Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Thyroidectomy Using the Lateral Cervical Small Incision Approach for Early Thyroid Cancer
Authors Jin XX, Zhang QY, Gao C, Wei WX, Jiao C, Li L, Ma BL, Dong C
Received 18 January 2022
Accepted for publication 30 March 2022
Published 20 April 2022 Volume 2022:15 Pages 713—720
DOI https://doi.org/10.2147/CCID.S358959
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Jeffrey Weinberg
Xi-Xin Jin,1 Qian-Yu Zhang,2 Chao Gao,1 Wen-Xin Wei,1 Chong Jiao,1 Li Li,3 Bin-Lin Ma,1 Chao Dong1
1Department of Breast, Head and Neck Surgery, Affiliated Cancer Hospital of Xinjiang Medical University, Urumqi, Xinjiang, People’s Republic of China; 2Department of Oral and Maxillofacial Surgery, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, Guangdong, People’s Republic of China; 3Department of Gynecology and surgery, Affiliated Cancer Hospital of Xinjiang Medical University, Urumqi, Xinjiang, People’s Republic of China
Correspondence: Chao Dong, Department of Breast, Head and Neck Surgery, Affiliated Cancer Hospital of Xinjiang Medical University, Urumqi, Xinjiang, People’s Republic of China, Tel +86 13999111211, Email [email protected]
Objective: Surgical resection is the main treatment for thyroid cancer, but while traditional open thyroidectomy improves prognosis, it also results in poor cosmetic outcomes. Therefore, we devised the lateral cervical small incision approach to thyroidectomy and will evaluate its efficacy.
Methods: The clinicopathological data of 191 patients who underwent unilateral thyroidectomy and isthmusectomy for early thyroid cancer were collected retrospectively. Of these, 100 patients underwent a traditional thyroidectomy using the median cervical approach (control group), and 91 patients underwent a thyroidectomy using the lateral cervical small incision approach (experimental group). The differences in perioperative prognosis, postoperative complications, and cosmetic outcomes between the two groups were evaluated.
Results: There was no significant difference in sex, age, tumor size, lymph node dissection, number of metastases, or postoperative complications between the experimental group and the control group (P > 0.05). There were significant differences in the duration of the operation; postoperative blood loss, drainage, and hospital stay; and scar color, blood circulation, hardness, and thickness between the groups (P < 0.05). The cosmetic outcomes of the incisions in the experimental group were more satisfactory than in the control group (P < 0.05).
Conclusion: When compared with traditional open thyroidectomy, the lateral cervical small incision approach has a lower incidence of complications, a better perioperative prognosis, and an improved cosmetic outcome.
Keywords: thyroid carcinoma, lateral cervical approach, small incision, surgical operation, thyroidectomy, neck aesthetics, comparative study
Introduction
Thyroid tumors are the most common malignant tumors of the endocrine system and are frequently found in females.1 Surgical resection is the main treatment for thyroid cancer and greatly improves prognosis.2 However, postoperative complications, such as poor cosmetic outcomes, scar adhesion, and hyperplasia, pose challenges for thyroid surgeons, especially in traditional thyroid surgery using a midline cervical incision, and the incidence of scar adhesion and hyperplasia is high.3 Endoscopic surgery has been used in thyroid surgery, and there have recently been noteworthy developments in this type of surgery. In 1996, Gagner et al4 first introduced the endoscopic technique for use in parathyroidectomy. Subsequently, with developments in endoscopic surgery, Miccoli et al5 performed small-incision thyroid surgery. Although these types of surgeries result in better cosmetic outcomes for patients, they require a high level of technical ability from the surgeon and have disadvantages, such as long operation times and high costs.6 Therefore, it is important to develop new surgical approaches.
Qin et al7 found that during thyroid surgery, it is better to expose the superior thyroid and superior laryngeal nerves using the anterior cervical intermuscular approach, as this results in a significantly lower incidence of postoperative negative voice outcomes, but this approach has a poor cosmetic outcome. As the anterior cervical band muscle space is located in the lateral neck, if a small incision is made in the lateral neck for unilateral thyroid gland lobectomy and isthmusectomy, the anterior cervical band muscle space and superior thyroid will be suitably exposed. Using this approach, the nerves may be avoided, reducing the incidence of surgical complications, and the incision can be hidden under the collar to achieve an ideal cosmetic outcome. Therefore, in this study, we aim to establish the lateral cervical small incision approach for thyroidectomy in patients with early thyroid cancer and evaluate its efficacy.
Materials and Methods
Patients
A total of 191 patients who underwent unilateral glandular lobectomy and isthmusectomy for early thyroid cancer from June 2019 to December 2019 were enrolled in this retrospective study. A preoperative ultrasonography-guided fine-needle puncture biopsy was performed on all patients to confirm stage T1 single differentiated papillary thyroid carcinoma in the unilateral thyroid lobe (tumor size: ≤2 cm), and the absence of cervical lymphadenopathy was confirmed in all patients via a computed tomography scan and ultrasonography. In addition, each patient underwent a thyroid function test and an esophageal and indirect laryngoscopy preoperatively in order to exclude esophageal and laryngeal lesions. The exclusion criteria were as follows: 1) undifferentiated thyroid carcinoma, enlarged lymph nodes in the lateral neck, and esophageal or laryngeal lesions and 2) hyperthyroidism; benign thyroid tumor; previous neck surgery; coagulation dysfunction; abnormal function of the heart, liver, or kidney; surgical or drug contraindications; suspected malignant thyroid carcinoma; cervical lymph node enlargement; or esophageal, pharyngeal, or laryngeal lesions. All operations were performed by the same group of doctors, all subjects signed informed consent prior to enrollment, the study was approved by the institutional review board of the Affiliated Cancer Hospital of the Xinjiang Medical University, and all interventions were performed under committee supervision in accordance with the relevant guidelines and regulations.
Surgical Approach
Preoperatively, the appropriate operative approach was established for each patient based on the preoperative physical and imaging examinations, tumor characteristics, and other factors. Each patient was placed in a seated position, and the incision was planned in a way that would allow it to be covered in the patient’s everyday life (eg, for male subjects the incision could be covered by wearing a collared shirt and in female subjects by wearing a necklace). In addition to cosmetic considerations, the location of the thyroid lesion was considered. A diagonal arc incision was planned and drawn at the left or right supraclavicular fossa, depending on the location of the lesion. The length of the incision depended on the characteristics of the tumor but was approximately 3.0–4.5 cm (see Figure 1A).
 |
Figure 1 Lateral cervical small incision approach (A). Skin incision (B). Exposure of the superior pole of the thyroid (C). Exposure of external branch of superior laryngeal nerve. |
All patients underwent surgery under general anesthesia with tracheal intubation. For the lateral cervical small incision approach, to fully expose the neck surgical field, patients were placed in the supine position with their shoulders and back raised and their head tilted back. An incision was made along the marked line, and the platysma myoides were exposed and resected. After loosening the flap up and down along the deep surface of the platysma, the anterior margin of the sternocleidomastoid muscle and the anterior neck muscle group were exposed. The sternohyoid muscle and the lateral edge of the sternothyroid muscle were longitudinally split to reveal the thyroid gland. The anterior cervical muscle group was pulled to the healthy side of the thyroid gland, and the intrinsic thyroid membrane and surgical membrane space, the natural space between the sternothyroid muscle and the thyroid gland, were opened. The inner side of the cervical sheath (internal jugular vein) and the lateral border of the sternothyroid muscle were separated. The natural gap between the deep surface of the anterior cervical band muscle and the thyroid was opened (see Figure 1B).
Separation range: the inner side of the separation was the thyroid isthmus near the healthy side of the thyroid, the outer side was the carotid sheath, the lower boundary was the notch of the sternum, and the upper boundary was the upper thyroid. A stable and clear surgical space was established to fully expose the affected thyroid lobe (see Figure 1B). A perioperative frozen biopsy was performed to confirm papillary thyroid cancer. After carefully freeing the thyroid tissue, the bleeding at the thinnest part of the thyroid tissue was stopped if the unilateral thyroid lesion was a solid cystic mass.8 The tumor and the ipsilateral thyroid lobe were removed together. During the operation, the RLN was identified and preserved and the prophylactic central lymph node dissection was performed (see Figure 1C), according to the recommendations in the Diagnosis and Treatment of Papillary Thyroid Microcarcinoma (2016 edition).9 The parathyroid glands were retained in situ, and their microcirculation was protected. Upon completion of the surgery, a drainage tube was placed on the outer edge of the original incision, without additional punching, and the wound was closed.10
Postoperative Treatment
Postoperatively, a standard treatment protocol was administered to all patients regardless of the surgical approach, and the adjuvant endocrine therapy included thyroid stimulating hormone suppression therapy with levothyroxine sodium tablets. Postoperative complications, such as recurrent laryngeal nerve injury, hypoparathyroidism (hypocalcemia), local effusion, postoperative bleeding, hematoma, and infection, were closely monitored. The drainage tube was removed when the drainage volume was <20 mL/d and the drainage fluid was clear. If there were no postoperative complications and the drainage tube had been removed, the patient was discharged.
Follow-Up
The postoperative follow-up was performed via outpatient visits. The patients were followed up quarterly in the first year, biannually in the second year, and at least annually thereafter.
Data Collection
The demographic and clinicopathological data of all enrolled patients, including tumor size, intraoperative blood loss, postoperative drainage, postoperative complications, length of hospital stay, and lymph node dissection and metastases, were collected.
Outcome Evaluation and Patient Satisfaction
Two months postoperatively, the Vancouver Scar Scale (VSS) and the Observer Scar Evaluation Scale (OSAS)11 were administered to patients face-to-face and evaluated by the doctors. The patients received no incentives for completing the surveys, and no patients declined to answer them. In the VSS, the scars were scored based on color, blood circulation, thickness, and softness. The scoring system is as follows: 1) Pigmentation: The color of the scar is similar to or no different from that of normal skin (0 points), light pink (1 point), a mixture of light and dark (2 points), or dark (3 points). 2) Vascularity: The color of the scar is close to that of normal skin (0 points), pink (1 point), red (2 points), or dark red (3 points). 3) Height: The thickness of the scar is similar to that of normal skin (0 points), >0 and <1 mm (1 point), ≥1 and <2 mm (2 points), 2–4 mm (3 points), and >4 mm (4 points). 4) Pliability: The texture of the scar is approximately as soft as normal skin (0 points), soft with skin deformation under minimal resistance (1 point), slightly tense (2 points), hard (3 points), curved and contracts when stretched (4 points), or contracted, eg, joint deformities (5 points). In the OSAS, the scars are scored on a scale of 0–10 points based on blood vessel distribution, color, thickness, softness, and surface area. The lower the score, the better the degree of scar recovery. Patient satisfaction was surveyed using the satisfaction survey from the (China) National Health Commission Satisfaction Survey Platform.
Statistical Analysis
All statistical analyses were conducted using SPSS 26.0 (IBM, USA). P < 0.05 (two sided) was considered statistically significant. Continuous variables were expressed as mean ± SD and compared using the t-test, and categorical variables were compared using the chi-squared test.
Results
Baseline Characteristics
A total of 191 patients (28 males and 163 females) were enrolled in this study, with a mean age of 44.8 ± 10.1 y. There were 91 patients (15 males and 76 females) in the lateral cervical approach group (experimental group) aged 17–67 y, with an average age of 43.51 ± 9.34 y. There were 100 patients (13 males and 87 females) in the traditional approach group (control group) aged 28–74 y, with an average age of 45.91 ± 10.71 y. There was no significant difference in sex, age, tumor size, lymph node dissection, or number of metastases between the groups (P > 0.05; see Table 1).
 |
Table 1 Basic Clinical Information of Patients |
Perioperative Prognosis
There were significant differences between the experimental group and the control group in operation duration (38.69 ± 3.34 and 89.99 ± 21.94 min, respectively), intraoperative bleeding volume (19.61 ± 11.45 and 30.85 ± 9.69 mL, respectively), postoperative drainage (17.58 ± 4.17 and 51 ± 17.9 mL, respectively), and postoperative hospital stay (2.38 ± 0.62 and 3.4 ± 1.34 days, respectively; P < 0.05; see Table 1).
Postoperative Complications
Routine complications after thyroidectomy include recurrent laryngeal nerve injury, hypoparathyroidism (hypocalcemia), local effusion, postoperative bleeding, hematoma, and wound infection. No postoperative bleeding, hematoma, or wound infection occurred in either of the groups (see Table 2), and there was no significant difference in the occurrence of complications between the two groups. There was one case of recurrent laryngeal nerve injury, manifesting as postoperative hoarseness, in the experimental group and three in the control group, and after symptomatic treatment, all these patients recovered within one month. No cases of permanent laryngeal nerve injury were found. There was one case of hypoparathyroidism, manifesting as hypocalcemia, in the experimental group and four in the control group. All these patients recovered within one month, and no cases of permanent hypoparathyroidism were found. There were no cases of local effusion in the experimental group and three in the control group. In all three cases, the local effusion was observed after drainage removal but did not require surgical drainage or aspiration.
 |
Table 2 Postoperative Complications |
Cosmetic Outcomes
The color, blood circulation, softness, and thickness of the scars were evaluated using the VSS and the OSAS, and the patients in the experimental group were more satisfied with the cosmetic outcomes of the incisions (P < 0.05; see Table 3).
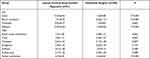 |
Table 3 Cosmetic Outcome |
Discussion
With improvements in surgical technology and the increasingly stringent cosmetic requirements of patients, minimally invasive techniques, such as endoscopic procedures, including complete endoscopic thyroid surgery and endoscope-assisted thyroidectomy,12 have been widely used in thyroid surgery.13 Complete endoscopic thyroid surgery results in a satisfactory cosmetic outcome, with no scar on the patient’s neck. In an endoscope-assisted thyroidectomy, a small incision is made on the neck, and the operative field is exposed with the assistance of an endoscope, without the need for gas to establish a surgical space. When compared with traditional surgery via the median approach, endoscope-assisted thyroidectomy has a shorter operative time and lower trauma rate but a higher cost, which limits the widespread use of endoscopic thyroid surgery.14,15 Therefore, compared with endoscopic assisted thyroidectomy, open thyroidectomy is still the main treatment for thyroid cancer, and the operation cost is lower.16
As a result, open thyroidectomy is still the primary treatment for thyroid cancer. However, traditional open thyroidectomy has some disadvantages, including a long incision (see Figure 2A); complete transection of the anterior cervical muscle group, resulting in significant trauma and bleeding (see Figure 2B and C); postoperative swallowing discomfort; surgical scarring; and poor cosmetic outcomes (see Figure 3A).17,18 It has been reported that open thyroidectomy with prophylactic lymphadenectomy will cause more complications.19 Consequently, we designed the lateral cervical small incision approach, which minimizes the damage caused by open surgery and has the following advantages: 1) A small incision (approximately 3.0–4.5 cm). The neck is cut along the predefined line. The longitudinal line between the sternocleidomastoid muscle and the band muscle is not cut, and the normal physiological space of the neck is used. As a result, postoperative lymph node edema caused by injury, pain from local swelling, and recovery time is reduced. In addition, the scar can be completely covered by simple jewelry, such as a necklace, or a collared shirt. 2) No injury to the anterior cervical area (see Figure 3B and C), the superior laryngeal nerves are protected, the operative time is reduced, and postoperative neck discomfort is decreased by using normal gaps.
 |
Figure 2 Median cervical approach (A). Skin incision (B). Exposure of the superior pole of the thyroid (C). Exposure of the external branch of the superior laryngeal nerve. |
The aim of the lateral cervical small incision approach is to reduce tissue injury during the operation and improve cosmetic outcomes. The indications for this surgery are as follows: 1) no history of neck surgery; 2) a benign thyroid lesion with a diameter <5 cm or bilateral thyroid lesions with a diameter ≤2 cm on one side and <3 cm on the other side; 3) low-grade malignant tumor of the thyroid gland with a tumor diameter <2 cm, with no need for large-scale cervical lymph node dissection; or 4) cystic thyroid adenoma. According to these indications, most thyroid surgical procedures can be completed using this approach, making it significantly more widely applicable than endoscopic surgery. In addition, this surgical approach does not require specialized surgical instruments.
In addition, research reports show that Lymph node yield (LNY) during initial central neck dissection (CND) surgery is an independent prognostic factor for recurrent/persistent disease in the central neck, LNY = 11 in bilateral CND procedures is an optimal number in estimating the prognosis of PTC patients undergoing total thyroidectomy plus bilateral CND.20 The median number of central lymph node dissection (CND) and lymph node metastasis (LNY) in the lateral neck small incision approach group were 6 (2–7) and 0 (0–3), respectively. The median of central lymph node dissection (CND) and lymph node metastasis (LNY) in the traditional median approach group were 6 (2–7) and 0 (0–3), respectively. The results showed that there was no difference in the number of lymph node dissection and lymph node metastasis between the two groups. Studies have reported that the LNY of the initial CND operation is an independent prognostic factor for recurrent/persistent diseases in the central neck, and the LNY of bilateral CND operation is 11, which is the best number for the prognosis of PTC patients undergoing total thyroidectomy plus bilateral CND. Therefore, the LNY in CND surgery in both groups is less than 11, suggesting that the probability of reexamination is low.
This study has some limitations. First, the lateral cervical small incision approach can only be used to remove a unilateral goiter. Second, the cosmetic effect of the cervical small incision approach is slightly worse than that of complete endoscopic surgery, and patients still need to use neck accessories or clothing to hide the scar.
Conclusions
When compared with a conventional thyroidectomy approach, the lateral cervical small incision approach had a lower incidence of complications, a better perioperative prognosis, and an improved cosmetic outcome, making it a safe and effective surgical approach for patients with early thyroid cancer. However, the lateral approach is most applicable to patients with confirmed unilateral papillary thyroid carcinoma, with a tumor size ≤2 cm, no esophageal or laryngeal lesions, and no prior history of neck surgery or radiotherapy.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Affiliated Cancer Hospital of Xinjiang Medical University (No.K-2019039). Written informed consent was obtained from all participants.
Funding
This study was funded by the Science and Technology Assistance Project of the Science and Technology Department of the Autonomous region (2018E02055). The funders have no any role in this study.
Disclosure
The authors declare that they have no competing interests.
References
1. Qiu W, Wu X, Shi H, et al. ASF1B: a possible prognostic marker, therapeutic target, and predictor of immunotherapy in male thyroid carcinoma. Front Oncol. 2022;12:678025. doi:10.3389/fonc.2022.678025
2. Petroianu A. Single supraclavicular transverse incision for radical neck dissections. Chirurgia. 2019;114(1):103–108. doi:10.21614/chirurgia.114.1.103
3. Zhang Z, Sun B, Ouyang H, Cong R, Xia F, Li X. Endoscopic lateral neck dissection: a new frontier in endoscopic thyroid surgery. Front Endocrinol. 2021;12:796984. doi:10.3389/fendo.2021.796984
4. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996;83(6):875. doi:10.1002/bjs.1800830656
5. Miccoli P, Pinchera A, Cecchini G, et al. Minimally invasive, video-assisted parathyroid surgery for primary hyperparathyroidism. J Endocrinol Invest. 1997;20(7):429–430. doi:10.1007/BF03347996
6. Zheng CM, Xu JJ, Jiang LH, Ge MH. Endoscopic thyroid lobectomy by a gasless unilateral axillary approach: Ge & Zheng’s seven-step method. Chin J General Surg. 2019;28(11):1336–1341.
7. Qin JW, Zhang ST. Thoughts on enacting and carrying out for reoperative procedures in thyroid surgery. Zhonghua Wai Ke Za Zhi. 2017;55(8):579–581. doi:10.3760/cma.j.issn.0529-5815.2017.08.005
8. Chen XD, Peng B, Gong RX, Wang L, Liao B, Li CL. Endoscopic thyroidectomy: an evidence-based research on feasibility, safety and clinical effectiveness. Chin Med J. 2008;121(20):2088–2094. doi:10.1097/00029330-200810020-00027
9. Gao M, Ge M, Ji Q, et al. 2016 Chinese expert consensus and guidelines for the diagnosis and treatment of papillary thyroid microcarcinoma. Cancer Biol Med. 2017;14(3):203–211. doi:10.20892/j.issn.2095-3941.2017.0051
10. Kalemera Ssenyondo E, Fualal J, Jombwe J, Galukande M. To drain or not to drain after thyroid surgery: a randomized controlled trial at a tertiary hospital in East Africa. Afr Health Sci. 2013;13(3):748–755. doi:10.4314/ahs.v13i3.33
11. Ma X, Xia QJ, Li G, Wang TX, Li Q. Aesthetic principles access thyroidectomy produces the best cosmetic outcomes as assessed using the patient and observer scar assessment scale. BMC Cancer. 2017;17(1):654. doi:10.1186/s12885-017-3645-2
12. Hüscher CS, Chiodini S, Napolitano C, Recher A, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc. 1997;11(8):877. doi:10.1007/s004649900476
13. Alramadhan M, Choe JH, Lee JH, Kim JH, Kim JS. Propensity score-matched analysis of the endoscopic bilateral axillo-breast approach (BABA) versus conventional open thyroidectomy in patients with benign or intermediate fine-needle aspiration cytology results, a retrospective study. Int J Surg. 2017;48:9–15. doi:10.1016/j.ijsu.2017.09.077
14. Miccoli P, Berti P, Frustaci GL, Ambrosini CE, Materazzi G. Video-assisted thyroidectomy: indications and results. Langenbecks Arch Surg. 2006;391(2):68–71. doi:10.1007/s00423-006-0027-7
15. Lombardi CP, Raffaelli M, Princi P, De Crea C, Bellantone R. Video-assisted thyroidectomy: report of a 7-year experience in Rome. Langenbecks Arch Surg. 2006;391(3):174–177. doi:10.1007/s00423-006-0023-y
16. Conzo G, Calò PG, Gambardella C, et al. Controversies in the surgical management of thyroid follicular neoplasms. Retrospective analysis of 721 patients. Int J Surg. 2014;12(Suppl 1):S29–34. PMID: 24859409. doi:10.1016/j.ijsu.2014.05.013
17. Tan Y, Guo B, Deng X, et al. Transoral endoscopic selective lateral neck dissection for papillary thyroid carcinoma: a pilot study. Surg Endosc. 2020;34(12):5274–5282. doi:10.1007/s00464-019-07314-8
18. He Q, Zhu J, Zhuang D, et al. Robotic lateral cervical lymph node dissection via bilateral axillo-breast approach for papillary thyroid carcinoma: a single-center experience of 260 cases. J Robot Surg. 2020;14(2):317–323. doi:10.1007/s11701-019-00986-3
19. Gambardella C, Patrone R, Di Capua F, et al. The role of prophylactic central compartment lymph node dissection in elderly patients with differentiated thyroid cancer: a multicentric study. BMC Surg. 2019;18(Suppl 1):110. PMID: 31074400; PMCID: PMC7402571. doi:10.1186/s12893-018-0433-0
20. Yu ST, Ge JN, Sun BH, et al. Lymph node yield in the initial central neck dissection (CND) associated with the risk of recurrence in papillary thyroid cancer: a reoperative CND cohort study. Oral Oncol. 2021;123:105567. doi:10.1016/j.oraloncology.2021.105567
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

