Back to Journals » Open Access Emergency Medicine » Volume 15
Upper Extremity Musculoskeletal Injuries Presenting to an Emergency Department Before and During the Initial COVID-19 Pandemic Surge
Authors Prokopakis KE, Bolotin T, Donley C, Lomasney M, Harter J, Graham J , Chopra Q, Olsen S, Noga J, Gatchel M, Paull B, Greyslak V, Bradford B, Plummer A, Powell C
Received 4 July 2022
Accepted for publication 27 January 2023
Published 7 March 2023 Volume 2023:15 Pages 63—68
DOI https://doi.org/10.2147/OAEM.S379059
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Hans-Christoph Pape
Kayla E Prokopakis,1 Todd Bolotin,1,2 Chad Donley,1,2 Mark Lomasney,1 Jason Harter,1 Jack Graham,1 Quincy Chopra,1 Steven Olsen,1,2 Joseph Noga,1,2 Matthew Gatchel,2 Brendan Paull,1 Victoria Greyslak,1 Bret Bradford,1 Anna Plummer,1 Carrie Powell3
1Department of Emergency Medicine, Mercy Health St. Elizabeth Boardman Hospital, Boardman, OH, USA; 2Department of Emergency Medicine, Mercy Health St. Elizabeth Youngstown Hospital, Youngstown, OH, USA; 3Lake Erie College of Osteopathic Medicine, Erie, PA, USA
Correspondence: Kayla E Prokopakis, Department of Emergency Medicine, Mercy Health St. Elizabeth Boardman Hospital, Boardman, OH, USA, Email [email protected]
Study Objective: The SARS-CoV-2 (COVID-19) pandemic significantly impacted emergency department volume and acuity. The Delta and Omicron variants contributed to additional surges. We describe the impact that the initial pandemic phase had on frequency and severity of typically non-life-threatening emergencies using upper extremity injuries as a model for other potentially emergent presentation as compared to pre-pandemic times. We do this using the epidemiology of pre-defined significant upper extremity injuries at our facility as a specific example of what occurred at an urban trauma center.
Methods: We conducted a comparison of two 6-month periods: between March 2019 and August 2019 (prior to COVID-19) and between March 2020 and August 2020 after the onset of the initial COVID-19 wave. We performed a retrospective chart review of patients who presented with upper extremity injury chief complaints using analysis of the electronic medical record at a single urban tertiary care trauma center in the Midwestern United States. We investigated examination findings, imaging, frequency of surgical procedures and final diagnosis.
Results: In the 2019 study period, there were 31,157 ED patients, including 429 with upper extremity injuries, of which 108 patients had significant injuries. In the 2020 study period, there were 24,295 patient presentations, of which 118 of 296 upper extremity presentations were significant. We a priori defined significant injury as follows: fractures, dislocations, neurovascular injuries, or need for operative intervention within 24 hours of ED presentation. Specifically, 25.2% of injuries were significant pre-COVID-19 and 39.9% (p < 0.001) during the initial COVID-19 surge. The absolute number and percentage of significant injuries increased from pre-COVID-19 compared to the initial COVID-19 surge despite an overall 22% decrease in total patient volume.
Conclusion: The incidence of significant upper extremity musculoskeletal injuries increased during the pandemic even though the overall number of ED presentations for upper extremity musculoskeletal injuries decreased.
Keywords: COVID-19, musculoskeletal complaints, emergency department presentation, upper extremity
Introduction
The COVID-19 pandemic has led to challenges and changes throughout the health-care field.1–4 In emergency departments worldwide, there has been a significant decrease in visits ranging from 20% to 64%.1–5 Despite there being a decrease in visits, there was an increase in admission and increase in emergency department (ED) acuity.3 When people did come to the emergency department it appeared to be for urgent and emergent medical issues. The presence of nonurgent complaints declined.1–4 Emergency departments see patients with all chief complaints; however, musculoskeletal complaints make up about 15–20% of emergency department visits annually.6,7 In the United States, there is an annual incidence of 1130 upper extremity injuries per 100,000 people.8 Approximately 7.4% percent require admission.9 Through the initial surge of the COVID-19 pandemic, emergency departments have seen a significant decrease in visits yet a rise in admissions.1–5,10 At a children’s hospital in Montreal, emergency department visits declined by 72% in the year 2020.10 In the UK, there was a 59% decrease in back pain, 79% decrease in neck pain and a 60% decrease in extremity pain during the pandemic.5
Even though there has been a decrease in musculoskeletal complaints overall during the pandemic, it is hypothesized that the percentage of significant injuries such as fractures, dislocations, neurovascular injuries, or injuries requiring surgery (such as open fractures) within twenty-four hours of the visit increased.1–5,9 The objective of this study was to investigate the impact of COVID-19 on upper extremity musculoskeletal injuries and the incidence of significant injuries compared to the pre-COVID-19 era.
Methods
Study Design and Setting
A retrospective single site analysis of electronic medical record (EMR) data was conducted at a Midwestern Level 1 Trauma Center and tertiary care academic emergency department from March-August 2019 and March- August 2020. The Mercy Health Youngstown, LLC Institutional Review Board (IRB) approved the study and a HIPAA waiver was granted. Informed consent was waived according to the Common Rule for retrospective studies.
Selection of Participants
Any patient adults or children who presented to the emergency department from March-August of 2019 and March-August 2020 was enrolled. All patients who presented as poly-trauma patients (trauma team or trauma alert) were excluded from the analysis.
Interventions
EPIC SlicerDicer is an EMR-based self-service query that allows users to view different patient populations and characteristics. It was used to generate a report of upper extremity injury chief complaints. Prior to the actual study, the first four authors ran a pilot study using the SlicerDicer methodology to run a report of shoulder injuries and evaluate the proposed data collection tool. This was performed utilizing a one-week time frame comparing October 2019 with October 2020. The purpose of this was to evaluate the proposed methodology.
Once proof of concept demonstrated the methodology was viable, a formal report for the periods of March-August of 2019 and March-August 2020 was run to demonstrate upper extremity injury chief complaints including: the shoulder, arm, elbow, wrist, hand, and fingers during the predefined study periods. Significant injuries were defined a priori as fractures, dislocations, neurovascular injuries, or injuries requiring surgery within twenty-four hours of the emergency department visit. Once the report of upper extremity injury chief complaints had been compiled a group of emergency medicine resident and faculty physicians, and one clinical pharmacist, who were all blinded to the study hypothesis, were formally trained to abstract the records. Training included how to review the patient records and complete the data collection instrument.
Measurement
All collected data were explicitly enumerated on the data collection instrument. The blinded reviewers were provided with an instruction sheet that reiterated what they were taught in a formal training session. The reviewers were instructed how to find the appropriate variables including demographic data, comorbidities, chief complaints, neurovascular injury data, radiographic results, and surgical records. They were also instructed on the appropriate procedures to follow if there was information missing. They were provided with the medical record numbers of each subject they were assigned. The record reviewers each did three sham record reviews and data collection forms under the supervision of the first two authors. After the blinded reviewers completed their record review, seven percent of the records that each one had reviewed were exchanged with other reviewers and they independently and blindly performed a second review of those records. A scheduled meeting between each reviewer and the unblinded principal investigators occurred at the end of the reviewer’s data collection process to answer questions and resolve issues and conflicts associated with data abstraction prior to unblinding the reviewers to the hypothesis. This allowed for reviewer process quality check and kappa calculation of inter-observer variability. Everyone with access to the patient data had formal HIPAA training as well as appropriate CITI training for involvement in a retrospective record review.
Outcomes
The primary outcome of this study is the number of significant injuries presenting to the emergency department pre-COVID19 compared to the initial pandemic surge. No additional outcomes were measured.
Analysis
Demographic factors were assessed using descriptive statistics and presented as means and standard deviations or sample size and percentages. The type of significant injury (fracture, dislocation, neurovascular injury, and operative intervention within 24 hours) also utilized descriptive statistics and are presented as sample size and percentages. Chi-square tests were used to examine differences for significant injuries by year; independent student test was used to evaluate age by year. Statistical significance was defined as a p-value less than 0.05. All analyses were conducted with SPSS statistical software (Chicago, IL: SPSS Inc.). Each reviewer performed an extra five chart reviews from another reviewers list as to allow for kappa calculation for inter-observer reliability. An institutionally employed PhD trained statistician performed the formal data analysis.
Results
Characteristics of Subjects
Subject demographics were consistent across the years (see Figure 1) as 66% were male in 2019 and 64.9% were male in 2020. This was similar in ethnicity with 41.9% and 42.9% nonwhite in 2019 and 2020, respectively. Comorbidities were also similar across with similar percentage of subjects with COPD, hypertension, congestive heart failure, diabetes mellitus, mental health disorders and coronary artery disease in the two years.
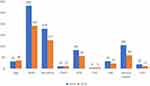 |
Figure 1 Demographical data of subjects and comorbidity rates. |
Main Results
The proportion of significant upper extremity injury prevalence was 25.2% (108/429) in 2019, increasing to 39.9% (118/296) (Chi Square = 17.617, p < 0.001) in 2020.
A total of 55,452 Emergency department visits during the study between the periods March 1, 2019 and August 31, 2019 and March 1, 2020 and August 31, 2020 were evaluated. Visits not having an upper extremity injury as their chief complaint were excluded from the analysis. This led to 429 patients in 2019 and 296 patients in 2020 for a total of 725 patient charts (see Figure 2 for graphic depiction).
 |
Figure 2 Total included subjects with subsequent breakdown for mined data. |
During the initial pandemic surge, from March thru August, total ED visits declined 22%, from 31,157 in 2019 to 24,295 in 2020. Upper extremity injury presentations also declined 31% during the same interval, from 429 in 2019 to 296 in 2020. Overall incidence of upper extremity injuries by period was similar at 1.4% versus 1.2%. The absolute number of significant upper extremity injury cases was also similar. In 2019, there were 108 significant injuries as compared to 118 significant injuries during 2020. Percent agreement among chart reviewers was strong with a kappa of 76%. The alternating chart audits were retained in the final analysis. The percentage of significant injuries increased from 25.2% to 39.9% Chi squared=17.617 (p < 0.001).
The prevalence of significant injuries is summarized in Table 1. The total number of significant injuries recorded exceeds the total number of subjects with significant injuries as one subject could have had more than one significant injury. For example, a subject could have had a fracture and a dislocation categorized as two significant injuries listed in the table.
 |
Table 1 Incidence of Significant Injury per Total Upper Extremity Presentations |
Discussion
Musculoskeletal disorders encompass a wide range of complaints. True musculoskeletal emergencies are rare; a previous study found they made up 0.5% of musculoskeletal presentations while 80.4% did not have a condition requiring urgent or emergent specialist consultation.11 As with multiple other studies during the COVID-19 pandemic, our emergency department visits declined. In our study, we saw a 22% decrease in visits overall during the two time periods as well as a 31% decrease in upper extremity musculoskeletal injury presentations. Despite the decrease, our study demonstrates an increased absolute number of patients with significant upper extremity injuries and more importantly a statistically significant increase in the percentage of patients with serious upper extremity injuries (25.2% to 39.9%). We analyzed all upper extremity injury chief complaints within our prespecified time periods as a surrogate for typically non-life-threatening patient presentations. We found that complaints that are typically less likely to be associated with a serious outcome were more likely to have a serious injury during the pandemic than prior.
In the beginning of the pandemic, ED visits decreased. Visits decreased from 20–64% worldwide (1–5). Despite there being a decrease in visits there was an increase in the admission rate and an increase in ED acuity.3 Our findings were consistent with a 14.7% total increase in serious injuries in our cohort.
We specifically looked at musculoskeletal complaints but believe this might be generalized to other chief complaints. As the public weighed risk vs benefit for ED presentation, generally those injuries or complaints which were more serious appear to have outweighed the risk of not being evaluated. Less serious, non-life or limb threatening injuries appear to have been managed in a setting with less risk of viral exposure. We believe that as a specialty we must have increased vigilance for what are typically minor complaints that do present to the ED during pandemic and other resource limited times as the patients have preselected themselves as being more likely to have a significant condition. Emergency provider gestalt during non-pandemic times needs to be adjusted during a pandemic.
Limitations
Weaknesses in our study include the failure to record the mechanism of injury as this may have actually changed during the pandemic. There were reported increases in interpersonal violence and alcohol abuse during the quarantine periods associated with the initial pandemic wave.12,13 Surgery within twenty-four hours could have been performed at an outlying institution and we would not have access to that information. Due to the retrospective nature of our experiment, we were dependent upon findings documented in the EMR. It is unlikely a neurovascular injury would not have been documented. If this had occurred, the patient would have presumably returned and been included in our data set on the subsequent day. Joint subluxations were not pre-defined as a significant injury, but one can conclude that a subluxation can cause joint instability and have an increased risk of morbidity. Acromioclavicular separations are technically a dislocation and were not specifically addressed with the blinded reviewers prior to abstracting which led to a minor inconsistency between reviewers. This design flaw lowered the inter-observer reliability. A limitation related to the retrospective nature of this study was patient identification based on documented chief complaints. Only those with upper extremity injuries were included and this would have excluded those who were triaged with a complaint of upper extremity pain. The inclusion of subjects was dictated by the triage process occurring on the day of the patient presentation and subjects were incorporated depending on the verbiage used. This could have missed a subset of patients if they were documented as upper extremity pain only, but this limitation applied to both periods. An additional significant limitation of this study is the single site nature of this experiment and the limited external validity of this sample. Readers need to compare the demographics of this population (Table 1) to their own patient populations when making conclusions about the findings.
Conclusion
Our study demonstrated that COVID-19 decreased overall visits to the ED but increased the incidence of significant injuries associated with musculoskeletal complaints. Musculoskeletal complaint may be a representative example of what we believe could be a larger trend with all chief complaints. To our knowledge, our study is unique in that it compared exclusively groups of patients with musculoskeletal injuries in the pre-COVID and COVID-19 eras. Other studies have focused on total emergency department volume, all chief complaints, and admission percentages rather than traditionally lower acuity chief complaints. This study allows insight into non-cardiovascular or respiratory ED patients and how the pandemic led to an increase in the severity of the patients with typically less serious complaints. Increased vigilance of traditionally lower acuity complaints is indicated during pandemic type situations when patients associate ED evaluation with higher personal risk of harm related to the visit.
Acknowledgment
David Gemmel, PhD for statistical help and analysis of the data.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Giamello JD, Abram S, Bernardi S, et al. The emergency department in the COVID-19 era. Who are we missing? Eur J Emerg Med. 2020;27(4):305–306. doi:10.1097/MEJ.0000000000000718
2. Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38(9):1732–1736. doi:10.1016/j.ajem.2020.06.007
3. Jeffery MM, D’Onofrio G, Paek H, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi:10.1001/jamainternmed.2020.3288
4. Butt AA, Azad AM, Kartha AB, et al. Volume and acuity of emergency department visits prior to and after COVID-19. J Emerg Med. 2020;59(5):730–734. doi:10.1016/j.jemermed.2020.08.013
5. Dowell RJ, Ashwood N, Hind J. Musculoskeletal attendances to a minor injury department during a pandemic. Cureus. 2021;13(2):e13143. doi:10.7759/cureus.13143
6. United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States (BMUS). BoneandJoint, org; 2014. Available from: https://www.boneandjointburden.org/docs/The%20Burden%20of%20Musculoskeletal%20Diseases%20in%20the%20United%20States%20(BMUS)%203rd%20Edition%20(Dated%2012.31.16).pdf.
7. De Lorenzo RA, Mayer D, Geehr EC. Analyzing clinical case distributions to improve an emergency medicine clerkship. Ann Emerg Med. 1990;19(7):746–751. doi:10.1016/s0196-0644(05
8. Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand. 2012;7(1):18–22. doi:10.1007/s11552-011-9383-z
9. Wenzinger E, Rivera-Barrios A, Gonzalez G, et al. Trends in upper extremity injuries presenting to US emergency departments. Hand. 2019;14(3):408–412. doi:10.1177/1558944717735943
10. Keays G, Friedman D, Gagnon I. Injuries in the time of COVID-19. Les blessures au temps de la COVID-19. Health Promot Chronic Dis Prev Can. 2020;40(11–12):336–341. doi:10.24095/hpcdp.40.11/12.02
11. Bellan M, Molinari R, Castello L, et al. Profiling the patients visiting the emergency room for musculoskeletal complaints: characteristics and outcomes. Clin Rheumatol. 2016;35(11):2835–2839. doi:10.1007/s10067-016-3328-4
12. Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110:106532. doi:10.1016/j.addbeh.2020.106532
13. Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38(12):2753–2755. doi:10.1016/j.ajem.2020.04.077
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
