Back to Journals » OncoTargets and Therapy » Volume 10
Therapeutic value of 3-D printing template-assisted 125I-seed implantation in the treatment of malignant liver tumors
Authors Han T , Yang X, Xu Y, Zheng Z, Yan Y, Wang N
Received 9 February 2017
Accepted for publication 26 May 2017
Published 3 July 2017 Volume 2017:10 Pages 3277—3283
DOI https://doi.org/10.2147/OTT.S134290
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Carlos E Vigil
Tao Han,1,* Xiaodan Yang,1,* Ying Xu,2,* Zhendong Zheng,1,* Ying Yan,2 Ning Wang2
1Department of Oncology, 2Department of Radiotherapy, General Hospital of Shenyang Military Region, Shenyang, China
*These authors contributed equally to this work
Objective: To explore the therapeutic value of 3-D printing template-assisted 125I-seed implantation in the treatment of malignant liver tumors.
Materials and methods: Fifteen liver cancer patients with 47 total lesions were treated with 3-D printing template-assisted radioactive seed implantation (group A), and 25 liver-tumor patients with 66 total lesions were treated with 125I-seed implantation without a template auxiliary (group B). Operation time, in-hospital time, operation complications, dose distribution, and response rate (number) were compared between the two groups.
Results: Shorter operation times and better dose distribution were observed in group A than in group B, and the differences were statistically significant. The response rate after 2 months was 86.7% (13 of 15) in group A and 84% (21 of 25) in group B; differences between the two groups were not significant.
Conclusion: Application of 3-D printing template-assisted radioactive seed implantation in the treatment of malignant liver tumors can help shorten operation time and optimize radiation-dose distribution, is worthy of further study, and has clinical significance.
Keywords: brachytherapy, stereotactic techniques, iodine isotopes, liver, carcinoma
Background
Malignant liver tumors include primary and metastatic malignant tumors. In recent years, 125I-seed implantation has been found to show very good therapeutic effects on malignant liver tumors.1 However, this treatment is always obscured by the costa and lung tissue, and displacement of the liver caused by breathing also makes treatment difficult. The use of 3-D printing template-assisted radioactive seed implantation could solve these problems and shorten operation time by optimizing radiation-dose distribution.2,3
Materials and methods
Ethics statement
All patients in this study underwent treatment at the General Hospital of Shenyang Military Region (Shenyang, China). All clinical operations and investigations were approved by the ethical committee of the General Hospital of Shenyang Military Region, and all patients submitted signed consent forms.
General
All patients who were chosen in our ward were treated from July 2014 to March 2016. Fifteen liver-tumor patients were treated with 3-D printing template-assisted radioactive seed implantation (group A), and 25 liver-tumor patients were treated with 125I-seed implantation without an auxiliary template as the control (group B) (Table 1). Inclusion criteria were a definite diagnosis of primary liver cancer, bile-duct carcinoma, or metastatic malignant liver tumor, good general condition (Karnofsky performance status >60, liver function grade A or B), and having undergone chest radiography, electrocardiography, abdominal computed tomography (CT), and other laboratory examinations before treatment. A total of 24 patients from groups A and B had metastatic tumors, 21 patients accepted chemotherapy, and three patients accepted targeted therapy.
  | Table 1 General characteristics of the patients |
Instrumentation and equipment
Materials used were a Philips MX 4000 dual-type CT scanner, 3-D printing template, 1122-type photosensitive resin, treatment-planning system (TPS) for brachytherapy (Prowess Panther Brachy version 5.0). Seed-implant devices used were puncture needles (18 and 21 G), a wheel disk-implant gun, and radioactive seeds (type 6711-99, particle activity 0.8 mCi, energy 27–35 keV, half-life 59.4 days). All particles were tested for activity before delivery, and notes were taken.
Therapeutic method
Preoperative plan and 3-D template printing
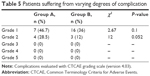
3-D printing is based on data design files, the material deposited layer by layer to form a three-dimensional object.4 The flexibility of 3-D printing allows investigators and manufacturers to create medical devices with a broad range of biological and physical properties. When paired with medical imaging, this flexibility may be leveraged to fabricate devices tailored to an individual patient’s anatomy, such as a 3-D template. We can use the 3-D template to complete the example of implantation accurately, including outlining the target area, simulating the needle path, simulating the spatial position of the particle cloth, calculating the number of particles, and generating templates.5 For group A, according to the nidus, a supine or prone position was chosen. Next, three hemispherical plastic tags of 0.7 cm were set near the operative area. CT scans were performed using 5 mm-thick lines, and included the whole liver and the position-mark point. The result was converted to the DICOM (digital imaging and communications in medicine) format and transferred to the TPS system. The target region was delineated, and the prescription dose was set at 12,000 cGy. Next, insertion of the pin was simulated, and then the pin and particle positions were adjusted so that the dose conformed to the following conditions: minimal periphery dose = prescription dose; D90 > maximum permissible dose; V100 >95%. After completing the preoperative plan, it was applied to the 3-D printing system to print the templates and order the particles. For group B, all procedures were performed as those in group A, except for application of the 3-D printing system and print templates (Figure 1).
  | Figure 1 Use of TPS to design the needle-insert and seed-arrangement plane according to CT result for printing 3-D templates. |
Software algorithm
Stereolithography (STL) files were loaded in Materialise Magics version 9.51 software to select the regions of interest. Anatomical structures (bile ducts, hepatic arteries, hepatic veins, and portal veins) were digitally segmented with MeVis-supplied (MeVis Medical Solutions AG, Bremen, Germany) digital files from the optimal visualization phases of contrast-enhanced CT and magnetic resonance imaging (MRI). Subsequently, the geometry of each structure was exported to a mesh-type (STL) file to create a 3-D geometry of that structure. Digital preparation of the STL files was accomplished with the Magics software.
Therapeutic process
The template should be placed according to the positioning mark, and a 21 G puncture needle can be used to administer local anesthesia. At this time, the patient should not breathe, an 18 G puncture needle should be used to insert the needle, and then the position should be checked by CT. If the needle is confirmed to be correctly positioned, then another two places are chosen to insert the needles in a similar way. If this did not conform to the plan, the patient should be instructed to breathe, and the puncture can be repeated until the position of the needle conforms to the plan. With three needles fixed to the template and liver, 18 G needles can be inserted according to the template, guided under local anesthesia, and the positions should be rechecked by CT to ensure that all of the needles are placed correctly and that the seeds were placed according to the plan. The needle can then be retreated gently. If bleeding occurs, the patient’s own hemocoagulase can be used to stop the bleeding. The entire therapy should be performed with electrocardiography monitoring, and rescue supplies should be prepared.
Postoperative validation
CT was performed immediately after seed implantation, using all conditions as described. The result was converted to the DICOM format and transferred to the TPS system to be verified postoperatively. The receiver postoperative isodose curve, dose-volume histogram, and other parameters were evaluated (Figure 2).
  | Figure 2 Preoperative planning and postoperative quality authentication. |
Therapeutic evaluation and side effects observed and followed
All patients who accepted radioactive particle-implantation treatment were rechecked with CT or MRI after 1, 2, and 3 months. Nidus size was compared with that determined 2 months previously. The largest diameter of the tumor was measured, all nidus diameters were added, and then statistical analysis was performed. According to Response Evaluation Criteria in Solid Tumors 1.1, complete response (CR), partial response (PR), no change, and progressive disease were determined:
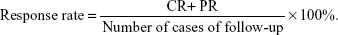
|
Statistical methods
Two groups of data were subjected to χ2 test, and measurement data were evaluated using t-tests and SPSS 19.0. P<0.05 indicated statistical significance.
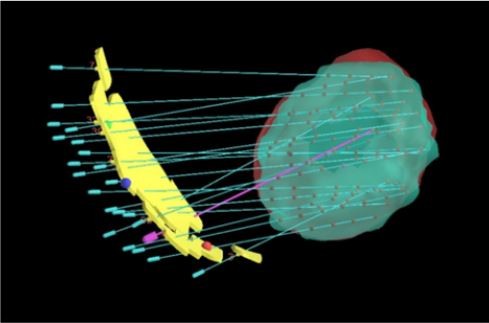
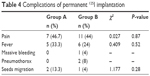
Results
All patients in the two groups underwent radioactive particle-implantation treatment successfully (Table 2). Compared with group B, duration in group A was shorter, D100 and V100 were closer to the prescribed dose, V150 was smaller, and the dose distribution was more precise. Differences between the groups showed statistical significance. Efficacy comparison of the two groups is shown in Table 3, and differences between the groups showed no statistical significance. Complication comparison is shown in Tables 4 and 5.
  | Table 2 Operation data |
  | Table 3 Response (rate) results, n (%) |
  | Table 4 Complications of permanent 125I implantation |
Discussion
Radioactive particle implantation has the characteristics of a small trauma operation, providing a high treatment dose in the tumor target area and only minor injury to normal tissue. In recent years, radioactive particle-implantation treatment has increasingly been used in solid malignant tumors and other treatments and achieved good therapeutic effect.6,7 Peng et al8 reported transarterial chemoembolization (TACE) combined with 125I particles in the treatment of 32 cases of primary liver cancer and TACE alone in a group of 43 patients. Results of the control group and combined-treatment group were 60.5% (26 of 43) and 84.4% (27 of 32), respectively, and the difference was significant (P<0.05). Median survival times were 19.5 and 22.9 months, respectively, and the difference was significant (P<0.05). Therefore, TACE combined with 125I particles in the treatment of primary liver cancer is safe and effective. Zhang et al reported CT-guided 125I seed implantation in the treatment of liver cancer recurrence after liver transplantation and extrahepatic metastases. The matched peripheral dose was 100–150 Gy, and the total effectiveness rate was 82.2%. The main complications were pneumothorax, a small amount of bleeding, a small shift in white blood-cell count, and a slight reduction in the number of white blood cells. For treatment of liver cancer recurrence and metastasis of liver tumors after liver transplantation, 125I seeds implanted under CT guidance are effective, less invasive, and cause fewer complications.9 Because the liver puncture is often blocked by the ribs, respiratory movement, tumor-infiltration range, and irregular shape, as well as other factors, it is often difficult to implement preoperative planning accurately, resulting in poor dose distribution at the tumor lesion, which affects tumor treatment, the ability to control the quality of the treatment technology, and universal standardization of the treatment plan.
Computer-aided design of the 3-D printing template can accurately map the preplanned information of the needle track to the individual template to achieve precise implementation of the treatment plan and optimize dose distribution within the target area. The use of 3-D printing of individual templates also allows the treatment process to be simple and effective, allows the continuous treatment of multiple lesions, shortens operation time, and improves patient tolerance. Zhang et al reported CT guidance combined with the use of the 3D printing template to guide the implantation of radioactive particles in the treatment of recurrent retroperitoneal tumor success.9 Huang et al10 reported the use of 3-D printing template CT-guided 125I implantation in 31 patients with head and neck cancer recurrence and locally advanced cancer patients, and D90, V100, and V150 achieved the treatment requirements, revealing that individual 3-D printing templates can make radioactive particle-implantation treatment simpler and more accurate.
Liver puncture is affected by breathing; therefore, our approach is to ask patients with shallow breathing in the inspiratory phase to hold their breath for 2 seconds, and a scan is used to position the needle; not only can patients maintain a sufficiently long breath hold to exclude gas time but this technique can also reduce pain caused by inspiratory changes in patients with aspiration that would impact the puncture. Scanning during the puncture (after deep inspiration) is performed to verify this method of holding the breath; the result is more accurate and easy to confirm. If the needle is found to be deviated from the predetermined position during scanning, it can be retracted to the subcutaneous adjustment direction and then used for repuncture until the predetermined position is reached. Usually, the first needle is the most difficult to achieve puncture, and subsequent needle puncture is relatively easy. The location of tumor foci is relatively fixed; therefore, puncture of the needle path through sensitive areas, such as the gallbladder, portal vein, hepatic vein, and near the top of the diaphragm, can be avoided by using the scan to verify the needle is positioned in the desired location. The remaining puncture needle can be positioned using the preset template position.
Lesions around the top of the phrenic nerve are always sheltered from the diaphragm and lung tissue and also affected by respiratory movement. Because of the requirement of location, we needed to puncture many times, possibly leading to bleeding, pneumothorax, hemopneumothorax, and other side effects. A 3-D printing template has accurate space-orientation function.11 Fifteen liver-tumor patients with 47 total lesions were treated with 3-D printing template-assisted radioactive seed implantation, and operation time was significantly shortened compared with the control group.
After particle implantation, verification of quality confirmed that D100, V100, and V150 had statistically significant differences between the groups. The template-assisted group’s matched peripheral dose was improved, target-zone high-dose area was smaller, and dose distribution conformed more closely to preoperative planning. The template-assisted group had a higher effective rate than the control group, but with no statistical significance, which may have been due to the low number of cases in this study.
Regarding complications, one patient in the control group exhibited hemothorax. After hemostasis, fluid infusion, blood transfusion, and other symptomatic treatment, the bleeding was stopped. Two months later, the pleural fluid was completely absorbed. Patients with lesions located under the diaphragm underwent cryoablation. The puncture position was close to the original puncture point. Vascular elasticity was decreased, implying that any hemorrhage might have been due to perivascular tissue organization. Another two patients with lesions located under the diaphragm in the control group developed pneumothorax caused by coplanar puncture damage to pleura and lung tissue. Prompt application of the 3-D printing template assisted by noncoplanar puncture can reduce diaphragmatic-targeted biopsy complications.
The results of this study suggest that 3-D printing template-assisted 125I-seed implantation in the treatment of malignant liver tumors can reduce operation time, optimize radiation-dose distribution, and show satisfactory results. However, because of the retrospective nature of the study, which included a small number of patients, some bias effects exist, such as patient compliance. In future, large-scale prospective randomized studies are needed to validate the clinical value of 3-D printing template-assisted 125I-seed implantation in treatment.
Acknowledgment
This work was supported by grants from the Postdoctoral Science Foundation of China (No 2015M582822) and the Doctor Scientific Research Foundation of Liaoning Province (No 201501022). No additional external funding received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Qian JA, Bao ZH, Zou J, Yang HL. Effect of pedicle fixation combined with 125I seed implantation for metastatic thoracolumbar tumors. J Pain Res. 2016;9:271–278. | ||
Huang ZM, Pan CC, Wu PH, et al. Efficacy of minimally invasive therapies on unresectable pancreatic cancer. Chin J Cancer. 2013;32:334–341. | ||
Zhang JP, Yu LP. Preparation of three-dimensional ordered macroporous Cu2O film through photonic crystal template-assisted electrodeposition method. J Mater Sci. 2014;25:5646–5651. | ||
Gerstle TL, Ibrahim AM, Kim PS, Lee BT, Lin SJ. A plastic surgery application in evolution: three-dimensional printing. Plast Reconstr Surg. 2014;133:446–451. | ||
Michalski MH, Ross JS. The shape of things to come: 3D printing in medicine. JAMA. 2014;312:2213–2214. | ||
Cao ZZ, Yang HY, Dou P, Wang C, Zheng J, Xu XH. Synthesis of three-dimensional hollow SnO2@PPy nanotube arrays via template-assisted method and chemical vapor-phase polymerization as high performance anodes for lithium-ion batteries. Electrochim Acta. 2016;209:700–708. | ||
Wang S, Shi G, Meng X. Clinical curative effect of percutaneous vertebroplasty combined with 125I-seed implantation in treating spinal metastatic tumor. Pak J Pharm Sci. 2015;28:1039–1042. | ||
Peng S, Yang QX, Zhang T, et al. Lobaplatin-TACE combined with radioactive 125I seed implantation for treatment of primary hepatocellular carcinoma. Asian Pac J Cancer Prev. 2014;15:5155–5160. | ||
Zhang FJ, Li CX, Wu PH, et al. [Radioactive seed 125I implantation in treating recurrence and metastasis after liver transplantation in hepatoma]. Zhonghua Yi Xue Za Zhi. 2007;87:956–959. Chinese. | ||
Huang MW, Liu SM, Zheng L, et al. A digital model individual template and CT-guided 125I seed implants for malignant tumors of the head and neck. J Radiat Res. 2012;53:973–977. | ||
Ji Z, Jiang Y, Guo F, et al. Dosimetry verification of radioactive seed implantation for malignant tumors assisted by 3D printing individual templates and CT guidance. Appl Radiat Isot. 2017;124:68–74. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.