Back to Journals » Open Access Surgery » Volume 13
Treatment of Isolated Complete Atrioventricular Septal Defect: The Hue Central Hospital Experience
Authors Xuan NT , Hung NX , An TH, Phuoc ND , Son NH , Hiep PN
Received 7 April 2020
Accepted for publication 13 May 2020
Published 2 June 2020 Volume 2020:13 Pages 39—46
DOI https://doi.org/10.2147/OAS.S255267
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Luigi Bonavina
Nguyen Thanh Xuan,1 Nguyen Xuan Hung,2 Tran Hoai An,2 Nguyen Dang Phuoc,2 Nguyen Huu Son,3 Pham Nhu Hiep1
1Department of Abdominal Emergency and Pediatric Surgery, Hue Central Hospital, Hue City, Vietnam; 2Department of Cardiovascular Surgery, Cardiovascular Center, Hue Central Hospital, Hue City, Vietnam; 3Department of Pediatric Neurology, Pediatric Center, Hue Central Hospital, Hue City, Vietnam
Correspondence: Nguyen Thanh Xuan
Department of Abdominal Emergency and Pediatric Surgery, Hue Central Hospital, 16 Le Loi Street, Hue City 530000, Vietnam
Tel +84945313999
Email [email protected]
Background: Complete atrioventricular septal defect is a complex cardiac malformation characterized by an ostium primum atrial septal defect, a common atrioventricular valve, and a variable deficiency of the ventricular septum inflow. The left AV valve and right AV valve have no clear division. The treatment of complete atrioventricular septal defects has evolved in recent decades, but it remains challenging. This retrospective study evaluated early and late outcomes in patients undergoing surgery at a single heart center.
Patients and Methods: We retrospectively evaluated outcomes in 52 complete atrioventricular septal defect patients undergoing definitive repair from January 2016 to January 2018. All patients were repaired with either the classic one-patch technique or the two-patch technique.
Results: The mean age at operation was 4.12 ± 0.26 months (2 months– 3 years). Forty cases (76.9%) included in the study have Down’s syndrome. After the operation, the atrioventricular valve showed marked improvement, and pulmonary artery pressure tended to decrease when compared with preoperative levels. Arrhythmias in two cases with 3rd-degree AV block required permanent pacing (3.8%). In-hospital mortality was observed in 1/52 (1.9%) of patients. The 3-year overall survival rate after repair was 98.1%. No significant difference was found between the two groups.
Conclusion: The surgical repair of complete atrioventricular septal defects demonstrated excellent results at a very early age and even in the case of Down’s syndrome.
Keywords: complete atrioventricular septal defect, repair, outcome
Introduction
Complete atrioventricular septal defect (AVSD) is a complicated congenital heart defect with an ostium primum type of atrial septal defect, a large ventricular septal defect, and severe atrioventricular valve lesions. Surgical repair for atrioventricular septal defects brings significant risks. These are one of the biggest challenges for cardiovascular surgeons and anesthetists, particularly in developing countries.1 Pediatric patients with complete AVSD have substantial morbidity as well as mortality due to postoperative atrioventricular valve regurgitation, remaining intracardiac shunts, pulmonary hypertension, and many severity cardiac arrhythmias.
Currently, three different surgical techniques have been applied, including the classical one-patch technique, two-patch technique, and the modified single-patch technique (or Australian technique), which have its advantages and disadvantages. Using this or the other techniques have usually been a surgeon’s choice based on their experience. Nevertheless, the shift to younger age for surgery of complete AVSD, even in symptomatic neonates2,3 has increased concerns with respect to the dividing and re-attachment of the fragile and delicate valve tissue of newborn babies and young infants in the one-patch technique.4 Excellent outcomes with the early surgical repair of complete AVSD have been reported with the two-patch technique.5–7
In Hue Central Hospital, we have performed either one-patch or two-patch surgical technique recently and had some valuable experience. To explore the early and late outcomes of patients with complete AVSD undergoing surgical repair, we conducted this study aims to compare the preoperative and postoperative conditions of valve regurgitation and pulmonary hypertension; evaluate potential complications and mid-term survival rate.
Patients and Methods
Patients
Fifty-two patients undergoing the surgical repair of complete AVSD were selected for a retrospective study. Complete AVSD patients with a single ventricle were excluded from the study. They were enrolled in the study from January 2016 to January 2018 after the ethical approval of the Research Ethics Committee of Hue Central Hospital under the reference number of 01012018/HCH. Patient consent to review their medical records was also obtained.
Surgical Technique
Twenty patients underwent surgical repair of complete AVSD with the classic one-patch technique (as shown in Figure 1), and thirty-two patients were repaired using the two-patch technique (as shown in Figure 2).
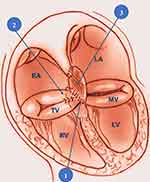 |
Figure 1 One-patch technique to repair of complete AVSD: (1) Close the VSD directly; (2) close cleft of the left AV valve leaflet; (3) close the ASD with a pericardial membrane. |
 |
Figure 2 Two-patch technique: (1) Close the cleft of the left AV valve leaflet; (2) close VSD with a pericardial membrane; (3) close the ASD with a pericardial membrane. |
One-patch was performed by closing the ventricular septal defect (VSD) directly with Prolene 6.0 and dividing the left AV and the right AV. We closed the cleft of the left AV valve leaflet, then closed the atrial septal defect (ASD) with a pericardial membrane.8
With the two-patch technique, we firstly closed the cleft of the left AV valve leaflet. The sutures were performed through the superior patch dividing the left AV and the right AV. These sutures were passed through ASD to close the ASD by pericardial membrane.9
Data Analysis
Patients were divided into two groups according to the surgical method: the one-patch group and the two-patch group. All data were collected from the medical records of the hospital during the patients hospitalized and a follow-up visit to our outpatient clinic. Clinical examination and echocardiographic exploration were regularly carried out at below time: pre-operation, post-operation, 3 months, 6 months, 12 months, 18 months, and 3 years after discharge.
Statistical analysis was undertaken using the SPSS statistical program version 22 (IBM Corp., NY, USA). All data were expressed as percentages, mean, standard deviation, or median values as per data type (qualitative or quantitative). Categoric variables between the two groups were compared using the χ2 test or the Fisher exact, where appropriate. Continuous variables were compared using the Mann Whitney U-test for independent samples. The survival rate after repair was calculated using the Kaplan–Meier method.
Results
The characteristics of 52 patients who underwent the definitive repair of complete AVSD are presented in Table 1. The mean of age and weight was 4.1 ± 0.3 months (range from 2 months to 3 years) and 6.1 ± 0.8 kg (range from 5.7 to 9.3 kg), respectively. Most patients (80.8%) were under 6 months of age. Down’s syndrome was seen in 40 (76.9%) patients. The degree of atrioventricular valve regurgitation before surgery was mostly moderate to severe, from 2/4 or more. Most patients had pulmonary hypertension (96.2%), and up to 35 pediatric patients had severe pulmonary hypertension >60 mmHg (67.3%). No significant difference was found between the two groups.
 |
Table 1 Patient’s Preoperative Characteristics |
The operative data and outcomes are shown in Table 2. After the surgery, the condition of valve regurgitation was significantly improved, with mild valve regurgitation for the left AV valve (92.3%) and for the right AV valve (96.2%). Patients after surgery no longer had pulmonary hypertension (92.3%). Common complications in the surgical treatment of complete AVSD are low cardiac output syndrome (7.7%) and acute kidney failure (11.5%) requiring peritoneal dialysis. In addition, the most unexpected complication was 3rd-degree AV block, which was seen in 2 (3.8%) patients. One patient (1.9%) died after the operation. There was no significant difference in outcome data between the two groups.
 |
Table 2 Operative Data and Postoperative Outcomes |
The patients were re-examined and showed good surgical results (Table 3). One patient with moderate left AV valve regurgitation needed to be closely monitored. Weight gain was monthly obtained in almost patients after repair. Respiratory infections as late complications occurred at a low rate. The 3-year overall survival (OS) rate after repair was 98.1% (Figure 3).
 |
Table 3 Re-Examination After 3, 6, 12 and 18 Months |
 |
Figure 3 Overall survival curve of the patients within 3-year follow-up. |
Discussion
The diagnosis of AVSD is usually based on echocardiography results. Echocardiography is particularly effective for describing the anatomy of AVSD and possible comorbidities. Understanding the anatomy and morphology of AVSD and advances in surgical technology have significantly reduced postoperative mortality. The timing of surgical intervention in patients is best at 3 to 6 months of age.10 Surgical delays lead to an increase in respiratory illnesses and pulmonary vascular disease.11 The trend towards early surgery reduces pulmonary hypertension, which is one of the main causes of morbidity.12,13
Our data showed that the mean of age and weight at operation was 4.1 ± 0.3 months (range from 2 months to 3 years) and 6.1 ± 0.8 kg (range from 5.7 to 9.3 kg), respectively, which was similar to those in the previous reports such as Bakhtiary with the median age was 3.8 months (range from 15 days to 4.7 years), and the median weight was 5.0 kg (range from 3.0 to 19 kg).14 St Louis with the median age and weight at surgery was 4.6 months and 5.0 kg, respectively.15
Earlier surgical repair of complete AVSD might be theoretically beneficial because annular dilation or degenerative changes, or both, of the common atrioventricular valve, might proceed as the children ages. Some reports could prove that annular dilatation is significant to develop left atrioventricular valve regurgitation and raises the risk for re-operation in older children.10,16
In addition, the early surgical treatment also helps to maintain the function of the atrioventricular valves, and the repair of atrioventricular valves at this stage is more convenient due to the absence of annulus dilation.17
The two-patch technique was performed in 32 (61.5%) of our patients. The kind of surgical technique did not show any significant differences in terms of postoperative valve regurgitation, pulmonary hypertension, potential complication, overall survival rate. Pan studied on 98 patients with complete AVSD, in which 46 infants underwent the modified single-patch technique, and 59 infants underwent the two-patch technique.7 No significant difference was seen between the two surgical techniques in terms of postoperative atrioventricular valve regurgitation, residual ventricular septal defect, left ventricular outflow tract obstruction, and mortality except for a longer cross-clamp time for the two-patch group. Pan also showed that two patients developed heart block that needed a pacemaker insertion, but there was no significant difference between the two groups. Two of our patients developed 3rd-degree AV block that required a pacemaker, which is similar to the occurrence in other centers throughout the world.
In our series, both the early outcomes and mid-term survival were very acceptable after the treatment of complete AVSD. The rate of complication was low, and all of them then have been well managed by multi-modalities, and no case required re-operation. In the study of Bakhtiary, there was no perioperative, early or late mortality. However, left atrioventricular valve regurgitation continued a matter during further follow-up. Reoperations for atrioventricular valve regurgitation were ordered in 6% of their patients.
Postoperative follow-up focuses on optimizing cardiac output and avoiding pulmonary hypertension. Using nitric oxide in all patients with a pulmonary artery pressure greater than 50% of the system pressure at the end of surgery is suggested.18 Postoperative follow-up should pay attention to hypoxia, hypertension, pain, and hypothermia as factors that cause lung contractions.
The surgical treatment of complete AVSD should focus on the lack of valve tissue leading to limited atrioventricular valve mobility.19 In our study, postoperative atrioventricular valve regurgitation significantly improved, giving positive results. In other studies, the two-patch technique maintained the valve structure, reduced the lack of valve tissue, and reduced the progression of atrioventricular valve regurgitation.20,21
One patient (1.9%) in-hospital died. Premature infant patients had a shorter postoperative time as well as a better prognosis. This finding is reasonable because older patients often have severe pulmonary hypertension and a large degree of regurgitation from which it is difficult to recover.11 The overall in-hospital mortality according to St Luis was 3.0%,15 which was higher than that in our study.
In our study, the degree of postoperative valve regurgitation was followed for up to 18 months, and the outcomes were improved greatly. The three-year OS rate among patients after repair was very high (98.1%). Late complications such as respiratory infections were found at a low rate, and most of them were well responded with appropriate therapeutics. The mortality was higher, and the OS rate was lower in the past (1974–2000) according to Ginde,22 which the overall perioperative mortality was 10.1%, and the overall estimated survival for the entire cohort was 85% at 10 years.
Our study has several limitations. It is a retrospective study at a single heart center, with mid-term follow-up among patients. All patients underwent surgical repair at Cardiovascular Center of Hue Central Hospital, mostly with a small team of cardiovascular surgeons, and the outcome data might not estimate for alterations in repair techniques and postoperative treatment at other centers.
Despite the limitations, our experience with both one-patch and two-patch technique evidenced the relatively short clamping aorta and extracorporeal circulation times, which was consistent with the literature. Further prospective studies are strongly recommended in the field with larger sample size and long-term follow-up to ascertain conclusions drawn from this study.
Conclusions
Our results highlight that all types of complete AVSD can be well repaired at a very early age, and even in case of Down’s syndrome. Both one-patch and two-patch techniques are safe and reproducible surgical methods that can achieve low mortality and good mid-term outcomes. Therefore, the surgery should be performed as soon as possible before pulmonary hypertension and other preoperative complications occurring.
Abbreviations
AVSD, atrioventricular septal defect; AV, atrioventricular; ASD, atrial septal defect; VSD, ventricular septal defect; ICU, intensive care unit; OS, overall survival.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Backer CL, Stewart RD, Bailliard F, Kelle AM, Webb CL, Mavroudis C. Complete atrioventricular canal: comparison of modified single-patch technique with two-patch technique. Ann Thorac Surg. 2007;84(6):2038–2046. doi:10.1016/j.athoracsur.2007.04.129
2. Ellis FH
3. Reddy VM, McElhinney DB, Sagrado T, Parry AJ, Teitel DF, Hanley FL. Results of 102 cases of complete repair of congenital heart defects in patients weighing 700 to 2500 grams. J Thorac Cardiovasc Surg. 1999;117(2):324–331. doi:10.1016/S0022-5223(99)70430-7
4. Fortuna RS, Ashburn DA, Carias De Oliveira N, et al. Atrioventricular septal defects: effect of bridging leaflet division on early valve function. Ann Thorac Surg. 2004;77(3):
5. Al-Hay AA, MacNeill SJ, Yacoub M, Shore DF, Shinebourne EA. Complete atrioventricular septal defect, down syndrome, and surgical outcome: risk factors. Ann Thorac Surg. 2003;75(2):412–421. doi:10.1016/S0003-4975(02)04026-2
6. Li D, Fan Q, Iwase T, Hirata Y, An Q. Modified single-patch technique versus two-patch technique for the repair of complete atrioventricular septal defect: a meta-analysis. Pediatr Cardiol. 2017;38(7):1456–1464. doi:10.1007/s00246-017-1684-8
7. Pan G, Song L, Zhou X, Zhao J. Complete atrioventricular septal defect: comparison of modified single-patch technique with two-patch technique in infants. J Card Surg. 2014;29(2):251–255. doi:10.1111/jocs.12295
8. Crawford FA Atrioventricular canal: single-patch technique.
9. Mavroudis C, Backer CL. The two-patch technique for complete atrioventricular canal. Semin Thorac Cardiovasc Surg. 1997;9(1):35–43.
10. Suzuki T, Bove EL, Devaney EJ, et al. Results of definitive repair of complete atrioventricular septal defect in neonates and infants. Ann Thorac Surg. 2008;86(2):596–602. doi:10.1016/j.athoracsur.2008.02.032
11. Prifti E, Bonacchi M, Bernabei M, et al. Repair of complete atrioventricular septal defects in patients weighing less than 5 kg. Ann Thorac Surg. 2004;77(5):1717–1726. doi:10.1016/j.athoracsur.2003.06.032
12. Alexi-Meskishvili V, Ishino K, Dahnert I, et al. Correction of complete atrioventricular septal defects with the double-patch technique and cleft closure. Ann Thorac Surg. 1996;62(2):
13. Wetter J, Sinzobahamvya N, Blaschczok C, et al. Closure of the zone of apposition at correction of complete atrioventricular septal defect improves outcome. Eur J Cardiothorac Surg. 2000;17(2):146–153. doi:10.1016/S1010-7940(99)00360-7
14. Bakhtiary F, Takacs J, Cho MY, et al. Long-term results after repair of complete atrioventricular septal defect with two-patch technique. Ann Thorac Surg. 2010;89(4):1239–1243. doi:10.1016/j.athoracsur.2009.11.017
15. St Louis JD, Jodhka U, Jacobs JP, et al. Contemporary outcomes of complete atrioventricular septal defect repair: analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. J Thorac Cardiovasc Surg. 2014;148(6):2526–2531. doi:10.1016/j.jtcvs.2014.05.095
16. Dodge-Khatami A, Herger S, Rousson V, et al. Outcomes and reoperations after total correction of complete atrio-ventricular septal defect. Eur J Cardiothorac Surg. 2008;34(4):745–750. doi:10.1016/j.ejcts.2008.06.047
17. Michielon G, Stellin G, Rizzoli G, Casarotto DC. Repair of complete common atrioventricular canal defects in patients younger than four months of age. Circulation. 1997;96(9 Suppl):
18. Machado RF, Londhe Nerkar MV, Dweik RA, et al. Nitric oxide and pulmonary arterial pressures in pulmonary hypertension. Free Radic Biol Med. 2004;37(7):1010–1017. doi:10.1016/j.freeradbiomed.2004.06.039
19. Najm HK, Coles JG, Endo M, et al. Complete atrioventricular septal defects: results of repair, risk factors, and freedom from reoperation. Circulation. 1997;96(9 Suppl):
20. Bogers AJ, Akkersdijk GP, de Jong PL, et al. Results of primary two-patch repair of complete atrioventricular septal defect. Eur J Cardiothorac Surg. 2000;18(4):473–479. doi:10.1016/S1010-7940(00)00536-4
21. Gunther T, Mazzitelli D, Haehnel CJ, Holper K, Sebening F, Meisner H. Long-term results after repair of complete atrioventricular septal defects: analysis of risk factors. Ann Thorac Surg. 1998;65(3):
22. Ginde S, Lam J, Hill GD, et al. Long-term outcomes after surgical repair of complete atrioventricular septal defect. J Thorac Cardiovasc Surg. 2015;150(2):369–374. doi:10.1016/j.jtcvs.2015.05.011
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
