Back to Journals » OncoTargets and Therapy » Volume 11
Tooth loss and risk of colorectal cancer: a dose–response meta-analysis of prospective cohort studies
Authors Ma P, Dai S, Jin C, Yao Y, Zou C
Received 6 September 2017
Accepted for publication 30 January 2018
Published 21 March 2018 Volume 2018:11 Pages 1617—1623
DOI https://doi.org/10.2147/OTT.S151028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Faris Farassati
Peng Ma, Shaojun Dai, Can Jin, Yonggang Yao, Chuanxin Zou
Department of Gastroenterology, The Second Clinical Medical College, Yangtze University, Jingzhou, Hubei Province, People’s Republic of China
Background: Previous studies have indicated that tooth loss is associated with colorectal cancer risk but have presented controversial results.
Methods: We conducted a dose–response meta-analysis in order to investigate the correlation between tooth loss and colorectal cancer risk. Up to August 2017, six eligible studies were included in this meta-analysis.
Results: Our results showed statistically significant association between tooth loss and colorectal cancer (OR =1.08, 95% CI: 1.03–1.15, P<0.001). In addition, we obtained the best fit at an inflection point of every two tooth loss in piecewise regression analysis, and the summary relative risk (RR) of colorectal cancer for an increase of every two tooth loss was 1.06 (95% CI: 1.02–1.11, P<0.001). Furthermore, tooth loss was significantly associated with colorectal cancer risk in Caucasia (RR: 1.18; 95% CI: 1.09–1.28; P<0.001) and Asia (RR: 1.06; 95% CI: 1.02–1.10; P<0.001). Moreover, tooth loss was significantly associated with a higher risk of colon cancer (RR: 1.09; 95% CI: 1.02–1.17; P<0.001) and rectal cancer (RR: 1.08; 95% CI: 1.01–1.17; P<0.001).
Conclusion: Subgroup meta-analyses showed consistency with the primary findings. Considering these promising results, increasing tooth loss may be harmful to our health, and maintenance of our oral health is essential.
Keywords: colorectal cancer, tooth loss, dose–response relationship, meta-analysis
Introduction
Colorectal cancer is the third most common cancer worldwide, and it costs patients, caregivers, and society.1 According to the statistics of the American Cancer Association, colorectal cancer mortality has gradually increased, while the overall cure rate for colorectal cancer has not improved significantly over the past decade.2,3 Every year, as many as 930,000 newly patients are diagnosed with colorectal cancer across the world.2 Due to differences in countries’ geographical environment and living habits, the incidence of colorectal cancer is different in various regions, being the most severe in developing countries such as Africa, Asia, and South America and higher in developed countries than in developing countries. Residents of North America and Europe are the most vulnerable to colorectal cancer, but China has a large population base, making it the country with the highest number of cancer deaths throughout the world.2
There are a few identified risk factors for colorectal cancer, including polyp formation, schistosomiasis, and chronic nonspecific ulcerative colitis. Understanding the impact of environmental factors on colorectal cancer will help to prevent colorectal cancer. Previous studies have showed that oral health is emerging as an independent risk factor for health.
Oral health is an important part of human health. The World Health Organization (WHO) identifies dental health as one of the top 10 criteria for human health. Poor oral health may increase systemic inflammation, resulting in a local overly aggressive immune response and thus could have important implications for cancer development. Periodontal disease and tooth loss are two common oral health problems.4 Colitis, an acute inflammatory state in the colon, is the basis for developing colorectal cancer in majority of the patients, and tooth loss is an independent risk factor for colitis. In addition, tooth loss has been considered to affect quality of life5 and has been known to considerably influence food choice, diet, nutrition intake, and aesthetics.6
Previous studies have reported that tooth loss significantly increases the risk of colorectal cancer. However, the result remains controversial.7–12 Therefore, we have conducted this comprehensive meta-analysis to clarify the correlation between tooth loss and colorectal cancer risk.
Methods
Search strategy
We conducted a systematic literature search of Medline and Embase up to August 2017 to examine the association between tooth loss and colorectal cancer risk. The search terms were “Colorectal Neoplasms” [MeSH] OR “Colorectal Tumor” [MeSH] OR “Colorectal Cancer” [MeSH] OR “Colorectal Carcinoma” [MeSH] OR “Cancer of Breast” [MeSH] AND “Dentition” [MeSH] OR “Tooth Loss” [MeSH] OR “Edentulous” [MeSH] OR “Loss of Tooth” [MeSH].
Data extraction
Investigators independently collected information if the following criteria were met: (1) the outcome was colorectal cancer; (2) risk estimates on the relationship between tooth loss and colorectal cancer risk were provided. According to the Newcastle–Ottawa scale, quality assessment was performed for nonrandomized studies.13
Statistical analysis
Stata software 14.0 (StataCorp LP, College Station, TX, USA) was used in all analyses. Due to different definitions for the cutoff points for categories in the included studies, we calculated the RR estimates by the method recommended by Greenland and Longnecker, as well as Orsini et al.14,15
Results
Literature search results
A total of 2,501 studies from Medline, 3,023 studies from Embase were screened. After removing duplicates, 2,818 studies were identified. Reviewing their titles and abstracts, 2,760 citations were excluded. The remaining 58 citations were assessed in more detail for eligibility by reading the full text. Among them, 18 studies were excluded due to no relevant outcome measure; 23 studies were excluded because they were not human studies; nine studies were excluded as they were reviews; and three studies were excluded due to lack of detailed information. After review of the references of the studies, one article was identified for rejection. Finally, six studies were used for the final data synthesis. The flow chart of the literature search is presented in Figure 1.
  | Figure 1 Flow diagram of the study selection process. |
Study characteristics
The characteristics of the included studies are shown in Tables 1 and 2. Among the selected studies, six studies were eligible, including four cohort studies and two case–control studies; three studies were on Caucasia and three were on Asia; a total of 160,182 participants with 8,309 incident cases were included in this meta-analysis.
  | Table 1 Characteristics of participants in the included studies on tooth loss in relation to risk of colorectal cancer |
Overall meta-analysis
Six eligible studies identified the relationship between tooth loss and colorectal cancer risk. Compared with the reference category, tooth loss is significantly associated with colorectal cancer risk (relative risk [RR]: 1.08; 95% CI: 1.02–1.15; P=0.011) (Figure 2). We found no evidence of between-study heterogeneity (I2=20.5%, P=0.115) and we observed no evidence of publication bias (Egger asymmetry test, P=0.239) (Table S1).
  | Figure 2 Forest plots of colorectal cancer for the highest versus lowest categories of tooth loss. |
Dose–response meta-analyses between tooth loss and colorectal cancer
A dose–response analysis showed that every two incremental increase in tooth loss was associated with a 6% increment in the risk of colorectal cancer; the summary RR of colorectal cancer for an increase of every 10 in tooth loss was 1.06 (95% CI: 1.02–1.11, P<0.001) (Figure 3).
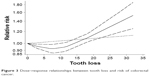  | Figure 3 Dose–response relationships between tooth loss and risk of colorectal cancer. |
Subgroup analyses
Subgroup analysis based on study location found a similar risk increment of colorectal cancer in Asia (OR =1.06; 95% CI: 1.02–1.10; P<0.001) and Caucasian (OR =1.18, 95% CI: 1.09–1.28; P<0.001) (Table 3). In addition, tooth loss is significantly associated with a higher risk of colon cancer (RR: 1.09; 95% CI: 1.02–1.17; P<0.001) and rectal cancer (RR: 1.08; 95% CI: 1.01–1.17; P<0.001) (Table 3). The relationship between tooth loss and colorectal cancer risk was similar in subgroup analyses, which were defined by study design, number of cases or participants, and study quality.
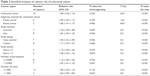  | Table 3 Stratified analyses of relative risk of colorectal cancer |
Publication bias
Publication bias of tooth loss and colorectal cancer was evaluated with both Begg’s and Egger’s tests (Table S1). A funnel plot for the assessment of publication bias is illustrated in Figure S1.
Discussion
Colorectal cancer affects millions of people in developed and developing countries and is now a public health crisis. Despite the decline in the mortality rate in developed countries, colorectal cancer has caused serious social and economic distress on a global scale over the past few decades. In low- and middle-income countries, the incidence of colorectal cancer has risen sharply.2 A link between tooth loss and all-cause mortality has been proposed, and there is evidence of a possible association between tooth loss and atherosclerotic vascular disease. However, studies of tooth loss in colorectal cancer have increased slowly, and the results are inconsistent.
Hiraki et al10 found that increasing teeth loss was associated with risk of head and neck cancer, esophageal cancer, and lung cancer but not colon cancer and ovarian cancer. Michaud et al9 showed that tooth loss was associated with an increased risk of total cancer, lung cancer, kidney cancer, and pancreatic cancer but not colorectal cancer. Momen-Heravi et al8 showed that increasing loss in number of teeth was associated with risk of colorectal cancer. Ren et al7 found no evidence supporting an association between teeth loss and colorectal cancer risk in three cohort studies. Ansai et al11 showed that tooth loss was associated with increased colorectal cancer in the Japanese population. Hujoel et al12 showed that increasing teeth loss was not associated with risk of colorectal cancer. Collectively, these data suggest that teeth loss may play an important role in colorectal cancer risk. However, the result remains controversial. Thus, we conducted this comprehensive meta-analysis to clarify the correlation between tooth loss and colorectal cancer risk.
This meta-analysis was based on six studies up to August 2017. Thus, this meta-analysis provides the most up-to-date epidemiological evidence supporting the proposition that tooth loss is harmful in the context of colorectal cancer.
Several plausible pathways may be responsible for the relationship between tooth loss and cancer. The influence of chronic inflammation on cancer development is one possible pathway.16 Chronic systemic inflammation is linked to periodontal disease,17,18 which is a major cause of tooth loss in adults and can increase the risk of cancer by inhibiting apoptosis and stimulating tumor cell proliferation.19 Secondly, the main cause of teeth loss is dental caries, and carbohydrate intake is the cause for dental caries.20 Carbohydrate intake is associated with increased risk of cancer; therefore, teeth loss indirectly affects the risk of cancer.21,22 Third, the progress of tooth damage destroys normal periodontal tissue, allowing oral microbial accumulation deep into oral tissue, thereby promoting its growth.23 Thus, tooth loss and cancer seem to be closely related.
To our knowledge, this is the first comprehensive study to identify the association between tooth loss and colorectal cancer risk. Some limitations must be considered in the current meta-analysis. First, we did not consider tumor invasion and metastasis in colorectal cancer, which may have resulted in different results in the subgroups. Secondly, though we found no publication bias in this study, there still existed heterogeneity in the association between tooth loss and rectal cancer. Third, we never tried to search for unpublished research, which may lead to the disappearance of related research.
Conclusion
Our dose–response meta-analysis suggests that tooth loss is independently associated with deleterious increments in the risk of colorectal cancer. Our findings underscore the notion that increasing tooth loss may be harmful to our health. In the future, large-scale and population-based association studies must be performed to help identify the putative causal role that tooth loss plays in increasing the incidence of these diseases.
Acknowledgment
This study received no specific external funding.
Disclosure
The authors reports no conflicts of interest in this work.
References
Holleczek B, Rossi S, Domenic A, et al. On-going improvement and persistent differences in the survival for patients with colon and rectum cancer across Europe 1999–2007 – results from the EUROCARE-5 study. Eur J Cancer. 2015;51(15):2158–2168. | ||
Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin. 2016;66(4):271–289. | ||
Zeng H, Zheng R, Guo Y, et al. Cancer survival in China, 2003–2005: a population-based study. Int J Cancer. 2015;136(8):1921–1930. | ||
Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809–1820. | ||
Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126. | ||
Adegboye AR, Twetman S, Christensen LB, Heitmann BL. Intake of dairy calcium and tooth loss among adult Danish men and women. Nutrition. 2012;28(7–8):779–784. | ||
Ren HG, Luu HN, Cai H, et al. Oral health and risk of colorectal cancer: results from three cohort studies and a meta-analysis. Ann Oncol. 2016;27(7):1329–1336. | ||
Momen-Heravi F, Babic A, Tworoger SS, et al. Periodontal disease, tooth loss and colorectal cancer risk: Results from the Nurses’ Health Study. Int J Cancer. 2017;140(3):646–652. | ||
Michaud DS, Liu Y, Meyer M, Giovannucci E, Joshipura K. Periodontal disease, tooth loss, and cancer risk in male health professionals: a prospective cohort study. Lancet Oncol. 2008;9(6):550–558. | ||
Hiraki A, Matsuo K, Suzuki T, Kawase T, Tajima K. Teeth loss and risk of cancer at 14 common sites in Japanese. Cancer Epidemiol Biomarkers Prev. 2008;17(5):1222–1227. | ||
Ansai T, Takata Y, Yoshida A, et al. Association between tooth loss and orodigestive cancer mortality in an 80-year-old community-dwelling Japanese population: a 12-year prospective study. BMC Public Health. 2013;13:814. | ||
Hujoel PP, Drangsholt M, Spiekerman C, Weiss NS. An exploration of the periodontitis-cancer association. Ann Epidemiol. 2003;13(5):312–316. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175(1):66–73. | ||
Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–561. | ||
Moutsopoulos NM, Madianos PN. Low-grade inflammation in chronic infectious diseases: paradigm of periodontal infections. Ann N Y Acad Sci. 2006;1088:251–264. | ||
Kaaks R, Lukanova A. Energy balance and cancer: the role of insulin and insulin-like growth factor-I. Proc Nutr Soc. 2001;60(1):91–106. | ||
Loos BG. Systemic markers of inflammation in periodontitis. J Periodontol. 2005;76(11 suppl):2106–2115. | ||
Chauncey HH, Glass RL, Alman JE. Dental caries. Principal cause of tooth extraction in a sample of US male adults. Caries Res. 1989;23(3):200–205. | ||
Saunders RH Jr, Meyerowitz C. Dental caries in older adults. Dent Clin North Am. 2005;49(2):293–308. | ||
Brand-Miller JC. Postprandial glycemia, glycemic index, and the prevention of type 2 diabetes. Am J Clin Nutr. 2004;80(2):243–244. | ||
Sanders TA. How important is the relative balance of fat and carbohydrate as sources of energy in relation to health? Proc Nutr Soc. 2016;75(2):147–153. | ||
Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Taylor PR, Mark SD. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int J Epidemiol. 2005;34(2):467–474. |
Supplementary materials
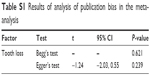  | Table S1 Results of analysis of publication bias in the meta-analysis |
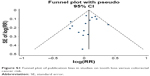  | Figure S1 Funnel plot of publication bias in studies on tooth loss versus colorectal cancer risk. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

