Back to Journals » Clinical Ophthalmology » Volume 12
Trends in the characteristics of vitrectomy in Eastern China
Authors Fang Y, Ku H, Liu Y, Gan D
Received 6 May 2018
Accepted for publication 13 August 2018
Published 10 October 2018 Volume 2018:12 Pages 1993—2000
DOI https://doi.org/10.2147/OPTH.S173251
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yuan Fang,1,* Hsiangyu Ku,1,* Yiwen Liu,1 Dekang Gan1–3
1Department of Ophthalmology and Visual Science, Eye and ENT Hospital, Shanghai Medical College, Fudan University, Shanghai 200031, China; 2Shanghai Key Laboratory of Visual Impairment and Restoration, Shanghai 200031, China; 3Key NHC Key Laboratory of Myopia (Fudan University), Laboratory of Myopia, Chinese Academy of Medical Sciences, Shanghai 200031, China
*These authors contributed equally to this work
Background: Several new instruments and techniques for pars plana vitrectomy (PPV) have been widely used in recent years, but information about the related characteristics of PPV in China is limited. To investigate the trends in the characteristics of PPV in Eastern China, an 8-year retrospective study was conducted.
Patients and methods: We collected data from patients who underwent PPV at the Eye, Ear, Nose and Throat Hospital of Fudan University, Shanghai, China, in November 2007, November 2011, and November 2015. Cases of trauma-related retinopathy were excluded. Data on the patient demographics, surgical procedures, and the prophylactic use of IOP-lowering medications were collected and analyzed.
Results: In 2015, most PPVs were conducted with a 23-gauge system, whereas all PPVs in 2007 and 2011 were conducted with a 20-gauge system. The proportions of macular disease in the population in 2007, 2011, and 2015 were 9.1%, 10.7%, and 21.5%, respectively (P<0.001). The proportion of PPV that was combined with lens extraction and intraocular lens (IOL) implantation increased significantly from 12.81% in 2007 to 25.95% by 2015 (P<0.001). The proportions of patients treated with IOP-lowering drugs in 2007, 2011, and 2015 were 27.40%, 38.20%, and 12.60%, respectively (P<0.001). In 2007, systemic carbonic anhydrase inhibitors (CAI-Ss) and beta blockers (BBs) were the two main types of prophylactic IOP-lowering drugs administered, but their use had decreased in 2015 (P<0.001). The preventive use of adrenergic agonists (AAs), topical carbonic anhydrase inhibitors (CAI-Ts), and prostaglandin analogs (PGAs) became increasingly frequent from 2007 to 2015 (P<0.05).
Conclusion: The 23-gauge system, rather than the 20-gauge system, had become the mainstream PPV instrument by 2015. The proportion of macular disease patients requiring PPV in China clearly increased, and the rate of prophylactic IOP-lowering drug use decreased by 2015.
Keywords: ocular hypertension, glaucoma, vitrectomy, macular disease, epidemiology
Introduction
Pars plana vitrectomy (PPV) is the surgical technique most frequently used to treat various retinal disorders. However, there is limited information on the demographic characteristics of patients who undergo PPV in China. In recent years, many new techniques and equipment for PPV have emerged and have been widely used in the clinical setting. For example, 23-gauge (23G), 25G, and 27G vitrectomy systems have been developed.1–3 Moreover, with advances in optical coherence tomography (OCT) and the staining technology used for PPV,4 macular diseases are more easily recognized and treated than ever before. A vitreous injection of antibody directed against vascular endothelial growth factor (VEGF) has been shown to be effective in treating vessel-related retinal diseases. All these advances have affected the characteristics of PPV procedures in the past several years.
Ocular hypertension is a common complication of PPV.5 Our previous study showed that about 20% of the patients with no history of glaucoma or ocular hypertension suffered ocular hypertension during the 1-year follow-up period after PPV,6 most in the first month after PPV.6 To reduce the incidence of early-onset ocular hypertension and the damage it causes to the optic nerve and retina, some surgeons prophylactically administer IOP-lowering drugs on postoperative day 1 after PPV in patients with a high risk of ocular hypertension.7–9 In this study, we collected data on patients who had undergone PPV at our hospital in November 2007, November 2011, or November 2015 to investigate the trends in the demographics of these patients, the procedures used for PPV, and the prophylactic use of IOP-lowering medicines from 2007 to 2015.
Patients and methods
This retrospective repeated cross-sectional study was approved by the institutional ethics committee of the Eye, Ear, Nose, and Throat Hospital of Fudan University, Shanghai, China. All procedures were performed in accordance with the ethical standards defined in the Declaration of Helsinki. All patients provided their written informed consent for the use of their medical data for research purposes.
These consecutive case series included 203 eyes in 203 patients, 279 eyes in 279 patients, and 343 eyes in 343 patients, who were hospitalized and underwent PPV at our hospital in November 2007, November 2011, and November 2015, respectively. The Eye, Ear, Nose, and Throat Hospital of Fudan University performs the largest number of PPV procedures than any other hospital in Eastern China.
The demographic information for each patient, including age, sex, systemic medical history, and refractive status, was recorded. In this study, the systemic medical history included only systemic hypertension and diabetes mellitus, which have high prevalence rates and are associated with retinopathy. All systemic diseases were diagnosed by an internist before PPV surgery was performed. IOP was measured 1 day before the operation and recorded as the preoperative IOP. The diagnoses were classified into rhegmatogenous retinal detachment (RRD), macular diseases, proliferative diabetic retinopathy (PDR), vitreous hemorrhage without PDR, and others. Macular diseases included macular hole (MH), macular schisis (MS), and epiretinal membrane (ERM). Because some patients with trauma-related retinopathy underwent PPV in the outpatient department of our hospital, their data could not be collected. The demographic data of hospitalized patients with trauma-related retinopathy were neither accurate nor reliable. Therefore, trauma-related retinal diseases were excluded from this study.
PPV was performed with a standard 20G, 23G, or 25G three-port system under retrobulbar anesthesia or general anesthesia in all patients. Filtered air, balanced salt solution (BSS), 20% sulfur hexafluoride (SF6), 14% octafluoropropane (C3F8), or silicone oil was used as the tamponade during vitrectomy. PPV was performed together with lens extraction, intraocular lens (IOL) implantation, or scleral buckling in some cases.
On postoperative day 1, all patients received topical antibiotic and topical steroid treatments. To reduce the incidence of postoperative ocular hypertension, some patients with a high risk of ocular hypertension were administered IOP-lowering drugs on postoperative day 1 before their IOPs were measured. This was defined as the prophylactic use of IOP-lowering drugs. The IOP-lowering drugs are classified as beta blockers (BBs), prostaglandin analogs (PGAs), adrenergic agonists (AAs), topical carbonic anhydrase inhibitors (CAI-Ts), or systemic carbonic anhydrase inhibitors (CAI-Ss). Because only topical BBs are used as IOP-lowering drugs at our hospital, “beta blockers” in this study refer to topical BBs. Fixed combinations of drugs are categorized as two single drugs given separately. Data on the preventive use of glaucoma drugs were collected and analyzed.
All data were analyzed with the SPSS software (version 18.0; SPSS Inc., Chicago, IL, USA). Descriptive statistics, including mean and SD, were calculated for all patient characteristics. One-way ANOVA was used to compare continuous variables, and Pearson’s chi-squared test was used to compare categorical variables. P-values of <0.05 were regarded as statistically significant.
Results
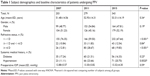
A total of 203 , 279, and 343 patients underwent PPV at the Eye, Ear, Nose, and Throat Hospital of Fudan University in November 2007, November 2001, and November 2015, respectively. The demographic characteristics of the three groups of patients are summarized in Table 1. The patients’ age, preoperative IOPs, sex ratios, and the proportions of patients with diabetes did not differ significantly among the groups. The proportions of patients with high myopia (≥ −6 spherical diopters) in 2007, 2011, and 2015 were 12.5%, 28.6%, and 19.5%, respectively, which differed significantly across the three groups (P<0.001, Pearson’s chi-squared test). The proportion of patients with high myopia was significantly higher in 2011 than in 2007 (P<0.001, Pearson’s chi-squared test), but was significantly lower in 2015 than in 2011 (P=0.01, Pearson’s chi-squared test). The proportions of patients with hypertension in 2007, 2011, and 2015 were 11.1%, 23.6%, and 20.3%, which differed significantly across the three groups (P=0.002, Pearson’s chi-squared test). The proportions of patients with hypertension were significantly higher in 2011 and 2015 than in 2007 (P=0.001 and P=0.005, respectively, Pearson’s chi-squared test).
Surgery-related information is shown in Table 2. The proportions of each of the five diagnoses were compared across the three groups. The proportions of RRD, PDR, vitreous hemorrhage without PDR, and other disorders did not differ significantly in the three groups (P>0.05, Pearson’s chi-squared test), but the proportion of macular disease was significantly higher in 2015 than in 2007 or 2011 (P<0.001, Pearson’s chi-squared test). This suggests that the number of patients with macular disease requiring PPV increased during the period of the study.
The vitrectomy system used changed greatly between 2007 and 2015. In 2007 and 2011, all PPVs were conducted with the 20G vitrectomy system. However, in 2015, the proportions of patients treated with the 20G, 23G, and 25G PPV systems were 15.45%, 83.09%, and 1.46%, respectively (P<0.001, Pearson’s chi-squared test).
The combined surgical procedures with PPV are listed in Table 2. There was almost no difference in the rate of cataract extraction without IOL implantation among the three groups (P=0.93). However, the proportions of patients who underwent PPV combined with cataract extraction and IOL implantation differed significantly across the groups, and this proportion increased significantly from 12.81% in 2007 to 25.95% in 2015 (P<0.001, Pearson’s chi-squared test). Therefore, the proportion of patients treated with PPV combined with cataract extraction and IOL implantation increased with time.
In terms of the intraocular tamponade used, the proportions of patients given filtered air were 7.7%, 4.3%, and 15.8% in 2007, 2011, and 2015, respectively, and differed significantly among the three groups (P<0.001, Pearson’s chi-squared test). The use of an expanding gas, such as SF6 or C3F8, also differed significantly in the three groups (P=0.044, Pearson’s chi-squared test). The rates of use of other tamponades, including BSS and silicone oil, did not differ significantly across the three groups.
The sex ratios among patients with different diagnoses in the total population are shown in Table 3. The female-to-male ratio in patients with RRD was 0.82, whereas the ratios in patients with MH, ERM, and MS were 2.00, 1.59, and 2.25, respectively. The ratio among patients with vitreous hemorrhage without PDR was 1.02, and the ratio for patients with PDR was 1.02.
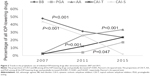
The preventive use of IOP-lowering drugs is shown in Table 4. The proportions of patients administered any prophylactic IOP-lowering drug were 28.08%, 38.35%, and 12.83% in 2007, 2011, and 2015, respectively, which differed significantly in the three groups (P<0.001, Pearson’s chi-squared test) (Figure 1). The proportion of patients given preventive drugs was significantly higher in 2011 than in 2007 (P=0.019, Pearson’s chi-squared test), but was lower in 2015 than in 2011 (P<0.001, Pearson’s chi-squared test).
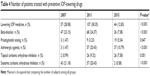  | Table 4 Number of patients treated with preventive IOP-lowering drugs |
The types of drugs used prophylactically changed greatly during the three groups investigated. As shown in Table 4 and Figure 2, the proportions of patients treated with BBs and CAI-Ss in 2007 were 22.6% and 20.7%, respectively. Together, BBs and CAI-Ss accounted for 91.93% of all IOP-lowering drugs administered in 2007. However, the proportions of patients treated with these two drugs decreased to 7.4% and 0.6%, respectively, in 2015, and together they accounted for only 25.48% of all IOP-lowering drugs administered. Significant differences were detected in the use of BBs and CAI-Ss in the three groups (P<0.001, Pearson’s chi-squared test). However, the proportions of patients treated prophylactically with AAs and CAI-Ts increased from 1.4% and 1.0%, respectively, in 2007 to 10.6% and 7.4%, respectively, in 2015 (P<0.001, Pearson’s chi-squared test). The proportion of patients treated with PGA increased significantly from 1.4% in 2007 to 5.4% in 2015 (P=0.047, Pearson’s chi-squared test).
Discussion
This retrospective repeated cross-sectional study traced the trends in the use of vitrectomy instruments and procedures, patient characteristics, and the preventive use of IOP-lowering drugs at our hospital from 2007 to 2015. Our data show that the 23G system, rather than the 20G system, had become the mainstream vitrectomy system by 2015. The proportion of patients with macular disease requiring PPV increased gradually. The proportions of patients undergoing PPV combined with lens extraction and IOL implantation increased continuously in 2015. The percentage of patients treated prophylactically with IOP-lowering drugs declined from 28.08% in 2007 and 38.35% in 2011 to 12.83% in 2015. The use of BBs and CAI-Ss decreased gradually between 2007 and 2015, whereas the preventive use of CAI-Ts, AAs, and PGA gradually increased over the same period.
In recent years, with the development of more sophisticated instruments, PPV has gradually become less invasive and more effective in treating various retinal disorders.1–3 As demonstrated in this study, the most frequently used vitrectomy system changed from the 20G system to the 23G system by 2015.
The main indication for PPV was RRD from 2007 to 2015, and accounted for 49.27%–53.20% of all patients, which is consistent with the constituent ratios of RRD in all PPV indications reported by other Chinese and UK studies.10–13 In a Chinese study, RRD patients accounted for about 40% of the PPV patients.11 In two UK studies, RRD patients accounted for 48.5%–54.83%.12,13
The rate of macular disease changed greatly over these 8 years, increasing significantly from 9.36% in 2007 to 21.87% in 2015. A Singaporean study showed that Chinese ethnicity entails a higher risk of ERM than Malay or Indian ethnicity.14 Another study in the United States showed that Asian-American enrollees had a 177% increased risk of developing MH than the white participants.11 Therefore, the Chinese population has a greater risk of both ERM and MH. Older age is another important risk factor for ERM and MH.14–19 China is one of the most rapidly aging societies in the world, and the prevalence rate of ERM is estimated to be 7.3%–11.43%.18,19 Moreover, with the adoption of the 23G system (a more refined vitrectomy system), and more sophisticated OCT instruments and staining techniques,4 the prognosis for macular diseases treated with PPV has improved in recent years. Therefore, more patients with ERM and MH prefer PPV than conservative treatment, which is another reason for the increase in the rate of macular diseases treated with PPV. Our data for 2015 show that the rates of MH and ERM were 10.2% and 9.33%, respectively, which are very close to those reported in 2013 in the 8-year United Kingdom National Ophthalmology Database Study, which were 9.8% and 9.6%, respectively.13 This suggests that our instrumentation, technique, and indications for PPV have improved greatly in recent years and are similar to the levels in developed countries. However, in another study at a teaching hospital in a medium-sized city in China, macular disease was not considered an indication for PPV until 2014.11 Therefore, the PPV techniques used and the indications applied differ greatly in different hospitals and cities in China.
Being female is a reported risk factor for ERM and MH.15,19 In this study, the OR of female sex for ERM was 1.59, which is consistent with that reported in another Chinese study (OR 1.67).19 The female-to-male ratio was also high in patients with MH or MS in this study, which is consistent with the results of other research.15
The rate of PPV combined with lens extraction and IOL implantation increased from 12.81% in 2007 to 25.95% in 2015, which differ significantly. Moreover, the proportion of patients receiving filtered air as a tamponade increased significantly in this 8-year period. As reported previously, PPV for idiopathic ERM combined with lens surgery greatly increases the patient’s visual quality.20 In this study, PPV was usually performed for the treatment of macular diseases with a combination of lens exaction and IOL implantation, with filtered air used as the tamponade. The increased rate of PPV combined with lens extraction and IOL implantation and the use of filtered air as tamponade resulted from the increase in the proportion of macular diseases among patients treated with PPV.
Ocular hypertension is a common complication of PPV. Several studies have shown that the incidence of ocular hypertension in vitrectomized eyes varies from 18% to 56%.21–24 In our previous study, we reported that about 20% of the patients who underwent PPV at our hospital in November 2011 had no history of glaucoma or ocular hypertension, but suffered ocular hypertension during the first postoperative year.6 Most ocular hypertension occurs in the first month after PPV.6 Risk factors for ocular hypertension after PPV include a history of glaucoma, a history of diabetes mellitus, scleral buckling procedures, lensectomy, and the use of silicone oil or expanding gas.6
There is no guideline for the management of ocular hypertension after PPV. To reduce the incidence of early-onset ocular hypertension and the damage it causes to the optic nerve and retina, some surgeons prophylactically administer IOP-lowering drugs on postoperative day 1 after PPV to patients with a high risk of ocular hypertension.7–9 This study showed that the preventive use of glaucoma drugs has decreased significantly in recent years. As previous studies have shown, the 23G PPV system is less invasive than 20G PPV, and the incidence of early-onset ocular hypertension in patients treated with 23G PPV is lower than that in patients treated with 20G PPV.2,3 Furthermore, macular disease presents a lower risk of elevated IOP after PPV than other vitreoretinal disorders.25,26 Therefore, the reduced use of IOP-lowering drugs might be the result of more refined PPV instruments and procedures and the increase in the proportion of patients with macular diseases. Another reason is that increasing numbers of surgeons prefer to control IOP after it has occurred rather than preventing it with antiglaucoma drugs, because these drugs can have adverse effects. Because there are no data on the incidence of ocular hypertension in November 2007 or November 2015, the relationship between the prophylactic use of IOP-lowering drugs and the incidence of ocular hypertension was difficult to assess in this study. However, this question requires investigation in future studies.
All types of IOP-lowering medications are recommended to treat early-onset ocular hypertension, except PGAs. This study showed that the prophylactic use of IOP-lowering drugs changed markedly in the 8 years of the study. The most obvious change was the reduction in the prophylactic use of CAI-Ss, which decreased from 21.18% to 0.58%. In recent years, there have been several case reports of severe complications associated with acetazolamide and methazolamide, including Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and death in some patients.27–29 The case reports of methazolamide-induced SJS and TEN were initially limited to patients of Japanese and Korean descent.27–29 However, in 2015, Chinese researchers reported cases of methazolamide-induced SJS/TEN in China and found that they were strongly associated with HLA-B*59:01.30,31 Therefore, systemic anhydrase inhibitors can cause severe complications, especially in the eastern-Asian population, and when this came to the notice of doctors, they were gradually abandoned as antiglaucoma medications in China. In this study, the prophylactic use of CAI-Ss decreased greatly. However, there have been no similar case reports of complications caused by CAI-Ts. Consequently, the preventive use of CAI-Ts increased significantly from 0.99% in 2007 to 7.58% in 2015.
PGA entails a potential risk of increasing inflammation and the development of cystoid macular edema.32–34 However, PGA is still effective and safe for the treatment of elevated IOP in patients with uveitis,35,36 but whether it can be used to control IOP in inflamed eyes is still contentious.37–39 The preventive use of PGA in patients who had undergone PPV increased significantly in the 8 years of this study. This suggests that although PGA is used less frequently than other topical IOP-lowering drugs, increasing numbers of surgeons consider that PGA can be used to treat ocular hypertension after PPV.
Conclusion
The 23G vitrectomy system had become the mainstream PPV system by 2015. The proportion of patients with macular diseases undergoing PPV has tended to increase in China in recent years. The prophylactic use of antiglaucoma drugs after PPV has decreased significantly. However, there is no guideline for the preventive use of glaucoma drugs, and further clinical research is required to supply such evidence in the future.
Acknowledgment
This study was supported by the Chinese National Natural Science Foundation (NSFC81100667), the Chinese International Science and Technology Cooperation Program (no 2015DFA31340), and the Science and Technology Commission of Shanghai Municipality (16411953700 and 16401932500).
Disclosure
The authors report no conflicts of interest in this work.
References
Taleb EA, Nagpal MP, Mehrotra NS, et al. Comparison of clinical outcome between 23-G and 25-G vitrectomy in diabetic patients. Oman J Ophthalmol. 2017;10(3):213–219. | ||
Kim IG, Lee SJ, Park JM. Comparison of the 20-gauge conventional vitrectomy technique with the 23-gauge releasable suture vitrectomy technique. Korean J Ophthalmol. 2013;27(1):12–18. | ||
Ahn SJ, Woo SJ, Ahn J, Park KH. Comparison of postoperative intraocular pressure changes between 23-gauge transconjunctival sutureless vitrectomy and conventional 20-gauge vitrectomy. Eye. 2012;26(6):796–802. | ||
Farah ME, Maia M, Penha FM, Rodrigues EB. The Use of Vital Dyes during Vitreoretinal Surgery – Chromovitrectomy. Dev Ophthalmol. 2016;55:365–375. | ||
Miele A, Govetto A, Fumagalli C, et al. Ocular hypertension and glaucoma following vitrectomy. A systematic review. Retina. 2017;0:1–8. | ||
Fang Y, Long Q, Wang X, Jiang R, Sun X. Intraocular pressure 1 year after vitrectomy in eyes without a history of glaucoma or ocular hypertension. Clin Ophthalmol. 2017;11:2091–2097. | ||
Mittra RA, Pollack JS, Dev S, et al. The use of topical aqueous suppressants in the prevention of postoperative intraocular pressure elevation after pars plana vitrectomy with long-acting gas tamponade. Ophthalmology. 2000;107(3):588–592. | ||
Sciscio A, Casswell AG. Effectiveness of apraclonidine 1% in preventing intraocular pressure rise following macular hole surgery. Br J Ophthalmol. 2001;85(2):164–168. | ||
Benz MS, Escalona-Benz EM, Murray TG, et al. Immediate postoperative use of a topical agent to prevent intraocular pressure elevation after pars plana vitrectomy with gas tamponade. Arch Ophthalmol. 2004;122(5):705–709. | ||
Zhou S, Wu C, Lang P, Huang B. Epidemiological survey of ophthalmic inpatient age 50 years or more. Journal of Practical Preventing Blind. 2007;3:33–35 (in Chinese). | ||
Lin H. The constitution of hospitalized patients in Department of Ophthalmology in Jiaxing Chinese Medical Hospital from 2011 to 2014. Chinese Journal of Hospital Statistics. 2017;3:231–233 (in Chinese). | ||
Gupta B, Neffendorf JE, Wong R, Laidlaw DAH, Williamson TH. Ethnic variation in vitreoretinal surgery: differences in clinical presentation and outcome. Eur J Ophthalmol. 2017;27(3):367–371. | ||
Jackson TL, Donachie PH, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database Study of Vitreoretinal Surgery: report 1; case mix, complications, and cataract. Eye. 2013;27(5):644–651. | ||
Cheung N, Tan SP, Lee SY, et al. Prevalence and risk factors for epiretinal membrane: the Singapore Epidemiology of Eye Disease study. Br J Ophthalmol. 2017;101(3):371–376. | ||
Ali FS, Stein JD, Blachley TS, Ackley S, Stewart JM. Incidence of and Risk Factors for Developing Idiopathic Macular Hole Among a Diverse Group of Patients Throughout the United States. JAMA Ophthalmol. 2017;135(4):299–305. | ||
Meuer SM, Myers CE, Klein BE, et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-domain optical coherence tomography: the beaver dam eye study. Ophthalmology. 2015;122(4):787–795. | ||
Kim JM, Lee H, Shin JP, Ahn J, Yoo JM, Song SJ. Epiretinal Membrane: Prevalence and Risk Factors from the Korea National Health and Nutrition Examination Survey, 2008 through 2012. Korean J Ophthalmol. 2017;31(6):514–523. | ||
Liu L, Yue S, Wu J, et al. The Prevalence and Distribution of Vitreoretinal Interface Abnormalities among Urban Community Population in China. J Ophthalmol. 2015;2015:742686–6. | ||
Ye H, Zhang Q, Liu X, et al. Prevalence and associations of epiretinal membrane in an elderly urban Chinese population in China: the Jiangning Eye Study. Br J Ophthalmol. 2015;99(12):1594–1597. | ||
Lee PY, Cheng KC, Wu WC. Anatomic and functional outcome after surgical removal of idiopathic macular epiretinal membrane. Kaohsiung J Med Sci. 2011;27(7):268–275. | ||
Faulborn J, Conway BP, Machemer R. Surgical complications of pars plana vitreous surgery. Ophthalmology. 1978;85(2):116–125. | ||
Parke DW 3rd, Sisk RA, Houston SK, Murray TG. Ocular hypertension after intravitreal triamcinolone with vitrectomy and phacoemulsification. Clin Ophthalmol. 2012;6:925–931. | ||
Antoun J, Azar G, Jabbour E, et al. Vitreoretinal surgery with silicone oil tamponade in primary uncomplicated rhegmatogenous retinal detachment: Clinical Outcomes and Complications. Retina. 2016;36(10):1906–1912. | ||
Jonas JB, Knorr HL, Rank RM, Budde WM. Intraocular pressure and silicone oil endotamponade. J Glaucoma. 2001;10(2):102–108. | ||
Hasegawa Y, Okamoto F, Sugiura Y, Okamoto Y, Hiraoka T, Oshika T. Intraocular pressure elevation after vitrectomy for various vitreoretinal disorders. Eur J Ophthalmol. 2014;24(2):235–241. | ||
Yamamoto K, Iwase T, Terasaki H. Long-term changes in intraocular pressure after vitrectomy for rhegmatogenous retinal detachment, epi-retinal membrane, or macular hole. PLoS One. 2016;11(11):e0167303. | ||
Her Y, Kil MS, Park JH, Kim CW, Kim SS. Stevens-Johnson syndrome induced by acetazolamide. J Dermatol. 2011;38(3):272–275. | ||
Ogasawara K, Tomitsuka N, Kobayashi M, et al. Stevens-Johnson syndrome associated with intravenous acetazolamide administration for evaluation of cerebrovascular reactivity. Case report. Neurol Med Chir. 2006;46(3):161–163. | ||
Flach AJ, Smith RE, Fraunfelder FT. Stevens-Johnson syndrome associated with methazolamide treatment reported in two Japanese-American women. Ophthalmology. 1995;102(11):1677–1680. | ||
Shu C, Shu D, Tie D, et al. Toxic epidermal necrolysis induced by methazolamide in a Chinese-Korean man carrying HLA-B*59:01. Int J Dermatol. 2015;54(11):1242–1245. | ||
Yang F, Yang Y, Zhu Q, et al. Research on Susceptible Genes and Immunological Pathogenesis of Cutaneous Adverse Drug Reactions in Chinese Hans. J Investig Dermatol Symp Proc. 2015;17(1):29–31. | ||
Moroi SE, Gottfredsdottir MS, Schteingart MT, et al. Cystoid macular edema associated with latanoprost therapy in a case series of patients with glaucoma and ocular hypertension. Ophthalmology. 1999;106(5):1024–1029. | ||
Ayyala RS, Cruz DA, Margo CE, et al. Cystoid macular edema associated with latanoprost in aphakic and pseudophakic eyes. Am J Ophthalmol. 1998;126(4):602–604. | ||
Wand M, Gaudio AR, Shields MB. Latanoprost and cystoid macular edema in high-risk aphakic or pseudophakic eyes. J Cataract Refract Surg. 2001;27(9):1397–1401. | ||
Chang JH, Mccluskey P, Missotten T, Ferrante P, Jalaludin B, Lightman S. Use of ocular hypotensive prostaglandin analogues in patients with uveitis: does their use increase anterior uveitis and cystoid macular oedema? Br J Ophthalmol. 2008;92(7):916–921. | ||
Moghimi S, Zandian M, Latifi G, et al. Topical latanoprost does not cause macular thickening after uncomplicated cataract surgery. J Ophthalmic Vis Res. 2012;7(4):289–294. | ||
Miyake K, Ibaraki N. Prostaglandins and cystoid macular edema. Surv Ophthalmol. 2002;47(Suppl 1):S203–S218. | ||
Alm A, Grierson I, Shields MB. Side effects associated with prostaglandin analog therapy. Surv Ophthalmol. 2008;53(Suppl 1):S93–S105. | ||
Horsley MB, Chen TC. The use of prostaglandin analogs in the uveitic patient. Semin Ophthalmol. 2011;26(4–5):285–289. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.