Back to Journals » Journal of Pain Research » Volume 10
Ultrasound-guided rectus sheath block, caudal analgesia, or surgical site infiltration for pediatric umbilical herniorrhaphy: a prospective, double-blinded, randomized comparison of three regional anesthetic techniques
Authors Relland LM, Tobias JD , Martin D, Veneziano G , Beltran RJ , McKee C , Bhalla T
Received 18 June 2017
Accepted for publication 22 August 2017
Published 9 November 2017 Volume 2017:10 Pages 2629—2634
DOI https://doi.org/10.2147/JPR.S144259
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Katherine Hanlon
Lance M Relland,1,2 Joseph D Tobias,1–3 David Martin,1,2 Giorgio Veneziano,1,2 Ralph J Beltran,1,2 Christopher McKee,1,2 Tarun Bhalla1,2
1Department of Anesthesiology and Pain Medicine, Nationwide Children’s Hospital, 2Department of Anesthesiology and Pain Medicine, The Ohio State University College of Medicine, 3Department of Pediatrics, Nationwide Children’s Hospital, The Ohio State University College of Medicine, Columbus, OH, USA
Background: Umbilical hernia repair is a common pediatric surgical procedure. While opioid analgesics are a feasible option and have long been a mainstay in the pharmacological intervention for pain, the effort to improve care and limit opioid-related adverse effects has led to the use of alternative techniques, including regional anesthesia. The current study prospectively compares the analgesic efficacy of three techniques, including caudal epidural blockade, peripheral nerve blockade, and local wound infiltration, in a double-blinded study.
Patients and methods: A total of 39 patients undergoing umbilical hernia repair were randomized to receive a caudal epidural block (CDL), ultrasound-guided bilateral rectus sheath blocks (RSB), or surgical site infiltration (SSI) with local anesthetic. Intraoperative anesthetic care was standardized, and treatment groups were otherwise blinded from the intraoperative anesthesiology team and recovery nurses. Postoperatively, the efficacy was evaluated using Hannallah pain scores, Aldrete recovery scores, the need for intravenous fentanyl, and the time to discharge.
Results: Each cohort was similar in terms of age, weight, premedication dosing, length of case, intraoperative and postoperative fentanyl requirements, and time to tracheal extubation. Among the three cohorts, there were no significant differences noted in terms of pain scores or time to recovery.
Conclusion: All the three techniques provided effective analgesia following umbilical hernia repair. Our findings offer effective and safe analgesic options as alternatives to the neuraxial (caudal) approach.
Keywords: caudal, pediatric, rectus sheath, regional anesthesia, umbilical hernia
Background
Umbilical hernias develop commonly in infants and reach a maximal size by the first month of life. They make up 14% of abdominal hernias and occur in approximately one of six children.1,2 The incidence decreases to 2–10% in children older than 1 year of age, and while most umbilical hernias close spontaneously before this time, the incidence of incarceration or strangulation may be as high as 10–20%.2,3 Although umbilical herniorrhaphy is a common pediatric outpatient surgical procedure, it may be associated with significant postoperative pain. Historically, the mainstay of pediatric analgesia has been opioid-based therapy. While this approach is generally safe, its potential for adverse effects has prompted the use of alternative analgesic methods in infants and children.4 Although caudal epidural blockade has been the most commonly used pediatric regional anesthetic technique, effective analgesia in a variety of circumstances is possible with the use of peripheral nerve blockade even in children.5-7 Additionally, peripheral nerve blockade may have a lower incidence of adverse effects when compared with neuraxial techniques, including caudal epidural analgesia.8
With respect to umbilical hernia repair in the pediatric population, the rectus sheath block (RSB) has been established as a modality for pain management.9-12 Popularity of the RSB has increased both due to its opioid-sparing effects and minimizing adverse effects such as itching, nausea, and vomiting and due to the advent of ultrasound guidance, which has allowed for significant improvements in safety and accuracy of this procedure.9,13-17 Despite the demonstrated efficacy of neuraxial and peripheral nerve blockade with regard to opioid use, there are relatively few prospective, direct comparisons of the respective regional techniques in an otherwise standardized setting. In the adult population, continuous infusion into the rectus sheath may provide equivalent analgesia to epidural analgesia following laparotomy for colorectal surgery or even superior pain relief following laparoscopic cholecystectomy when compared to the intraperitoneal instillation of a local anesthetic agent.18,19 In children, significant differences have been noted between an RSB approach and surgical wound infiltration in the context of umbilical hernia repair, but the administration of the local anesthetic agent by the surgeon occurred at the end of surgery in these studies.20,21 This may have biased the results in favor of the RSB, based on anticipated differences in the intraoperative requirement of opioids. Our study is unique in that it provides a concurrent comparison of three separate regional anesthetic methods for pediatric umbilical hernia repair. After initiating the study with a pairwise comparison of RSB to the caudal epidural block (CDL), we expanded the study to include a third cohort as a further point of reference, which was treated with pre-incisional surgical site infiltration (SSI) of local anesthetic by the surgeon.
Patients and methods
Study design
We conducted a prospective, double-blinded, randomized comparison of three patient cohorts following registration at www.clinicaltrials.gov (NCT01394523, TBhalla, 07/11/2011). The study was performed with ethical approval by the Institutional Review Board of the Nationwide Children’s Hospital, OH, USA. Written informed consent was obtained from the parents of all children involved in the study, and where appropriate, assent was obtained from the child. To be included in the study, pediatric patients presenting for umbilical hernia repair needed to be of American Society of Anesthesiologists (ASA) physical status I or II. Patients with comorbid cardiac, pulmonary, or neurological diseases or those having concomitant procedures (circumcision, orchidopexy, etc.) were excluded from the study. The time period for inclusion had no set end point initially, but was to end when reaching 25 subjects per group based on the power analysis and inclusion of a third experimental group as detailed below. Treatment was standardized with exception of the experimental variable, which was based on one of the three treatments groups: CDL, RSB, or SSI. The primary outcome measured was postoperative observational pain score, obtained using a Hannallah pain scale, and we also compared length of surgical procedure, anesthesia time (induction to tracheal extubation), recovery scores using the Aldrete system, and postoperative requirement for analgesics.22,23 Other secondary measurements included time from case completion to endotracheal extubation, intraoperative end-tidal inhalational agent, intraoperative requirement for supplemental fentanyl, and time to discharge. Demographic data such as patients’ age, sex, and weight were also collected. The respective Hannallah and Aldrete scores were assessed at 5, 10, 20, and 30 minutes after tracheal extubation.
Anesthetic management
Premedication with oral midazolam was provided at the discretion of the attending anesthesiologist in the preoperative holding area. All patients underwent standard mask induction with nitrous oxide and sevoflurane in oxygen followed by placement of an intravenous cannula. For blinding purposes, in the absence of the primary anesthesiology providers, a specialized regional anesthesiology team took over patient care in the operating room (OR) after induction of anesthesia until draping of the patient for surgery. During this time, the regional anesthesiologist or surgeon performed the CDL, RSB, or SSI, respectively, based on a computer-generated random assignment. Maintenance anesthesia consisted of isoflurane titrated to keep heart rate and blood pressure within 10% of baseline values. If these parameters could not be maintained with an isoflurane end-tidal concentration of ≤2%, supplemental fentanyl (1 µg/kg) was administered. Upon completion of the surgical procedure, the patient’s trachea was extubated and patient care was transferred to a provider in the post-anesthesia care unit (PACU). An independent observer, who was blinded to the type of regional anesthesia that was provided in the OR, assigned the appropriate Hannallah and Aldrete scores at the allotted times. A standardized fentanyl dose of 1 µg/kg was provided in the PACU for pain scores >4 and reassessed until they dropped below this level. Patients were then discharged upon achieving an Aldrete score of ≥9.
Regional treatments
Patients who weighed up to 20 kg in the CDL group received 1.5 mL/kg of 0.2% ropivacaine and those who weighed >20 kg received 1.2 mL/kg to a maximum of 30 mL/kg. The relatively higher volumes used for the CDL were designed to provide more cephalad spread for coverage of the surgical procedure, but remained in line with established dosing guidelines for these blocks. Following a previously described technique, the RSB group was treated bilaterally with 0.1 mL/kg of 0.2% ropivacaine per side and administered at the T9–T10 level under ultrasound guidance.15 For those patients who were randomized into the SSI cohort, the surgeon injected either 0.5 mL/kg of 0.5% bupivacaine or 1 mL/kg of 0.25% bupivacaine based on the surgeon’s discretion in line with his or her standard practice. All the aforementioned local anesthetic preparations contained 5 µg/mL of epinephrine.
Statistical analysis
Our initial study design was powered to detect a one standard deviation difference in postoperative pain scores between CDL and RSB, which yielded a sample size requirement of 18 patients in each group to achieve 80% power for a 95% confidence level with an unpaired t-test. To include the interests of our surgical colleagues, we added a third group (SSI) to the design prior to study initiation with plans to enroll 25 patients in each group to account for possible attrition from the study or missing data. A relatively low rate of enrollment prompted an interim review 5 years into the study. During this time, 78 patients met criteria for the study based on preliminary screening and were approached accordingly. Half of these patients were excluded from the study (n = 39), mostly due to refusal to participate (n = 27, 69.2%) and also due to the presence of comorbidities (n = 4, 10.3%), inappropriate patient weight (n = 4, 10.3%), or surgical factors (n = 4, 10.3%). Subsequent conditional power analysis, using data on the Hannallah pain score in the PACU, yielded an anticipated power of 6.8% for demonstrating a significant difference in this outcome between the CDL and RSB groups if the study were to proceed as planned. Given the statistical futility and impracticality of continuing the study, we concluded with a total of 39 patients, distributed equally among the three cohorts. Data were analyzed using GraphPad Prism version 7.00 for Windows (GraphPad Software, Inc., La Jolla, CA, USA; www.graphpad.com). We compared baseline patient characteristics and perioperative measurements using one-way analysis of variance (ANOVA) and the chi-square test for continuous and categorical data, respectively. Hannallah and Aldrete scores were compared using the Kruskal–Wallis rank sum test. Pairwise comparisons were corrected for multiple comparisons using the Tukey and Dunn’s tests for ANOVA and Kruskal–Wallis rank sum, respectively. Statistical significance would be considered at a P-value of ≤0.05.
Results
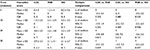
Each group consisted of 13 patients, all of whom contributed to the analysis with exception of one failed block in the CDL group. There were no significant differences between groups in terms of age, weight, and sex distribution (Table 1). Length of surgery, anesthesia time, and the time to tracheal extubation were also similar. All groups required comparable amounts of intraoperative opioid and inhaled anesthetic agent, as well as having an equivalent need for postoperative fentanyl. As a whole, fewer than half of the patients in our study required analgesic intervention in the PACU, ranging from 38.4% to 53.8% when considering the treatment groups separately. While the only parameter left to the discretion of the primary anesthesiology team was provision of oral midazolam, we ruled this out as a factor insofar as all groups received similar quantities of premedication. A regrouped analysis based on administration of premedication showed no significant difference between groups for any of the measured parameters, so the provision of midazolam preoperatively did not demonstrate an influence on the results of this study.
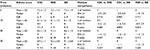
An assessment of pain in the PACU using the Hannallah scoring system revealed little to no pain in the first 5–10 minutes after tracheal extubation (Table 2). The highest median pain scores were achieved at the 20-minute assessment period in all groups, with a possibility of an increase in pain scores relatively sooner in the RSB and SSI groups when compared to the CDL cohort. However, there were no statistically significant differences overall between the treatment groups. While the uncorrected confidence interval for difference of medians between CDL and SSI Hannallah scores at the 20-minute time point did not include zero, correction for multiple comparisons suggested a lack of statistical significance. Similarly, each cohort displayed a similar recovery profile, all reaching a median Aldrete score high enough for discharge by 20 minutes after tracheal extubation (Table 3). In absolute terms, 78.9% of all patients had an Aldrete score ≥9 by 30 minutes after tracheal extubation, ranging from 76.9% to 83.3% when considering the groups separately. Of note, there were no significant differences between groups in terms of analgesic requirements, the bulk of which were nonopioid based, and between the 30-minute time point and time to discharge, and there were also no significant differences between groups in terms of length of stay in the hospital.
Discussion
Our study provides a direct, concurrent comparison of three separate regional anesthetic modalities that were provided preoperatively in the context of superficial abdominal wall surgery in a pediatric population. Because the studied interventions were performed at the same time relative to surgical incision, this permits a fair assessment of both the respective intraoperative and postoperative impacts of these techniques. Despite difficulty in enrolling the planned number of patients for this study, the lack of variability between treatment groups provides fundamental implications for the postoperative care of these patients.
Our data are in alignment with previous work that reported adequate and equivalent analgesia between the RSB and neuraxial route as well as with other investigators who found no difference in postoperative opioid use and pain scores when comparing the RSB to local anesthetic infiltration into the surgical wound.11,18 Investigators who have used ultrasound guidance advocate the increased accuracy and safety of this approach with the RSB, thereby making it superior and more efficacious than SSI with local anesthetic. However, these distinctions were made in the context of differential timing of drug administration in these studies (pre-incision for the RSB versus postsurgical manipulation for the SSI). The lack of variability between treatment groups in our study supports the idea that deposition of local anesthetic at one of the multiple sites along the nociceptive pathway could provide a similar analgesic effect when applied pre-incision in the context of minor surgical procedures. In recognition that SSI may have a relatively quick onset, the relevance of timing administration could be probed further by comparison to a postsurgical SSI group. An important consideration is whether or not the lingering effects of premedication and/or use of inhaled anesthesia may have lessened any apparent differences between our studied groups. To address the former, we ruled out the influence of midazolam based on a regrouped analysis. Of note, no significant differences were apparent between groups in our study throughout the entire length of stay, which averaged 2.6 hours, and in another study that reported significance between two of the regional techniques (RSB vs. SSI), all patients were premedicated with midazolam and all received inhaled anesthesia.20 In view of this and given that the inhaled anesthetic was titrated reactively in our study, the effect of any residual general anesthetic in our study is likely negligible. The ramifications of our results could be meaningful in changing clinical practice by expanding the options that are available to anesthesiologists and surgeons. SSI with local anesthetic may be an appropriate alternative in those patients who refuse to undergo peripheral nerve blockade, in the same way that the RSB may be a good alternative for those patients in whom a neuraxial modality is contraindicated.
Conclusion
In summary, our study demonstrated equivalent opioid requirements and similar efficacy in analgesia between three regional anesthetic techniques. With the advancements in imaging technology and improved accuracy of peripheral nerve blockade, these techniques have become increasingly popular, and our data support that RSB may be used in lieu of caudal analgesia for umbilical herniorrhaphy in children. Of note, the volume of injectate required for the RSB is 60–87% smaller when compared to the CDL or SSI approach, making the former the most amenable to minimizing quantities of administered drug, which could reduce the chances of local anesthetic systemic toxicity. In cases where preoperative SSI is feasible without excessive anatomical distortion that would interfere with surgery, SSI with a local anesthetic would be an alternative means to potentially limit intraoperative opioid requirements and provide effective postoperative analgesia while limiting the time required for neuraxial or peripheral nerve blockade. Limiting the amount of opioid that is needed postoperatively and the ability to minimize the quantity of prescription medication upon discharge could also improve patient safety.
Acknowledgments
We thank Julie Rice and Dmitry Tumin for their contributions in data collection, statistical analysis, and review of the manuscript. This report was previously presented, in part, at the conference of Society for Pediatric Anesthesia in March 2017.
Disclosure
The authors report no conflicts of interest in this work.
References
Katz DA. Evaluation and management of inguinal and umbilical hernias. Pediatr Ann. 2001;30(12):729–735. | ||
Brandt ML. Pediatric hernias. Surg Clin North Am. 2008;88(1):27–43. | ||
Kapur P, Caty MG, Glick PL. Pediatric hernias and hydroceles. Pediatr Clin North Am. 1998;45(4):773–789. | ||
Morton NS, Errera A. APA national audit of pediatric opioid infusions. Paediatr Anaesth. 2010;20(2):119–125. | ||
Tobias JD. Brachial plexus anaesthesia in children. Pediatric Anesth. 2001;11(3):265–275. | ||
Tobias JD. Regional anaesthesia of the lower extremity in infants and children. Paediatr Anaesth. 2003;13(2):152–163. | ||
Ross AK, Eck JB, Tobias JD. Pediatric regional anesthesia: beyond the caudal. Anesth Analg. 2000;91(1):16. | ||
Giaufré E, Dalens B, Gombert A. Epidemiology and morbidity of regional anesthesia in children: a one-year prospective survey of the French-Language Society of Pediatric Anesthesiologists. Anesth Analg. 1996;83(5):904–912. | ||
Willschke H, Bösenberg A, Marhofer P, et al. Ultrasonography-guided rectus sheath block in paediatric anaesthesia – a new approach to an old technique. Br J Anaesth. 2006;97(2):244–249. | ||
Ferguson S, Thomas V, Lewis I. The rectus sheath block in paediatric anaesthesia: new indications for an old technique? Paediatr Anaesth. 1996;6(6):463–466. | ||
Isaac LA, McEwen J, Hayes JA, Crawford MW. A pilot study of the rectus sheath block for pain control after umbilical hernia repair. Paediatr Anaesth. 2006;16(4):406–409. | ||
Courreges P, Poddevin F, Lecoutre D. Para-umbilical block: a new concept for regional anaesthesia in children. Paediatr Anaesth. 1997;7(3):211–214. | ||
Bakshi S, Mapari A, Paliwal R. Ultrasound-guided rectus sheath catheters: a feasible and effective, opioid-sparing, post-operative pain management technique: a case series. Indian J Anaesth. 2015;59(2):118–120. | ||
Dolan J, Lucie P, Geary T, Smith M, Kenny GN. The rectus sheath block: accuracy of local anesthetic placement by trainee anesthesiologists using loss of resistance or ultrasound guidance. Reg Anesth Pain Med. 2009;34(3):247–250. | ||
de Jose Maria B, Götzens V, Mabrok M. Ultrasound-guided umbilical nerve block in children: a brief description of a new approach. Paediatr Anaesth. 2007;17(1):44–50. | ||
Yuen PM, Ng PS. Retroperitoneal hematoma after a rectus sheath block. J Am Assoc Gynecol Laparosc. 2004;11(4):448. | ||
Dolan J, Smith M. Visualization of bowel adherent to the peritoneum before rectus sheath block: another indication for the use of ultrasound in regional anesthesia. Reg Anesth Pain Med. 2009;34(3):280–281. | ||
Tudor EC, Yang W, Brown R, Mackey PM. Rectus sheath catheters provide equivalent analgesia to epidurals following laparotomy for colorectal surgery. Ann R Coll Surg Engl. 2015;97(7):530–533. | ||
Gupta M, Naithani U, Singariya G, Gupta S. Comparison of 0.25% ropivacaine for intraperitoneal instillation v/s rectus sheath block for postoperative pain relief following laparoscopic cholecystectomy: a prospective study. J Clin Diagn Res. 2016;10(8):UC10–UC15. | ||
Flack SH, Martin LD, Walker BJ, et al. Ultrasound-guided rectus sheath block or wound infiltration in children: a randomized blinded study of analgesia and bupivacaine absorption. Paediatr Anaesth. 2014;24(9):968–973. | ||
Gurnaney HG, Maxwell LG, Kraemer FW, Goebel T, Nance ML, Ganesh A. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaesth. 2011;107(5):790–795. | ||
Hannallah RS, Broadman LM, Belman AB, Abramowitz MD, Epstein BS. Comparison of caudal and ilioinguinal/iliohypogastric nerve blocks for control of post-orchiopexy pain in pediatric ambulatory surgery. Anesthesiology. 1987;66(6):832–834. | ||
Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7(1):89–91. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.