Back to Journals » Open Access Journal of Contraception » Volume 12
Time to Long-Acting Reversible Contraceptive Uptake Over Twelve Months Postpartum: Findings of the Yam Daabo Cluster Randomized-Controlled Trial in Burkina Faso and the Democratic Republic of the Congo
Authors Coulibaly A , Millogo T, Baguiya A , Tran NT , Thieba B, Seuc A , Cuzin-Kihl A , Landoulsi S, Kiarie J, Yodi R, Mashinda D, Kouanda S
Received 20 October 2020
Accepted for publication 11 February 2021
Published 9 March 2021 Volume 2021:12 Pages 73—82
DOI https://doi.org/10.2147/OAJC.S287770
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Abou Coulibaly,1 Tieba Millogo,2 Adama Baguiya,1 Nguyen Toan Tran,3 Blandine Thieba,4 Armando Seuc,5 Asa Cuzin-Kihl,5 Sihem Landoulsi,5 James Kiarie,5 Rachel Yodi,6 Désiré Mashinda,6 Séni Kouanda1
1Institut de Recherche en Sciences de la Santé (IRSS), Département Biomédical et Santé Publique, Ouagadougou, Burkina Faso; 2Institut Africain de Santé Publique, Ouagadougou, Burkina Faso; 3University of Technology, Faculty of Health, Australian Centre for Public and Population Health Research, Sydney, Australia; 4Université Joseph KI-ZERBO, Unité de Formation et de Recherche en Sciences de la Santé, Ouagadougou, Burkina Faso; 5World Health Organization, Department of Reproductive Health Research, Geneva, Switzerland; 6Université de Kinshasa, Ecole de Santé Publique, Kinshasa, République Démocratique du Congo
Correspondence: Abou Coulibaly
Institut de Recherche en Sciences de la Santé (IRSS), 03 B.P. 7047, Ouagadougou, 03, Burkina Faso
Tel +226 71 40 77 89
Email [email protected]
Purpose: An earlier adoption of contraceptive methods during the postpartum period could help women to extend the inter-pregnancy interval. This article aimed to determine and compare the timing of long-acting reversible contraceptives (LARC) use (ie, intrauterine device and implant) in Burkina Faso (BF) and DR Congo (DRC) between the intervention and control groups.
Patients and Methods: A total of 1120 postpartum women were enrolled and followed up to 12 months postpartum. We used Yam-Daabo trial data which was a multi-intervention, single-blinded, cluster-randomised controlled trial done in primary health-care centres (clusters) in both countries. Centres were randomly allocated to receive the six-component intervention or standard antenatal and postnatal care in matched pairs (1:1). We did a secondary analysis using Royston-Parmar’s semi-parametric model to estimate the effect of the interventions on the median time of LARC uptake.
Results: Our analysis included 567 postpartum women in BF (284 in the intervention group and 283 in the control group) and 553 in the DRC (274 in the intervention group and 279 in the control group). After showing an increase in family planning use in these two African countries, Yam Daabo’s interventions showed a reduction of the median time of LARCs adoption in the intervention group compared to the control group in both countries (difference of 39 days in Burkina Faso; difference of 86 days in the DR Congo).
Conclusion: The Yam Daabo intervention package resulted in increased and earlier adoption of LARC in rural settings in Burkina Faso and urban settings in DR Congo. Such an intervention could be relevant in similar contexts in Sub-Saharan Africa with very high fertility rates and high unmet needs for contraception.
Keywords: family planning, postpartum, long-acting reversible contraceptives, sub-Saharan Africa
Introduction
To prevent maternal deaths, family planning (FP) is an effective strategy to address women’s and couples’ fertility choices by helping them limit the number of children and extend the inter-pregnancy interval by at least two years.1 According to an analysis of 27 countries Demographic and Health Surveys (DHS), 95% of women who gave birth within the previous 12 months wished to avoid a pregnancy in the following 24 months, but up to 70% did not use contraception.2 Several interventions to help women satisfy their contraceptive needs in the postpartum period have been implemented in many countries. Research in different contexts, where interventions focused on counseling (during pregnancy and after childbirth), showed a significant increase in the use of contraceptive methods in the postpartum period.3,4 In contrast with single-intervention studies, Yam Daabo (which means “your choice” in Mooré, one of the local languages in Burkina Faso) was a cluster randomized-controlled trial that tested a set of different Postpartum family planning (PPFP) interventions implemented from the third trimester of pregnancy throughout the extended postpartum period until one year. Yam Daabo aimed at strengthening existing primary health-care services and did not focus on promoting a specific contraceptive method.
The DRC and Burkina Faso are two sub-Saharan Africa countries, with a population of 86,791,000 in 2019,5 for the DRC and 20,321,000 in 2019 for the BF.6 According to the study by Ahmed et al,7 the modern contraceptive prevalence rate (mCPR) among all women in Burkina was 24.7% and, 10.0% in the DRC in 2017. The unmet needs for modern method were respectively 27.2% and 39.9%. The demand satisfied with modern methods were respectively 47.6% and 20.0%. Similar to the majority of sub-Saharan African countries, cultural norms favor large families, with fertility rates higher in rural than urban areas. For instance, in 2019, Burkina Faso had 5.6 and the DRC 6.4 lives birth per woman.5,6
Yam Daabo was effective in increasing the use of modern PPFP methods at 12 months postpartum. In Burkina Faso, the modern contraceptive prevalence was 55% among women who received the package and 29% among those who received routine care in control clusters (adjusted prevalence ratio 1.79, 95% CI=1.30−2.47).8 In DR Congo, the modern contraceptive prevalence was 46% among women in the intervention group and 35% in the control group (adjusted prevalence ratio 1.58, 95% CI=0.74−3.38).9 But, Yam Daabo interventions had no effect on modern methods discontinuation.10
All of the studies that measured the effects of various interventions on postpartum family planning (PPFP) uptake did not explore the median time to contraceptives adoption. In other words, we do not know whether previous interventions contribute to earlier adoption of methods among women in the intervention group than those in the control group.
This paper aims to explore the time to long-acting reversible contraceptives (LARC) uptake in both countries. We are looking at the effect of Yam Daabo intervention on the time to long-acting reversible contraceptives by comparing this in intervention and control cohorts. We focused this analysis on LARC methods because they have specific advantages, including a high satisfaction rate and low discontinuation rate.11 Another reason for analyzing LARC uptake is that their use requires a skilled service provider who may not be available in certain outreach areas in low-income countries like Burkina Faso and DR Congo.12
Patients and Methods
We performed a secondary analysis of the Yam Daabo study, which was a two-group, multi-intervention, single-blinded, cluster-randomized controlled trial with health centres as the randomization units. The study involved two countries: Burkina Faso and the DR Congo.
Health centers were eligible if (1) they offer the continuum of antenatal care, delivery, and postnatal care; (2) they provide a selection of at least three modern contraceptive methods, including a barrier method such as condom, a short-term method such as pills, a long-term method such as intra-uterine device and referrals for permanent methods to clients; (3) there were no stock-outs of contraceptives during the preceding six months; (4) they have on average at least thirty deliveries per month; (5) they are situated within four hours drive from the research center; and (6) they are willing to participate. Thus, in each country, eight others were allocated randomly to the experimental and control groups of the intervention phase. So, we conducted the trial in eight primary health centers which were matched by pairs according to (1) the average number of deliveries per month, (2) the ratio of health workers per population, and (3) the settings (rural, urban). Within each of the four pairs, we randomly selected the site assigned to the experimental intervention. All pregnant women were eligible to participate in the study if (1) they were in their third pregnancy trimester; (2) the status of the pregnancy and the woman allowed for a birth at the health center; (3) the woman had the intention to attend ANC, delivery, and PNC at the health center; (4) the woman did not participate in another study; and (5) we obtained informed consent. Research assistants collected data on paper-based Case Report Forms (CRF). The world health organization (WHO) team in Geneva developed the CRF with inputs from the country research teams. Each health center had a research assistant who was trained to adhere to the study manual and standard operating procedures for data management, which are common to both study countries and have been developed by WHO. The information reported on the CRFs was checked for accuracy and completeness several times at different levels by field coordinators and data managers. The Biostatistics and Data Management team developed the electronic CRF (eCRF) through OpenClinica (version 3.11), an electronic data capture software for clinical research, which includes programmed edit checks for data accuracy, completeness, and consistency, reduces delays in data queries and problem resolution. Further methodological details on the Yam Daabo trial are available elsewhere.13
Study Period
We have included pregnant women from July 27 to October 17, 2016. We followed all the pregnant women up to twelve months after delivery. So, the last follow-up date was February 28, 2018.
Interventions
The package comprised three facility-based interventions (PPFP refresher course for providers, supportive supervision, and availability of contraceptive services seven days a week) and three client-oriented interventions (invitation letter to husbands or partners, appointment card, and a decision-making tool for clients and providers to enable a systematic counseling approach on PPFP).
The health centers of the experimental group implemented the PPFP intervention package. The control group implemented the usual care. Depending on the final package’s nature, some were implemented before participant recruitment (such as PPFP refresher training for service providers). In contrast, others were implemented afterward (such as using the PPFP counseling tool with participants). Participants received individual-based interventions during third-trimester antenatal care visits and postnatal care follow-up visits, according to national practice (typically on clinical discharge [24−48 h], at 6 days, 6 weeks, then at months 6 and 9, before the trial exit at month 12 postpartum). In many African countries, the routine Postpartum care (PPC) is offered to women at different times, based on WHO recommendations. The WHO guidelines for maternal and infant Postpartum care (PPC) include guidance on routine care, such as monitoring the wellbeing of the mother and/or baby, early detection and management of complications, preventive measures and counseling, and family planning. The recommended timing, including the number of postpartum contacts for all mothers and newborns, evolved from the renowned formula of “6 hours, 6 days, 6 weeks and 6 months” after birth to four postpartum visits: on the first day, at day 3 (48–72 h), between days 7–14, and 6 weeks after birth.14
Outcomes
In this analysis, we focused on LARC methods (Intrauterine devices and implants). We did not consider the short-acting methods (pills, injectables, condoms, spermicides, and the lactational amenorrhea method). We performed an intention-to-treat analysis, and our event of interest was the LARC uptake.
Statistical Analysis
Considering the choice of our outcome and the data’s nature, we opted for survival analysis. Since we performed a survival analysis, we focused on the distribution of the aleatory variable, elapsed time from delivery until the adoption of a LARC, continuously positive, noted as T among the study’s women. A woman is called “right-censured” when she is still at risk of adopting a LARC at twelve months postpartum. In our study, all the participants are “left-truncated” because a woman can adopt a LARC only after delivery, meaning that before delivery, the woman cannot adopt a LARC. There is a date of origin for each woman, which is the date of delivery, and thus, the beginning of the follow-up, and an end date of the follow-up (12 months postpartum). If the participant adopted of LARC during the follow-up, this end-of-observation date corresponds to the date of LARC use. If the participant did not adopt a LARC during the follow-up, the end date corresponds to the study’s end date (ie, 12 months postpartum). For women lost to follow-up, the end date is the date of the last interview conducted. Thus, we obtain a duration until LARC use for each participant or until the end of the observation period, which will allow us to estimate the probability of LARC use.
For the selection of the type of modeling, we compared the different models (Kaplan-Meier non-parametric modeling, parametric modeling (Weibull, Exponential, Gompertz, Loglogistic, Lognormal, G-gamma and Royston–Parmar), and semi-parametric modeling (Cox’s modeling)) using the Akaike’s Information Criteria (AIC). The Royston-Parmar’s flexible model had the lowest AIC and was therefore selected.
We used the Stata stpm2 command15 to estimate the intervention effect on LARC use. This command fits flexible parametric regression models (Royston–Parmar models using restricted cubic splines functions) by directly modeling the cumulative incidence function (CIF). The command also produces estimates of hazard ratios (HR) for our exposure variable. We adjusted the results for all the variables found to be imbalanced between the intervention and control group. To be consistent with comparing the adjusted hazard ratios between the two countries, we calculated stratified rate ratios and significance tests by using a Mantel-Haenszel-type method. We also produced the CIF curves for LARC uptake over time in each country and computed the median survival time and restricted mean survival time of adopting a LARC.
Ethics Approval
The trial was approved by the WHO Research Ethics Review Committee, the ethics committee for health research in Burkina Faso, and the School of Public Health ethics committee in DR Congo. Moreover, the trial was registered in the Pan African Clinical Trials Registry (PACTR201609001784334) and was conducted in accordance with the Declaration of Helsinki.
Results
Our analysis included 567 postpartum women in Burkina Faso (284 in the intervention group) and 553 in DR Congo (274 in the intervention group). Figure 1 section summarizes the study flow.
 |
Figure 1 Flowchart of the study. Abbreviation: LARC, long-acting and reversible contraceptives. |
The baseline comparison between the control and the intervention group showed with Burkina Faso’s data a significant difference for the woman’s age (p=0.021), the number of pregnancies (p=0.048) and the number of abortion (p=0.007). The DRC data comparison showed a significant difference for the number of stillbirths (p=0.017), the education status (p=0.008) and the woman’s occupation (p=0.000). All these results are expressed in Table 1.
 |
Table 1 Baseline Characteristics of Women at Inclusion After Delivery |
Effect of the Interventions on LARC Adoption
The adjusted results showed a positive effect of the interventions on LARC adoption in Burkina Faso (Table 2): at 12 months postpartum, when compared to the control group, women in the intervention group were 2.11 times more likely to use LARC (95% CI=1.48–3.02; p<0.001). In the DR Congo, women of the intervention group were 3.5 times more likely to use LARC (HR=3.48; 95% CI=2.08–5.84; p<0.001) when compared to the control group women. However, there was no difference between the two countries’ adjusted rate ratio (p=0.344), meaning no difference between comparison of Burkina Faso and the DRC results.
 |
Table 2 Use of Long-Acting and Reversible Contraceptives at 12 Months Postpartum |
Effect of the Interventions on the Median Time of Contraceptive Methods Adoption
Analysis of the median survival time and the restricted mean survival time of contraceptive methods adoption showed differences between the intervention and control groups in both countries (Table 3). In Burkina Faso, for the median survival time, there was on average a difference of 39 days (5 weeks and 4 days) for time to LARC uptake, as users in the intervention group adopted their method at 55 days postpartum (just under 2 months) against 94 days (more than 3 months) in the control group. In DR Congo, the difference was 86 days (close to 3 months), with a median time to LARC uptake at 75 days postpartum (2.5 months) in the intervention group versus 161 days (approximately 5 months and 15 days) in the control group.
 |
Table 3 Proportion of Long-Acting and Reversible Contraceptives Users and Median Survival Time and Restricted Mean Survival Time (RMST) of Adoption |
Analysis of the restricted mean survival time of LARC adoption showed similar differences. These differences are also expressed in Figure 2. On this figure, we noted that the cumulative incidence curve of the Burkina comparison group has a similar evolution over the time to that of the intervention group in DR Congo.
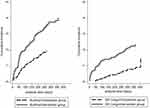 |
Figure 2 Cumulative incidence of long-acting reversible contraceptives adoption. |
Discussion
Findings and Interpretations
First, although Yam Daabo did not promote a particular method, our results showed that Yam Daabo interventions had similar effects on significantly increasing LARC adoption in Burkina Faso and DR Congo as compared intensity testing between the two countries did not find a significant difference. It is important to note that the majority of LARC services concerned implants, as service providers at the primary health-care clinics enrolled in Yam Daabo, were mostly auxiliary midwives or nurses who were not allowed to offer IUDs, unlike midwives or physicians. LARC methods provide security against pregnancy and are simple to use (no daily or periodic administration) and cost-effective in the long term. According to Secura, in 2013, the use of LARC is more than 99% effective against pregnancies and over 20 times more effective at preventing unintended pregnancy compared to the contraceptive pill, patch, or ring.16 The effect of Yam Daabo on LARC uptake maybe because its interventions addressed several service utilization barriers like the low knowledge and skills of service providers, misconceptions among providers and clients. Providers’ adequate knowledge and skills, which were strengthened by supportive supervision, combined with quality counseling over several encounters, were likely contributing factors.
Second, our results showed an earlier adoption of LARC in the intervention groups of both countries. On average, the control groups, which received routine care, adopted LARC later than the 6-week postpartum visit, which is dedicated in both countries to PPFP information and services. In Burkina Faso, it was at 3 months postpartum for LARC, which contrasted with a much later adoption in the DRC at more than 5 months postpartum for LARC. Our Yam Daabo formative research already revealed that women appeared to rarely attend the 6-week postpartum visit,17 which is confirmed by this secondary analysis. Nonetheless, for similar contexts in Sub-Saharan Africa, our interventions could help improve an earlier and increased adoption of postpartum contraceptives, which could help women effectively extend their inter-pregnancy interval or limit the number of children. So, regarding the advantages of LARC, further research must focus on reducing the time to LARC uptake, especially in postpartum women. The decision-makers and health providers should support women in attending the six-week visit and ensuring that they can adopt a LARC early (no stock-outs, availability of skilled providers).
Third, as noted above, there was an earlier adoption of LARC in Burkina Faso than in the DRC. In addition to the difference in research settings (rural vs urban), various factors could further explain the contrasting results, including the heterogeneity between both countries in terms of perinatal policies and systems; varying levels of facility-based delivery; differences in maternity care providers; heterogeneous quality of care; and other determinants pertaining to contexts, values, and experiences of postpartum care. Yam Daabo interventions aimed to strengthen some of these factors within an overall primary health-care service strengthening approach, which was aligned with national health policies.13 While 91% of the 766 health facilities in Burkina Faso surveyed in the Service Availability and Readiness Assessment (SARA) survey offered at least one method in 2014, only 33% of the 1555 health facilities surveyed in the DRC provided at least one method in 2014. When comparing the proportion of health facilities offering implants, it was 80% in BF in 2014 compared to 11% in DRC in the same year.18 Comparison of the proportions of health facilities that experienced contraceptive stock-outs also shows enormous disparities. Moreover, besides, to support the idea of structural differences between the health systems and policies of both countries, an analysis of the DHS data in Burkina (2010) and the DR Congo (2013), showed differences between the proportions of women who attended postpartum visits at six weeks. In Burkina Faso, 72% of postpartum women received postnatal care within 48 hours of childbirth against 44% in DR Congo. Moreover, 52% of women did not receive postnatal care (including late care, ie, 41 days after delivery) in DR Congo19 against 17% in Burkina Faso.20 However, during this period, counseling may be critical to equip women with knowledge to inform the adoption of contraceptive methods of their choice. Thus, if women do not return to health centers, they will not be adequately exposed to PPFP information and services. Also, according to Kwete et al, several factors could explain the high reliance on traditional methods in DR Congo, which would delay their adoption of modern contraceptives: the years of political turmoil that led to a scarcity of medical supplies, the deeply ingrained fear of side effects (particularly the sterility) from modern methods, and the promotion of natural methods by faith-based organizations that run more than half of the health facilities in the country.21 All the factors mentioned above could have had an effect on time to LARC uptake.
Limitations
In the present study, we focused on the timing of LARC uptake among postpartum women. The limitations described in the main papers are also valid for this secondary analysis. It is essential to mention that three out of four control sites in the DRC have been contaminated during the trial by implementing other family planning interventions. In these three control sites, despite not focusing on postpartum family planning, these interventions were linked to HIV or family planning programming and were also offered to women postpartum, including to Yam Daabo participants. These interventions delivered free family planning services in one center, including long-acting and reversible contraceptives, providing free contraceptive methods and services in the other center. In the last center, the intervention was free condom distribution and other family planning methods and services. During these interventions, the implant was free, but its insertion services were not. So, in the DRC, the Yam Daabo intervention package was not compared with typical routine care, but with other family-planning-related activities. However, our postpartum family planning-focused intervention, compared with other family-planning-related activities in control sites, proved more effective in enabling women to adopt a LARC.
Our study had no data on husband approval of contraceptive initiation and resumption of sexual activity. Several authors have found these variables to influence postpartum use of a modern contraceptive method.22,23 Therefore, the time of a LARC initiation is also influenced by these variables.
Conclusion
Yam Daabo’s interventions showed a reduction of the median time of LARCs adoption in the intervention group compared to the control group in two African countries with different contexts. These results have critical programmatic implications for countries with very high fertility rates with high unmet needs for contraception.
Data Sharing Statement
Requests for the anonymized, coded trial data can be made to the Department of Reproductive Health and Research, World Health Organization ([email protected]). Data sharing is subject to WHO data sharing policies and data use agreements with the participating research centres.
Acknowledgments
This work was carried out as part of the epidemiology thesis of the corresponding author. Special thanks go to the World Health Organization for agreeing to provide us the database for secondary analyzes and for offering the scholarship of doctoral studies in epidemiology. We also thank the Government of France generously provided funding for this research grant in the context of the Muskoka Initiative on Maternal and Child Health.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study funder (Government of France) had no role in study design, data collection, data analysis, data interpretation, or writing the Article.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. World Health Organization. Maternal mortality. February 16, 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
2. Ross JA, Winfrey WL. Contraceptive use, intention to use and unmet need during the extended postpartum period. Int Fam Plan Perspect. 2001;27:20–27. doi:10.2307/2673801
3. Ahmed S, Ahmed S, McKaig C, et al. The effect of integrating family planning with a maternal and newborn health program on postpartum contraceptive use and optimal birth spacing in rural Bangladesh. Stud Fam Plann. 2015;46(3):297–312. doi:10.1111/j.1728-4465.2015.00031.x
4. Huang Y, Merkatz R, Zhu H, Roberts K, Sitruk-Ware R, Cheng L. The free perinatal/postpartum contraceptive services project for migrant women in Shanghai: effects on the incidence of unintended pregnancy. Contraception. 2014;89(6):521–527. doi:10.1016/j.contraception.2014.03.001
5. United Nations. Country profile: Democratic Republic of Congo. UNdata website. Available from: http://data.un.org/en/iso/cd.html.
6. United Nations. Country profile: Burkina Faso. UNdata website. Available from: http://data.un.org/en/iso/bf.html.
7. Cahill N, Sonneveldt E, Stover J, et al. Modern contraceptive use, unmet need, and demand satisfied among women of reproductive age who are married or in a union in the focus countries of the family planning 2020 initiative: a systematic analysis using the family planning estimation tool. Lancet. 2018;391(10123):870–882. doi:10.1016/S0140-6736(17)33104-5
8. Tran NT, Seuc A, Coulibaly A, et al. Post-partum family planning in Burkina Faso (Yam Daabo): a two group, multi-intervention, single-blinded, cluster-randomised controlled trial. Lancet Glob Health. 2019;7(8):e1109–e1117. doi:10.1016/S2214-109X(19)30202-5
9. Tran NT, Seuc A, Tshikaya B, et al. Effectiveness of post-partum family planning interventions on contraceptive use and method mix at 1 year after childbirth in Kinshasa, DR Congo (Yam Daabo): a single-blind, cluster-randomised controlled trial. Lancet Glob Health. 2020;8(3):e399–e410. doi:10.1016/S2214-109X(19)30546-7
10. Coulibaly A, Millogo T, Baguiya A, et al. Discontinuation and switching of postpartum contraceptive methods over twelve months in Burkina Faso and the Democratic Republic of the Congo: a secondary analysis of the Yam Daabo trial. Contracept Reprod Med. 2020;5(1):35. doi:10.1186/s40834-020-00137-2
11. Steele F, Curtis S. Appropriate methods for analyzing the effect of method choice on contraceptive discontinuation. Demography. 2003;40(1):1–22. doi:10.1353/dem.2003.0009
12. Mpunga D, Lumbayi J, Dikamba N, Mwembo A, Ali Mapatano M, Wembodinga G. Availability and quality of family planning services in the Democratic Republic of the Congo: high potential for improvement. Glob Health Sci Pract. 2017;5(2):274–285. doi:10.9745/GHSP-D-16-00205
13. Tran NT, Gaffield ME, Seuc A, et al. Effectiveness of a package of postpartum family planning interventions on the uptake of contraceptive methods until twelve months postpartum in Burkina Faso and the Democratic Republic of Congo: the YAM DAABO study protocol. BMC Health Serv Res. 2018;18(1):439. doi:10.1186/s12913-018-3199-2
14. World Health Organization. Postpartum care of the mother and newborn: a practical guide. Technical Working Group, World Health Organization. Birth Berkeley Calif. 1999;26(4):255–258. doi:10.1046/j.1523-536x.1999.00255.x
15. Lambert PC, Royston P. Further development of flexible parametric models for survival analysis. Stata J. 2009;9(2):265–290. doi:10.1177/1536867X0900900206
16. Secura G. Long-acting reversible contraception: a practical solution to reduce unintended pregnancy. Minerva Ginecol. 2013;65(3):271–277.
17. Tran NT, Yameogo WME, Gaffield ME, et al. Postpartum family-planning barriers and catalysts in Burkina Faso and the Democratic Republic of Congo: a multiperspective study. Open Access J Contracept. 2018;9:63–74. doi:10.2147/OAJC.S170150
18. Ali M, Farron M, Ramachandran Dilip T, Folz R. Assessment of family planning service availability and readiness in 10 African countries. Glob Health Sci Pract. 2018;6(3):473–483. doi:10.9745/GHSP-D-18-00041
19. Ministère du Plan et Suivi de la Mise en oeuvre de la Révolution de la Modernité (MPSMRM), Ministère de la Santé Publique (MSP) and, ICF International. Demographic and Health Survey in the Democratic Republic of the Congo 2013-2014.
20. Institut National de la Statistique et de la Démographie (INSD) and ICF International. Demographic and Health Survey and Multiple Indicator Cluster Survey, Burkina Faso 2010.
21. Kwete D, Binanga A, Mukaba T, et al. Family planning in the Democratic Republic of the Congo: encouraging momentum, formidable challenges. Glob Health Sci Pract. 2018;6(1):40–54. doi:10.9745/GHSP-D-17-00346
22. Emiru AA, Alene GD, Debelew GT. The role of maternal health care services as predictors of time to modern contraceptive use after childbirth in Northwest Ethiopia: application of the shared frailty survival analysis. PLoS One. 2020;15(2):e0228678. doi:10.1371/journal.pone.0228678
23. Berta M, Feleke A, Abate T, Worku T, Gebrecherkos T. Utilization and associated factors of modern contraceptives during extended postpartum period among women who gave birth in the last 12 months in Gondar Town, northwest Ethiopia. Ethiop J Health Sci. 2018;28(2):207. doi:10.4314/ejhs.v28i2.12
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
