Back to Journals » Clinical Interventions in Aging » Volume 9
Twelve weeks of BodyBalance® training improved balance and functional task performance in middle-aged and older adults
Authors Nicholson V, McKean M, Burkett B
Received 25 July 2014
Accepted for publication 7 August 2014
Published 6 November 2014 Volume 2014:9 Pages 1895—1904
DOI https://doi.org/10.2147/CIA.S71769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Vaughan P Nicholson, Mark R McKean, Brendan J Burkett
School of Health and Sport Sciences, University of the Sunshine Coast, Sunshine Coast, QLD, Australia
Purpose: The purpose of the study was to evaluate the effect of BodyBalance® training on balance, functional task performance, fear of falling, and health-related quality of life in adults aged over 55 years.
Participants and methods: A total of 28 healthy, active adults aged 66±5 years completed the randomized controlled trial. Balance, functional task performance, fear of falling, and self-reported quality of life were assessed at baseline and after 12 weeks. Participants either undertook two sessions of BodyBalance per week for 12 weeks (n=15) or continued with their normal activities (n=13).
Results: Significant group-by-time interactions were found for the timed up and go (P=0.038), 30-second chair stand (P=0.037), and mediolateral center-of-pressure range in narrow stance with eyes closed (P=0.017). There were no significant effects on fear of falling or self-reported quality of life.
Conclusion: Twelve weeks of BodyBalance training is effective at improving certain balance and functional based tasks in healthy older adults.
Keywords: postural control, yoga, tai chi, center of pressure, exercise
Introduction
Age-related changes in balance and functional task performance are well-established and evident from the fourth and fifth decades of life in men and women.1,2 Deficits in balance are associated with falls,3 difficulties with activities of daily living,4 and poor survival5 in older adults. Fortunately, appropriate exercise can improve balance performance6 and contribute to improved mobility,7 independence, and a reduction in the risk of falling.8 Interventions utilizing traditional or holistic exercises, such as tai chi,9 Pilates,10 and yoga,11 have all been found to improve balance in older adults. A number of authors have also highlighted the importance of delivering preemptive exercise interventions to middle-aged and older adults before deteriorations in balance and mobility lead to adverse outcomes.12,13 Additionally, such interventions may reduce fear of falling and improve quality of life.14 These aspects are important, as fear of falling is associated with a reduction in physical activity and subsequent increased fall risk,15 while improving health and quality of life are important motivators for exercise in older adults.16
While there are various exercise options that are capable of improving balance in middle-aged and older adults, gym-based activities are becoming increasingly popular in this age-group.17,18 Group fitness classes that incorporate appropriate challenges to balance are likely to be successful at improving balance outcomes. BodyBalance® (Les Mills) (BodyFlow™ in the US) is one gym-based activity that has the potential to promote improvements in balance, as it is comprised of yoga, tai chi, and Pilates elements, all of which in isolation can successfully improve balance.7,19,20 The prechoreographed class is available in over 14,000 fitness facilities globally, so its potential reach is vast. It has been subject to just one peer-reviewed study, in which benefits in strength, state – anxiety, and flexibility were found in young and middle-aged adults.21 The effect of BodyBalance on balance and functional task performance has yet to be determined in middle-aged or older adults.
The primary aim of this study was to determine whether 12 weeks of BodyBalance classes would improve balance and functional task performance in healthy, active adults aged over 55 years. Secondary aims were to determine the effect of BodyBalance training on fear of falling and self-reported quality of life. It was hypothesized that 12 weeks of BodyBalance training would improve measures of balance and functional task performance without having an effect on fear of falling or self-reported quality of life.
Participants and methods
Study design and intervention
A two-group, repeated-measures, randomized controlled trial was used to determine the effect of a 12-week BodyBalance training program. Men and women aged 55–75 years not involved in formal resistance or balance training in the previous 6 months were invited to participate in the study. All participants were physically active, taking part in regular exercise, such as walking, cycling, and swimming. Exclusion criteria included: acute or terminal illness, myocardial infarction in the past 6 months, recent low-impact fracture, or any condition that would interfere with moderate-intensity exercise participation. Participants were recruited through an adult-education facility and via local advertising. All participants provided written informed consent conforming to the Declaration of Helsinki before participating in the study. The study protocol was approved by the Human Research Ethics Committee of the University of the Sunshine Coast.
Participants were allocated to either the intervention (BodyBalance [BB]) or control (CON) group in a 1:1 ratio using a computer generated random-number list (stratified for age and sex). The participants were informed of their allocation after baseline data collection.
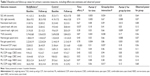
Participants in the BB group undertook 12 weeks of BodyBalance classes. Participants were provided with free access to a local fitness facility, and were encouraged to attend two scheduled classes per week. All classes were instructed by experienced group fitness instructors who were not associated with testing or recruitment of participants. The focus of the first 2 weeks of the intervention was for each participant to learn the exercises and postures of the class appropriately. As such, the transitions between postures were deliberately slow in the first 2 weeks. From week 3 onward, all classes were instructed at a level that one would expect to encounter if they took part in a BodyBalance class at a local gym. The class involves a variety of poses and exercises that are derived from yoga, tai chi, and Pilates (Table 1). The class instructor provided basic, intermediate, and advanced options for each pose or exercise. CON-group participants were encouraged to continue with their normal activities, but did not take part in any class.
  | Table 1 Typical BodyBalance® class components |
Measures
All measures were completed during a single session for each participant at baseline and follow-up. Two questionnaires were completed at the start of the session to assess fear of falling and self-reported quality of life. The assessment of balance on a force platform was then conducted followed by a battery of established clinical balance assessments and functional tasks.
Questionnaires
The 10-item Iconographical Falls Efficacy Scale22 was completed at the start of each balance-assessment session to provide an indication of each participant’s fear of falling. The Short Form (36) Health Survey (SF-36)-v2 (Australian version) was also completed at baseline and follow-up to assess the self-reported quality of life of each participant. SF-36v2 percentage scores were converted to t-scores using Health Outcomes™ Scoring Software 4.5 (QualityMetric, Lincoln, RI, USA) for analysis and interpretation.
Center-of-pressure balance assessment
Balance and functional task assessments were conducted at baseline and immediately postintervention. All measures were assessed with participants unshod. Participants performed a series of four different standing-balance tasks on a strain-gauge 4060-08 force platform (Bertec, Columbus, OH, USA). The force plate was calibrated in accordance with the manufacturer’s recommendations. Signal processing and data analysis were performed using Track Manager (Qualisys, Gothenburg, Sweden). Data were sampled at a rate of 50 Hz, with a cutoff frequency of 10 Hz. The balance tasks were comfortable stance (eyes open and closed) and narrow stance (eyes open and closed). For the comfortable stance positions, participants stood with their feet at pelvic width, while for the narrow stance position they stood with their feet together with the first metatarsal–phalangeal joints and medial malleoli touching. Participants were instructed to keep their hands by their sides and to remain as still as possible while looking straight ahead. Two successful repetitions of 30 seconds in each position were performed, with 60 seconds’ rest between trials. The same order was followed for all participants at each testing session: comfortable stance, eyes open, followed by comfortable stance, eyes closed, then narrow stance, eyes open, and finally narrow stance, eyes closed. The mediolateral center-of-pressure (COP) range for each stance position was used for data analysis. The mediolateral COP range is the distance between the maximal and minimal position of the COP in the frontal plane.23 High test–retest reliability for this COP parameter was found in pilot testing with 20 similar-aged participants (intraclass correlation coefficient 0.86).
Single-leg balance
With their eyes open, subjects raised the nonstanding leg so that the raised foot was near but not touching the ankle of the stance limb and maintained that position for as long as long as they could up to a maximum of 60 seconds.24 Time was measured with a digital stopwatch. Timing commenced when the subject lifted the foot off the floor, and timing ceased when the subject either 1) used their arms (moved arms away from their side) to balance, 2) moved the weight-bearing foot to maintain balance, 3) a maximum of 60 seconds had elapsed, 4) placed their nonstanding leg on the ground, or 5) required assistance to maintain balance. Two successful trials on each leg were recorded (left leg assessed first), and the mean of the two scores was used for analysis.
Functional reach
The subject stood with feet a comfortable distance apart behind a line perpendicular and adjacent to a wall (foot position noted for each subject). Subjects were asked to make a fist and to raise the arm closest to the wall to shoulder height, and the position of the third metacarpal was recorded. The subject was then instructed to keep the feet flat on the floor and lean forward as far as possible without losing balance, touching the wall, or taking a step.25 The position of the third metacarpal was recorded at the point of furthest reach. The functional reach is the difference between the two measures. Two measures were recorded for the right side (left side was used if right shoulder mobility was limited), and the mean used for analysis.
Lateral reach
The subject stood with their back to (but not in contact with) a wall. Feet were placed in a standardized position with 0.1 m between the most medial aspects of the heels, with each foot angle out at 30°. To ensure accurate recording of the initial hand position, subjects stood for 10 seconds with both arms abducted and maintained equal weight bearing, and the position of the tip of the third finger was measured. Subjects were given standardized instructions to reach directly sideward as far as possible without overbalancing, taking a step or touching the wall.26 The perceived maximal reach position was maintained for 3 seconds and recorded. The distance between the initial hand position and maximal reach position is the lateral reach. Two successful trials were performed for each side and the mean used for analysis.
Timed up and go
Subjects were seated in a normal armchair (0.44 m high) with their back against the chair. They were instructed to stand up, walk 3 meters as quickly and safely as possible past a marker on the floor, turn around, walk back to the chair, and sit down with their back against the chair.27 Time started on the command “Go” and stopped once the subject’s back was against the chair after completing the walk. The mean of two trials was used for analysis.
Normal gait speed
Subjects were instructed to stand still with their feet just behind a starting line marked with tape, and then to walk at their “normal, comfortable pace” along a 6-meter course until a few steps past the finish line after the examiner’s command of “Go”. Timing with a digital stopwatch commenced with the first footfall and stopped with the subject’s first footfall after crossing the 6-meter end line.28 The mean time for two trials was converted to gait speed (m/s) and used for data analysis.
Fast-gait speed
Subjects were instructed to stand still with their feet just behind a starting line marked with tape, and then to walk “as quickly as possible without running” along a 6-meter course until a few steps past the finish line after the examiner’s command of “Go”. Timing with a digital stopwatch commenced with the first footfall and stopped with the subject’s first footfall after crossing the 6-meter end line. The mean time for two trials was converted to gait speed (m/s) and used for data analysis.
Thirty-second chair-stand test
The 30-second chair stand test was administered using a chair without arms, with a seat height of 0.44 m. The back of the chair was placed against a wall to prevent it from moving during the test. The test began with the subject seated in the middle of the chair, feet approximately shoulder width apart and placed on the floor at an angle slightly behind the knees. Arms were crossed at the wrists and held against the chest. On the “Go” signal, the subject rose to a full stand and then returned back to the initial seated position, then completed as many full stands as possible within 30 seconds.29 The mean of two trials was used for analysis.
Floor rise to standing
The participants started in a supine position with their legs and feet together and arms by their side with palms down. Timing started on the “Go” command, and participants rose to full standing as fast as possible.30 Timing ceased when the patient was fully upright and had come to a complete stop. The mean of two trials was used for analysis.
Data analysis
All data are reported as means and standard deviation. Primary outcomes were changes in balance and functional task performance from baseline in response to the 12-week BodyBalance intervention. Secondary outcomes were changes in fear of falling and self-reported quality of life. Potential differences between groups at baseline were assessed by independent t-tests. A repeated-measures general linear model was used to determine group (BB, CON) and time (baseline, 12 weeks) effects on primary and secondary outcomes. Baseline values were used as covariates in the general linear model for any measures that were different between groups at baseline. Partial η2 was used to determine the effect size for each outcome variable. A priori power calculations were performed for the key balance variables of timed up and go (TUG) and gait speed based on previous research,10,31 indicating that a sample size of 15 participants per group would be required to provide greater than 80% power at a level of 0.05. To account for a 10% attrition rate, a total of 17 participants per group was required. Analyses were performed using SPSS (IBM, Armonk, NY, USA). Statistical significance was set at P<0.05.
Results
Study population and compliance
Twenty-eight participants aged between 57 and 73 years (BB, n=15, age 66±4.9 years; CON, n=13, age 66±5.1 years) completed all baseline and follow-up testing (Table 2). All participants were active adults living independently within the community, and did not require assistive devices for ambulation. All BB participants that started the program completed the intervention, with a mean attendance of 22±2.1 classes resulting in an overall compliance of 92%. One BB participant reported ongoing low-back pain during classes, but was able to complete the program and follow-up testing, but did require physiotherapy treatment. No other adverse events were reported during the intervention. Three participants from CON were lost to follow-up after completing baseline testing (Figure 1). There were no significant individual differences between those who withdrew and those who completed all testing for any primary or secondary outcome measure.
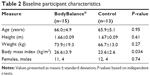  | Table 2 Baseline participant characteristics |
  | Figure 1 Project flowchart. |
Effects on balance measures and functional tasks
There were no significant differences between groups in any balance measure or functional task at baseline (Table 3). There were significant group-by-time interactions in favor of BB for the 30-second chair-stand test (F1,26=4.9, P=0.037, partial η2=0.18), the TUG (F1,26=4.8, P=0.038, partial η2=0.17) and mediolateral COP range in narrow stance, eyes closed (F1,26=6.2, P=0.017, partial η2=0.13) (Table 3 and Figures 2–4). There was a significant group-by-time interaction for single leg, stance left (F1,26=5.9, P=0.024, partial η2=0.20), indicating an increase in stance time for CON. There were significant time effects for lateral reach, left (F1,26=4.9, P=0.037, partial η2=0.18), 30-second chair-stand test (F1,26=23.0, P<0.001, partial η2=0.51), and mediolateral COP range with comfortable stance, eyes closed (F1,26=5.7, P=0.022, partial η2=0.12). These time effects all indicated an improvement between baseline and follow-up.
  | Figure 2 Values (means ± standard error) for the timed up and go (TUG) at baseline and follow-up. |
  | Figure 3 Values (means ± standard error) for the 30-second chair-stand test (CST) at baseline and follow-up. |
Effects on fear of falling and self-reported quality of life
There were no significant baseline group differences between groups for fear of falling or any self-reported quality-of-life measure (Table 4). There were no significant group-by-time interactions for fear of falling or quality-of-life measures. There was a significant time effect for bodily pain (F1,26=7.45, P=0.014, partial η2=0.29), indicating more reported pain (lower t-score) at follow-up compared to baseline for both groups.
Discussion
This study provides the first controlled evaluation of the effects of BodyBalance training on balance, functional task performance, fear of falling, and health-related quality of life in middle-aged and older adults. The results of this study partly support the hypothesis that measures of balance and function would improve after 12 weeks of BodyBalance training, and that there would be no evident improvement in fear of falling or self-reported quality of life. Greater improvements were observed for the BB group in the 30-second chair-stand test, TUG, and mediolateral COP range in comfortable stance with eyes closed. Interestingly, greater improvements were evident in the CON group for single-leg stance, left: a measure of static standing balance. There were no significant improvements in fear of falling or self-reported quality of life following the BodyBalance intervention.
The baseline values obtained for this cohort indicated that both groups were comprised of well-functioning participants with good levels of balance, low fear of falling levels, and high self-reported quality of life. For example, the mean TUG time for this cohort was over 2 seconds quicker than normative values for similar-aged healthy adults,2,27 and the physical components of self-reported quality of life were approximately 15% higher than Australian normative values.32
BodyBalance is comprised of elements from yoga, tai chi, and Pilates, so the results of this study will be discussed in the context of these interventions. The improvements in a small selection of tasks in this study are in partial agreement with previous studies that have found improvements in balance and functional tasks after yoga-,7 tai chi-,19 and Pilates-based33 interventions in similar-aged adults. The improvements in both the TUG and chair-stand test is of note, as both involve the sit-to-stand transfer: a task that represents a complex functional movement that is influenced by lower-limb strength, balance, and sensorimotor and psychological factors.34 Performance in the TUG and chair-stand tests are predictive of function and falls in older adults,35,36 so any improvement in these tasks is of benefit to even healthy and mobile older adults.
The improvement in mediolateral COP range in narrow stance with eyes closed suggests an improvement in the most challenging static balance task assessed in this study. Lower COP ranges in the mediolateral direction are typically seen in younger adults and nonfallers, while higher COP ranges in both narrow stance and normal stance positions are seen in fallers37 or those with poor clinical balance.38 The results of this study are in contrast to previous tai chi39,40 interventions that have been unable to demonstrate training-induced improvements in COP displacements in bipedal stance. The results from the current study suggest that static standing-balance improvements provided by the intervention may be best observed in more demanding balance tasks where visual cues are limited. This is supported by previous studies assessing Pilates41 and tai chi42 that have reported greater disparity in postural stability between exercising participants and controls in more demanding tasks compared to simple balance tasks. Recent work in middle-aged women demonstrated that poor performance in a balance task that confounded the use of vision and somatosensation was the only task to predict future falls.43 The inclusion of more demanding balance tasks, such as those that simultaneously challenge proprioception and vision, may have better identified any improvements provided by the intervention.
The lack of significant improvement in reaching and single leg standing tasks in the BB group was likely due to a number of factors, including the already-good balance performance of participants at baseline and the high variability of some testing measures. For example, participants in the current study had single-leg stance times approximately 10 seconds longer than previously reported normative values,44 while lateral reach was approximately 15% longer than previously reported.2 Although there was a group-by-time interaction in favor of the CON group in single-leg stance, left, it is unlikely this small improvement represents a real change, as this test lacks sensitivity in well-functioning older adults,45 although it is an appropriate tool for predicting functional decline.46 The intervention itself, although comprising elements of activities shown to improve balance, may not have been challenging enough to provide consistent improvements in balance outcome measures. As a number of options were available to participants for each exercise or pose, participants may have inadequately challenged their balance by performing less challenging options. The study duration and volume were likely sufficient to provide improvements in balance, given the positive results of training interventions ranging from 12 to 16 weeks in similar-aged cohorts.7,19,33
Balance-exercise guidelines provided by the American College of Sports Medicine recommend using activities that include: progressively difficult postures that gradually reduce the base of support; dynamic movements that perturb the center of gravity; stress to postural control muscles; or reducing sensory input.47 Like a number of other modalities, such as yoga and tai chi, BodyBalance achieves three of the four recommendations by incorporating progressively difficult postures, dynamic movements that perturb the center of gravity, and stressing postural control muscles. BodyBalance may prove to be a more effective modality if greater challenges to sensory input and dual tasking are incorporated into its choreography.
There were no intervention effects on fear of falling or self-reported quality of life. The lack of change for fear of falling was most likely due to the low baseline values for both groups. Low values represent low levels of fear, which may have produced a floor effect similar to that seen with other fear-of-falling questionnaires.48 Previous studies that have reported reduced fear of falling following balance-based interventions49,50 have typically targeted older adults with a history of falls or impaired balance, and as such those participants are more likely to have higher levels of fear that may be reduced with appropriately targeted programs. The lack of improvement in quality-of-life measures is not surprising given the high baseline scores, which would have limited the potential for improvement. The physical component scores of this cohort were approximately 15% higher than Australian norms, while mental component scores were approximately 5% higher than previously reported.32
A number of study limitations require attention. Firstly, the small sample size and low observed power for a number of measures in this study limited our ability to detect between-group differences (if differences were present). The balance-assessment tasks used in this study may not have provided enough challenge to those with good balance ability, thus creating a ceiling effect and limiting the potential for observing any improvement. Other confounding measures, such as cardiovascular parameters, were not assessed, which may have had an impact on results. As a healthy, active cohort with good balance ability was recruited for this study, the generalizability of these results in sedentary persons, recurrent fallers, or those with balance impairments cannot be determined.
Conclusion
Twelve weeks of BodyBalance training was effective at improving performance in the TUG and 30-second chair-stand test and reducing mediolateral COP range in narrow stance with eyes closed in healthy, active adults aged 59–73 years. BodyBalance training was not effective at improving single-leg balance, reaching tasks, gait speed, or floor rise to standing. BodyBalance training did not positively influence fear of falling or self-reported quality of life any more than habitual activity. It appears that BodyBalance training may be an appropriate modality for enhancing certain aspects of balance and functional performance in this age-group. Future studies should assess the effect of such training on those with impaired balance, a fear of falling, or a history of falls.
Acknowledgment
This research was supported by PhD funding provided by the Australian Fitness Network.
Disclosure
The authors report no conflicts of interest in this work.
References
Illing S, Low Choy N, Nitz J, Nolan M. Sensory system function and postural stability in men aged 30–80 years. Aging Male. 2010;13(3): 202–210. | ||
Isles RC, Low Choy N, Steer M, Nitz JC. Normal values of balance tests in women aged 20–80. J Am Geriatr Soc. 2004;52(8):1367–1372. | ||
Lord SR, Clark RD. Simple physiological and clinical tests for the accurate prediction of falling in older people. Gerontology. 1996;42(4): 199–203. | ||
Era P, Avlund K, Jokela J, et al. Postural balance and self-reported functional ability in 75-year-old men and women: a cross-national comparative study. J Am Geriatr Soc. 1997;45(1):21–29. | ||
Era P, Heikkinen E, Gause-Nilsson I, Schroll M. Postural balance in elderly people: changes over a five-year follow-up and its predictive value for survival. Aging Clin Exp Res. 2002;14(3 Suppl):37–46. | ||
Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for improving balance in older people (Review). Cochrane Database Syst Rev. 2011;11:CD004963. | ||
Tiedemann A, O’Rourke S, Sesto R, Sherrington C. A 12-week Iyengar yoga program improved balance and mobility in older community-dwelling people: a pilot randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68(9):1068–1075. | ||
Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta analysis. J Am Geriatr Soc. 2008;56(12):2234–2243. | ||
Li F, Harmer P, Fisher KJ, McAuley E. Tai chi: improving functional balance and predicting subsequent falls in older persons. Med Sci Sports Exerc. 2004;36(12):2046–2052. | ||
Kaesler D, Mellifont R, Kelly PS, Taaffe D. A novel balance exercise program for postural stability in older adults: a pilot study. J Bodyw Mov Ther. 2007;11(1):37–43. | ||
Schmid AA, Van Puymbroeck M, Koceja DM. Effect of a 12-week yoga intervention on fear of falling and balance in older adults: a pilot study. Arch Phys Med Rehabil. 2010;91(4):576–583. | ||
Low Choy N, Brauer S, Nitz J. Linking stability to demographics, strength and sensory system function in women over 40 to support pre-emptive preventive intervention. Climacteric. 2008;11(2):144–154. | ||
Daly RM, Rosengren BE, Alwis G, Ahlborg HG, Sernbo I, Karlsson MK. Gender specific age-related changes in bone density, muscle strength and functional performance in the elderly: a-10 year prospective population-based study. BMC Geriatr. 2013;13:71. | ||
Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44(5):489–497. | ||
Delbaere K, Crombez G, Vanderstraeten G, Willems T, Cambier D. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33(4):368–373. | ||
Kolt GS, Driver RP, Giles LC. Why older Australians participate in exercise and sport. J Aging Phys Act. 2004;12(2):185–198. | ||
Merom D, Cosgrove C, Venugopal K, Bauman A. How diverse was the leisure time physical activity of older Australians over the past decade? J Sci Med Sport. 2012;15(3):213–219. | ||
International Health, Racquet and Sportsclub Association. IHRSA International Report. Boston: IHRSA; 2011. | ||
Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185–1191. | ||
Newell D, Shead V, Sloane L. Changes in gait and balance parameters in elderly subjects attending an 8-week supervised Pilates programme. J Bodyw Mov Ther. 2012;16(4):549–554. | ||
Khan RS, Marlow C, Head A. Physiological and psychological responses to a 12-week BodyBalance training programme. J Sci Med Sport. 2008;11(3):299–307. | ||
Delbaere K, Smith ST, Lord SR. Development and initial validation of the iconographical falls efficacy scale. J Gerontol A Biol Sci Med Sci. 2011;66(6):674–680. | ||
Rafał S, Janusz M, Wiesław O, Robert S. Test-retest reliability of measurements of the center of pressure displacement in quiet standing and during maximal voluntary body leaning among healthy elderly men. J Hum Kinet. 2011;28:15–23. | ||
Bulbulian R, Hargan ML. The effect of activity history and current activity on static and dynamic postural balance in older adults. Physiol Behav. 2000;70(3):319–325. | ||
Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192. | ||
Brauer S, Burns Y, Galley P. Lateral reach: a clinical measure of medio-lateral postural stability. Physiother Res Int. 1999;4(2):81–88. | ||
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903. | ||
Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well functioning older people: results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10): 1675–1680. | ||
Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. | ||
Henwood TR, Taaffe DR. Improved physical performance in older adults undertaking a short-term programme of high-velocity resistance training. Gerontology. 2005;51(2):108–115. | ||
Zettergren KK, Lubeski JM, Viverito JM. Effects of a yoga program on postural control, mobility, and gait speed in community-living older adults: a pilot study. J Geriatr Phys Ther. 2011;34(2):88–94. | ||
Hawthorne G, Osborne RH, Taylor A, Sansoni J. The SF36 Version 2: critical analyses of population weights, scoring algorithms and population norms. Qual Life Res. 2007;16(4):661–673. | ||
Irez GB, Ozdemir RA, Evin R, Irez SG, Korkusuz F. Integrating Pilates exercise into an exercise program for 65+ year-old women to reduce falls. J Sports Sci Med. 2011;10(1):105–111. | ||
Lord SR, Murray SM, Chapman K, Munro B, Tiedemann A. Sit-to-stand performance depends on sensation, speed, balance, and psychological status in addition to strength in older people. J Gerontol A Biol Sci Med Sci. 2002;57(8):M539. | ||
Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: the role of physical performance. J Am Geriatr Soc. 1995;43(6):603–609. | ||
Viccaro LJ, Perera S, Studenski SA. Is timed up and go better than gait speed in predicting health, function, and falls in older adults? J Am Geriatr Soc. 2011;59(5):887–892. | ||
Melzer I, Benjuya N, Kaplanski J. Postural stability in the elderly: a comparison between fallers and non-fallers. Age Ageing. 2004;33(6): 602–607. | ||
Laughton CA, Slavin M, Katdare K, et al. Aging, muscle activity, and balance control: physiologic changes associated with balance impairment. Gait Posture. 2003;18(2):101–108. | ||
Lelard T, Doutrellot PL, David P, Ahmaidi S. Effects of a 12-week tai chi chuan program versus a balance training program on postural control and walking ability in older people. Arch Phys Med Rehabil. 2010;91(1):9–14. | ||
Chen YS, Zhou S, Cartwright C. Effect of 12 weeks of tai chi training on soleus Hoffmann reflex and control of static posture in older adults. Arch Phys Med Rehabil. 2011;92(6):886–891. | ||
Bird M, Hill KD, Fell JW. A randomized controlled study investigating static and dynamic balance in older adults after training with Pilates. Arch Phys Med Rehabil. 2012;93(1):43–49. | ||
Wong AM, Lin YC, Chou SW, Tang FT, Wong PY. Coordination exercise and postural stability in elderly people: effect of tai chi chuan. Arch Phys Med Rehabil. 2001;82(5):608–612. | ||
Nitz JC, Stock L, Khan A. Health-related predictors of falls and fractures in women over 40. Osteoporos Int. 2013;24(2):613–621. | ||
Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007;30(1):8–15. | ||
Goldberg A, Casby A, Wasielewski M. Minimum detectable change for single-leg-stance-time in older adults. Gait Posture. 2011;33(4): 737–739. | ||
Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004;52(8):1343–1348. | ||
Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7): 1510–1530. | ||
Delbaere K, Close JCT, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The falls efficacy scale international (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39(2):210–216. | ||
Zhang JG, Ishikawa-Takata K, Yamazaki H, Morita T, Ohta T. The effects of tai chi chuan on physiological function and fear of falling in the less robust elderly: an intervention study for preventing falls. Arch Gerontol Geriatr. 2006;42(2):107–116. | ||
Wolf SL, Sattin RW, Kutner M, O’Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51(12):1693–1701. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.