may be due to the prior knowledge of hemorrhagic symptoms and the consequences, as well as the perception of the consequences of hemophilia, in these patients.
Sample adherence to treatment
The results of this study show that patients in the Spanish sample had lower adherence to treatment than those enrolled in the study conducted by Duncan et al.18 In our opinion, there are several reasons. First, the Spanish and American health models are totally different, the Spanish system favoring a universal free access to medical treatments, which may weaken the patient’s obligation to comply with the prescription. Moreover, the fear of treatment in many adult patients, as a result of HIV and HCV infections, makes adherence lower in this group of patients. Finally, it must be noted that although in children with severe hemophilia, prophylaxis is generalized, this is not the case in adults, for which the percentage of patients receiving prophylactic treatment is much lower.
Strengths and limitations
The main strength of the study lies in the methodology used to perform the process of back translation, as well as the evaluation and analysis of the VERITAS-Pro questionnaire, which was administered twice to the same patients. This methodology promotes a comprehensive psychometric analysis of the validation.
However, this work presents some limitations. A main drawback is that it is impossible to compare the results of the VERITAS-Pro questionnaire to those obtained with the application of another level of adherence to treatment in patients with hemophilia, because there is no measuring instrument to evaluate this variable in this group of patients. Although no significant differences were obtained between patients’ replies depending on the type and severity of hemophilia, this detail must be taken into account.
Conclusion
The Spanish version of the VERITAS-Pro has high levels of consistency and empirical validity. This measuring instrument can be administered as a useful tool for assessing the degree of adherence with medical treatment by adult patients with hemophilia receiving prophylaxis. It is necessary to confirm the validity of the VERITAS-Pro questionnaire with other scales assessing adherence to treatment in this group of patients.
Acknowledgments
The authors are especially grateful to Murcia Regional Hemophilia Association, Association of Hemophilia of Burgos, Association of Hemophilia of Santa Cruz de Tenerife, Gallega Association of Hemophilia and Spanish Federation of Hemophilia for their help in recruitment of the sample. The authors wish to thank Medtep Inc., promoter of the study u-patient. Grifols Inc provided funding for this study in accordance with international guidelines on good publication practices.
Author contributions
Rubén Cuesta-Barriuso, Ana Torres-Ortuño and José Antonio López-Pina have made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; Pilar Galindo-Piñana and Joaquín Nieto-Munuera have been involved in drafting the manuscript or revising it critically for important intellectual content; and Rubén Cuesta-Barriuso, Ana Torres-Ortuño, Pilar Galindo-Piñana, Joaquín Nieto-Munuera, Natalie Duncan and José Antonio López-Pina have given final approval of the version to be published. All authors contributed toward data analysis, drafting and critically revising the paper and agreeing to be accountable for all aspects of the work.
Disclosure
The authors report no other conflicts of interest in this work.
References
Van den Berg HM, Dunn A, Fischer K, Blanchette VS. Prevention and treatment of musculoskeletal disease in the haemophilia population: role of prophylaxis and synovectomy. Haemophilia. 2006;12(suppl 3):159–168. | ||
Liesner RJ, Khair K, Hann IM. The impact of prophylactic treatment on children with severe haemophilia. Br J Haematol. 1996;92:973–978. | ||
National Hemophilia Foundation. Medical and Scientific Advisory Council (MASAC) Recommendations Concerning Prophylaxis. MASAC Document 179. New York, NY: National Hemophilia Foundation; 2007:10001. | ||
Manco-Johnson M, Abshire T, Shapiro A, et al. Prophylaxis versus episodic treatment to prevent joint disease in boys with severe hemophilia. N Engl J Med. 2007;357(6):535–544. | ||
Gringeri A, Lundin B, von Mackensen S, Mantovani L, Mannucci PM; ESPRIT Study Group. A randomized clinical trial of prophylaxis in children with haemophilia A (the ESPRIT study). J Thromb Haemost. 2011;9:700–710. | ||
Shapiro A, Donfield S, Lynn H, et al; Academic Achievement in Children with Hemophilia Study Group. Defining the impact of hemophilia: the academic achievement in children with hemophilia study. Pediatrics. 2001;108(6):e105. | ||
Thornburg C, Pipe S. Adherence to prophylactic infusions of factor VIII or factor IX for haemophilia. Haemophilia. 2006;12:198–199. | ||
Coppola A, Franchini M, Tagliaferri A. Prophylaxis in people with haemophilia. J Thromb Haemost. 2009;101:674–681. | ||
World Health Organization. Delivery of Treatment for Haemophilia: Report of a Joint WHO/WFH/ISTH Meeting London, UK; February 11–13, 2002. London, UK: WHO, 2002. | ||
WFH [webpage on the Internet]. WFH Guidelines for the Management of Hemophilia; 2015. Available from: http://www.wfh.org/en/resources/wfh-treatment-guidelines. Accessed February 3, 2017. | ||
Hacker MR, Geraghty S, Manco-Johnson M. Barriers to compliance with prophylaxis therapy in haemophilia. Haemophilia. 2001;7(4):392–396. | ||
Khair K. Minimizing joint damage: the role of nurses in promoting adherence to hemophilia treatment. Orthop Nurs. 2010;29(3):193–200. | ||
Kyngas HA, Kroll T, Duffy ME. Compliance in adolescents with chronic diseases: a review. J Adolesc Health. 2000;26:379–388. | ||
Petrini P. Identifying and overcoming barriers to prophylaxis in the management of haemophilia. Haemophilia. 2007;13(suppl 2):16–22. | ||
Thornburg CD. Physicians’ perceptions of adherence to prophylactic clotting factor infusions. Haemophilia. 2008;14:25–29. | ||
Schrijvers LH, Uitslager N, Schuurmans MJ, Fischer K. Barriers and motivators of adherence to prophylactic treatment in haemophilia: a systematic review. Haemophilia. 2013;19(3):355–361. | ||
Llewellyn C, Miners A, Lee C, Harrington C, Weinman J. The illness perceptions and treatment beliefs of individuals with severe haemophilia and their role in adherence to home treatment. Psychol Health. 2003;18:185–200. | ||
Duncan N, Kronenberger W, Roberson C, Shapiro A. VERITAS-Pro: a new measure of adherence to prophylactic regimens in haemophilia. Haemophilia. 2010;16(2):247–255. | ||
Lock J, Raat H, Duncan N, et al. Adherence to treatment in a Western European paediatric population with haemophilia: reliability and validity of the VERITAS-Pro scale. Haemophilia. 2014;20(5):616–623. | ||
Krishnan S, Vietri J, Furlan R, Duncan N. Adherence to prophylaxis is associated with better outcomes in moderate and severe haemophilia: results of a patient survey. Haemophilia. 2015;21(1):64–70. | ||
Miesbach W, Kalnins W. Adherence to prophylaxis treatment in patients with haemophilia in Germany. Haemophilia. 2016;22(5):e367–e374. | ||
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–3191. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.