Back to Journals » Clinical Interventions in Aging » Volume 9
The use of potentially inappropriate medications and changes in quality of life among older nursing home residents
Authors Al Aqqad S, Chen LL, Shafie A , Hassali MA, Tangiisuran B
Received 1 August 2013
Accepted for publication 21 November 2013
Published 22 January 2014 Volume 2014:9 Pages 201—207
DOI https://doi.org/10.2147/CIA.S52356
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Sana’ MH Al Aqqad, Li Li Chen, Asrul Akmal Shafie, Mohamed Azmi Hassali, Balamurugan Tangiisuran
Pharmacy Practice Research Group, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia
Background: Nursing home residents are mainly older people with multiple diseases and taking multiple medications. The quality use of medication and its association with health related quality of life (HRQoL) have not been reported in Malaysia. This study aims to investigate the association between the use of potentially inappropriate medications (PIMs) and the changes observed in the HRQoL among older nursing home residents.
Methods: A prospective follow up study was conducted at four nongovernmental organization nursing homes in Penang, Malaysia. Older residents (≥65 years old) taking at least one prescribed medication were included. Residents with PIMs were identified by using Screening Tool of Older Person's potentially inappropriate Prescriptions (STOPP) criteria. HRQoL was assessed using EuroQol-5 dimension (EQ-5D) and EuroQol-visual analog scale (EQ-VAS) at baseline and after a 3-month follow up. The association of PIMs with HRQoL was analyzed using Mann-Whitney U test.
Results: The median age of the 211 participants was 77 years (interquartile range 72–82 years) and the median number of prescription medicines was four (interquartile range three to six). The prevalence of PIMs was 23.7% and 18.6% at baseline and 3 months later, respectively. The most commonly prescribed PIMs in decreasing order were first generation antihistamine, prescriptions of duplicate drug class, glibenclamide with type 2 diabetes mellitus, and anticholinergic to treat extrapyramidal side effects of neuroleptic medications. At baseline, there was no significant difference among residents with or without PIMs in each bracket of EQ-5D, EQ-5D index, or EQ-VAS scores. Comparison of the differences in the mean score index of EQ-5D between baseline and after 3 months also showed no statistically significant differences.
Conclusion: PIMs were found to be relatively common among older nursing home residents. However, no significant changes were observed in HRQoL among these residents. Further studies with a bigger sample size and longer follow up period are required to establish this association.
Keywords: elderly, health related quality of life, patient safety
Introduction
Aging has become an emerging health problem and is considered the most challenging health issue worldwide. Advances in technologies and the development of new medicines have contributed longer life expectancy. It has been reported that 90% of the older population in the US have been using at least one medication.1 The complex process of aging, which causes changes in physiological function, can affect the pharmacodynamics and pharmacokinetics of the medication taken by older populations.2 In addition, the use of multiple medications due to multiple comorbid conditions may also lead to the use of potentially inappropriate medications (PIMs), which place medication users at higher risk for adverse drug reaction.
PIM has been defined as the use of medication with risk greater than benefit, inappropriate dosing duration, prescriptions that lead to clinically significant drug–drug and drug–disease interactions, and the under-use of potentially beneficial medications.3 PIMs among the older population have continued to be a significant problem worldwide.4,5 This scenario is particularly common among nursing home residents due to the high prevalence of frailty, multiple comorbidities, and functional limitations.16 PIMs have been reported to be common among the elderly with a prevalence of 40%–50% among nursing home residents7,8 and 19%–28% among community dwelling patients.7,9,10
In Malaysia, the number of institutions for the elderly is increasing. There are few residential homes and long-term care facilities that are fully funded by the government. The majority of nursing homes are operated by private sector and nongovernmental organizations with some financial support from the government. There are no dedicated physicians and/or pharmacists working in the nursing homes to provide continuous medical care. Also, routine medication review processes are not being conducted in nursing homes in Malaysia as they are in other developed countries. The residents are sent to either government hospitals or primary health care clinics for medical treatment. Patients with chronic diseases are under regular monitoring in specialized clinics in hospitals.
Health related quality of life (HRQoL) is now considered as an essential outcome measure for assessing the effectiveness of medical intervention. A study, which was conducted using the database from the 1996 Medical Expenditure Panel Survey, has shown that PIM is a predictor for and is associated with poor patient HRQoL.11 Recent studies have shown a significant improvement in HRQoL among patients who are taking safer and more appropriate drugs.12,13 From the local perspective, there is only one study that has been recently published on PIMs use among older populations.14 The prevalence of PIMs use among nursing home residents was reported to be high at 32.7% using Beers criteria.14 However, no data have been reported focusing on the changes of HRQoL among older people prescribed with PIMs. Hence, the current study aims to investigate the association between the use of PIMs and the changes observed in the HRQoL among older nursing home residents.
Materials and methods
Study design and setting
A prospective follow-up study was conducted at four nongovernmental nursing homes in Penang, Malaysia.
The study was divided into two phases. In Phase I of the study, the baseline data from all the nursing homes were collected over a 2 month period from January 2011 through February 2011. Each recruited patient from Phase I of the study was followed up after a 3 month period (Phase II). The PIMs and HRQoL were reassessed after a period of 3 months. All residents of 65 years of age or over with nursing home stay for at least 3 consecutive months and who were taking at least one prescribed medication for 7 days prior to the recruitment were included in the study. The exclusion criteria were residents with medical diagnoses of dementia (or those taking antidementia drugs), those who refused to participate in the study, or those who were unable to participate in the study due to delirium or were unable to respond, communicate, and present with complete cognitive and functional disability.
The demographic, clinical, and medications data of residents were collected using medical records review and interviews of residents where necessary. Functional status for residents was assessed using Katz activities of daily living.15 This scale reflects dependence in six primary functions, ie, bathing, dressing, toileting, continence, walking, and eating. The scores of this scale ranges from 0 (independence) to 6 (high dependency).
The cognitive status
The cognitive function of the residents was screened using the Mini-Cog exam,16 which is a tool comprising three-item recall and the clock drawing test (CDT) with sensitivity ranging from 76%–99%, and specificity ranging from 89%–93%. Patients who fail to recall all three items after the CDT distractor are classified as possibly demented. The residents who are able to recall one or two of the items are classified based on the CDT. An abnormal CDT equates with possibly demented and a normal CDT is considered normal and equates with non-demented. The Mini-Cog was developed as a screening tool to identify patients with possible dementia. The Mini-Cog tool was not used as an exclusion tool in this study.
Health related quality of life
All residents who fulfill the inclusion criteria were assessed at baseline for HRQoL using the EuroQoL tool, which comprised of EuroQol-5 dimension (EQ-5D) and EuroQol-visual analog scale (EQ-VAS).17 The first part is considered a descriptive system that is used to evaluate health function in 5 dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). The results were classified based on the scoring system categorized as: no problem (score 1); some problem (score 2); and extreme problem (score 3). In addition, the results can be identified for each domain separately. Moreover, the EuroQol index is a single weighted health index, which was converted from 243 possible combinations of health states by applying the weights from the York tariffs.18 Values of the EuroQol index can range from −0.594 to 1 and a negative index score implies a quality of life worse than death.
The second part is a self-administered EQ-VAS used to evaluate current and general health status. The residents were asked to assess their health status by drawing a line from a box that represents “your health status today” to a point on EQ-VAS that represents heath status. A score of 100 indicates the best health status, while a score of zero indicates the worst health status.17 Permission was obtained from the EuroQoL group to use both the English and Malay versions of the EQ-5D. Both versions have been validated for use among Malaysian populations.19
Potentially inappropriate medications
PIMs use in this population was assessed using the Screening Tool of Older Person’s potentially inappropriate Prescriptions (STOPP) criteria20,21 at baseline and after a period of 3 months. Residents’ medications in the last 7 days prior to interview were assessed for the identification of PIMs. STOPP is a tool used to identify PIMs and potential adverse drug reactions among older people. It consists of 65 clinically significant criteria for PIM. For the convenient use of the criteria, arrangements of medications are carried out according to relevant physiological systems. Inter-rater reliability of STOPP criteria is good, with a kappa coefficient of 0.75.20
Statistical analysis
The comparison of the differences in the baseline variables between the PIM and non-PIM group was conducted using Student’s t-test for normally distributed data, Pearson’s chi-squared test was used for categorical data, and Mann-Whitney U-test was used for non-normally distributed data. Unpaired t-test was used to measure the change in the quality of life ([QOL] ΔQOL = QOLs after 3 months minus baseline QOLs) between the PIM group and non-PIM group, and to evaluate whether PIMs affected individual baseline of QOLs during the 3 month follow-up. In addition, chi-square test was used to compare the changes of PIMs at baseline and 3 months later. The data were analyzed using PASW® (Predictive Analytics SoftWare) Statistics 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics approval
This study was approved by the local ethics committee (Medical Research and Ethics Committee [MREC], Ministry of Health, Malaysia), and carried out in accordance with the Declaration of Helsinki.
Results
Of the total population (n=460) residing in four nursing homes, 211 (45.7%) residents were included in the study. The remaining 249 residents were excluded for the following reasons: residents not able to participate due to delirium or unable to respond to interview questions [n=91], <65 years old (n=11), not taking any prescribed medications (n=77), less than 3 month stay in a nursing home (n=2), diagnosis of dementia (n=32), and those who refused to participate (n=36). During the follow up period (Phase II), 12 residents were excluded from this study for reasons such as leaving home or on holiday (n=5), hospitalized due to fall and vascular ulcer (n=2), not able to participate (n=2), and death (n=3).
The baseline characteristics of the study subjects are listed in Table 1. The median age is 77 years (interquartile range 72–82 years). The study’s participants were mainly females (60.7%). The most common comorbidities among participants were hypertension (71.1%) followed by diabetes mellitus (27.1%), stroke (12.3%), osteoarthritis (11.8%), and ischemic heart disease (7.1%). The median number of medications prescribed was four (range of one to 14) from a total of 989 medications.
  | Table 1 The characteristics of residents included in the study |
The prevalence of PIMs identified by STOPP criteria at baseline was 23.7%; 64 PIMs affecting 50 residents. Eleven residents (5.2%) were taking more than one PIM. The most common PIMs detected were first generation antihistamine (23.4%), followed by prescriptions of duplicate drug class (including two angiotensin receptor blockers, two first generation antihistamines, and alpha-2 blockers) (15.6%), glibenclamide or chlorpropamide with type 2 diabetes mellitus (10.9%), and anticholinergic to treat extrapyramidal side effects of neuroleptic medications (9.4%). Other less common medications were prolonged use (>1 week) of first generation antihistamines (7.8%), benzodiazepines (4.7%), and neuroleptics (1.7%) as shown in Table 2. Reassessment of PIMs after 3 months showed that there was a decrease in the prevalence of PIMs to a prevalence of 18.6%, affecting 37 residents. The prevalence of residents who were still taking PIMs was 15.2% (n=32), while 7.1% (15) of the residents stopped taking PIMs. However, 2.4% (n=5) of residents had added PIMs. The number of prescribed medications in Phase II decreased from 989 at baseline to 911.
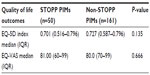
Pearson’s chi-squared test analysis was used to assess the association between PIMs with the 5 dimensions of EQ-5D at baseline. Results showed that there were no significant differences in all of the 5 dimensions among residents with and without STOPP PIMs (Table 3). Similar findings were found for both EQ-5D index and EQ-VAS. Table 4 shows that there were no significant differences in HRQoL measured by EQ-5D index (P=0.135) and by EQ-VAS (P=0.666) among residents with and without PIMs.
The changes in HRQoL among residents with PIMs were assessed by comparing differences in the mean score index of EQ-5D and EQ-VAS between baseline and the 3 months follow-up period. No significant differences were seen in EQ-5D score (P=0.07) and EQ-VAS score (P=0.34) among residents with STOPP PIMs and without STOPP PIMs (Table 5).
Discussion
Several published studies have in fact reported the relationship between HRQoL and the use of PIMs.11,12,22,23 All of these studies were conducted in either hospitals or ambulatory care settings, but none of them focused on a nursing home setting in Malaysia, in particular. This study shows that the rate of PIMs was lower (23.7%) compared to other studies. A study that was conducted across different health care settings using STOPP criteria in Spain reported higher prevalence; 36% in a public primary clinic, 54% a in hospital geriatric clinic, and 50% in assisted nursing homes.24 Different prescribing practices tailored to local health care systems and the number of medications may explain the variations observed. The number of prescriptions has been identified as a significant predictor of inappropriate use of medications and HRQoL.23,25 The population of this study was taking a median of four medications, which is slightly lower compared to the ones taken in the developed countries. For example, in an Australian study, the average number of medications utilized by elderly residents was seven.26 Hence, the low rate of medication use may contribute to the lower rate of PIMs observed.
During the follow-up phase, lower prevalence of PIMs was observed in this study compared to baseline (18.6% versus 23.7%, respectively). This could be due to the decrease in the utilization of prescribed medications during the follow-up phase. First generation antihistamine was still identified as the most common prescribed PIM although it was the most common stopped PIM during the 3 month follow-up. A decrease of PIMs cases classified as drug duplications was noticed. PIMs due to glibenclamide prescriptions with type 2 diabetes mellitus remained the same in terms of numbers (seven cases) although the percentage was higher in Phase II than at baseline (17.1% versus 10.9%, respectively).
The main result of this study showed no statistically significant association between PIMs and HRQoL. PIMs showed no statistical significant differences based on any EQ-5D descriptive system and EQ-VAS score at baseline and after 3 months. The HRQoL was comparable among residents with and without PIMs. On average, the EQ-5D and EQ-VAS score was above 0.60 and 70, respectively. In a study conducted among older community dwellers, a higher EQ-5D index (0.7) was reported compared to the current study, but a similar EQ-VAS score was reported.23 The discrepancy could be due to better health status of their study population, which consists of a general population of noninstitutionalized individuals compared to a nursing home population in the present study. However, the same EQ-VAS value can be due to individual perception of the current residents’ health status in this study, which was largely influenced by many factors including better self-acceptance of health conditions among nursing home residents.
Another study by Olsson et al examined the association between medication qualities measured by the medication appropriateness index and HRQoL measured by the EQ-5D in a group of elderly people discharged from hospitals.12 Their study population achieved a lower score compared to this study; mean EQ-5D <0.5 and mean EQ-VAS <60. Hospitalized patients would have slightly lower HRQoL because they were admitted for acute medical conditions and may have loss of activities of daily living during the recuperation period. One study has shown that hospitalizations were associated with functional decline among elderly patients.27 Consequently, these may have lowered the EQ-5D measurement on HRQoL.
Although the majority of the studies do not show any significant difference or a relationship between PIMs and HRQoL,22,23 one study, which employed one question on global self-rated health status, showed a significant decrease in self-perceived health status in the elderly.11 This result was mainly attributed to the tool used for the outcome measurement. Although the method utilized may contribute for estimation bias, it was reported that the tool was widely used with proven predictive validity and substantial reliability in epidemiological research.11
One group of researchers suggested that the use of the disease-specific HRQoL scale might provide more specific and receptive results for the measurement of the impact of PIMs towards patient’s HRQoL.23 Such argument was on the basis that generic quality of life measures may not be sensitive to nonsevere illnesses. However, there are no data from the literature to support this statement. The use of EQ-5D to assess HRQoL is considered as a point of strength in this study. It is a standardized measure of health status developed by the EuroQol Group that is applicable to a wide range of health conditions and treatments with a simple descriptive profile and a single index value for health status. It is cognitively undemanding, taking only a few minutes to complete. Wolfs et al showed that the EQ-5D is well suited for evaluating HRQoL among population with cognitive impairment.28 In a recent study, EQ-5D was found to be user friendly and a potential predictor of mortality and first hospitalization among the elderly.29 Although regional variation in term valuations or weightings may contribute to different outcomes, it should not be considered as a major limitation. The author adopted the EQ-5D index derived from the UK population due to unavailability of local term valuation. The application of the valuations among a Malaysian population may differ due to dissimilar sociodemographic characteristics and cultural perceptions towards health status.
The strength of this study lies in the high reliability for all assessments as they were conducted only by one researcher. All interviews were conducted in English, Malay, or, when necessary, with the most appropriate dialect with an assigned interpreter. The researcher followed a script that was used to ensure consistency when assessing the residents.
Although the study was conducted using a robust method, there are several limitations that are worth mentioning here. First, small sample size may have contributed to the result observed in the HRQoL. The current findings could not be generalized to the entire Malaysian elderly population due to the special population group limited to nursing homes. Although this study was a multicenter study, it focused on one state only in Northern Malaysia. Second, the lower prevalence of PIMs identified could be due to under reporting due to older residents with the diagnosis of dementia being excluded in this study; demented patients are reportedly more prone to be prescribed with PIMs.30 Third, the researchers did not perform the under-treatment assessment among the nursing homes, which can affect the rate of PIMs and the consequent change in HRQoL. Finally, inclusion of four centers may lead to variation of the PIMs rate due to different prescribing patterns from different hospitals and clinicians.
Conclusion
This study indicates that PIMs are relatively prevalent in the Malaysian nursing homes as detected by STOPP criteria. Although there were no statistically significant changes observed in terms of the HRQoL among the nursing home residents, the study does provide baseline information and challenges faced in terms of the quality use of medications. A larger study with a longer follow-up period should be conducted throughout Malaysia to give more insight into this issue. Aside from this, new policies should be implemented implicating the involvement of pharmacists to provide a routine comprehensive medication review in the nursing homes to improve medication use among the elderly.
Acknowledgments
The researchers would like to thank the nursing homes and all the respondents, who have willingly participated in this study. They also extend their due thanks to Universiti Sains Malaysia for the provision of funding under the Short Term Grant.
Disclosure
The authors report no conflicts of interest in this work.
References
Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337–344. | |
Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol. 2004;57(1):6–14. | |
Spinewine A, Schmader KE, Barber N, et al. Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet. 2007;370(9582):173–184. | |
Liu GG, Christensen DB. The continuing challenge of inappropriate prescribing in the elderly: an update of the evidence. J Am Pharm Assoc (Wash). 2002;42(6):847–857. | |
Hanlon JT, Lindblad CI, Hajjar ER, McCarthy TC. Update on drug-related problems in the elderly. Am J Geriatr Pharmacother. 2003;1(1):38–43. | |
Crystal S, Gaboda D, Lucas J, Gerhard T, Chakravarty S. Assessing medication exposures and outcomes in the frail elderly: assessing research challenges in nursing home pharmacotherapy. Med Care. 2010;48(Suppl 6):S23–S31. | |
Aparasu RR, Mort JR. Inappropriate prescribing for the elderly: beers criteria-based review. Ann Pharmacother. 2000;34(3):338–346. | |
Lau DT, Kasper JD, Potter DE, Lyles A. Potentially inappropriate medication prescriptions among elderly nursing home residents: their scope and associated resident and facility characteristics. Health Serv Res. 2004;39(5):1257–1276. | |
Fialova D, Topinkova E, Gambassi G, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293(11):1348–1358. | |
Azoulay L, Zargarzadeh A, Salahshouri Z, Oraichi D, Bérard A. Inappropriate medication prescribing in community-dwelling elderly people living in Iran. Eur J Clin Pharmacol. 2005;61(12):913–919. | |
Fu AZ, Liu GG, Christensen DB. Inappropriate medication use and health outcomes in the elderly. J Am Geriatr Soc. 2004;52(11):1934–1939. | |
Olsson IN, Runnamo R, Engfeldt P. Medication quality and quality of life in the elderly, a cohort study. Health Qual Life Outcomes. 2011;9:95. | |
Bladh L, Ottosson E, Karlsson J, Klintberg L, Wallerstedt SM. Effects of a clinical pharmacist service on health-related quality of life and prescribing of drugs: a randomised controlled trial. BMJ Qual Saf. 2011;20(9):738–746. | |
Chen LL, Tangiisuran B, Shafie AA, Hassali MA. Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int J Clin Pharm. 2012;34(4):596–603. | |
Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. | |
Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15(11):1021–1027. | |
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. | |
Dolan P, Gudex C, Kind P, Williams A. The time trade-off method: results from a general population study. Health Econ. 1996;5(2):141–154. | |
Shafie AA, Hassali MA, Liau SY. A cross-sectional validation study of EQ-5D among the Malaysian adult population. Qual Life Res. 2011;20(4):593–600. | |
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83. | |
Gallagher P, O’Mahony D. STOPP (Screening Tool of Older Persons’ potentially inappropriate Prescriptions): application to acutely ill elderly patients and comparison with Beers’ criteria. Age Ageing. 2008;37(6):673–679. | |
Holland R, Lenaghan E, Harvey I, et al. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ. 2005;330(7486):293. | |
Franic DM, Jiang JZ. Potentially inappropriate drug use and health-related quality of life in the elderly. Pharmacotherapy. 2006;26(6):768–778. | |
Conejos Miquel MD, Sánchez Cuervo M, Delgado Silveira E, et al. Potentially inappropriate drug prescription in older subjects across health care settings. Eur Geriatr Med. 2010;1:9–14. | |
Zhan C, Sangl J, Bierman AS, et al. Potentially inappropriate medication use in the community-dwelling elderly: findings from the 1996 Medical Expenditure Panel Survey. JAMA. 2001;286(22):2823–2829. | |
Stafford AC, Alswayan MS, Tenni PC. Inappropriate prescribing in older residents of Australian care homes. J Clin Pharm Ther. 2011;36(1):33–44. | |
Corsonello A, Pedone C, Lattanzio F, et al. Potentially inappropriate medications and functional decline in elderly hospitalized patients. J Am Geriatr Soc. 2009;57(6):1007–1014. | |
Wolfs CA, Dirksen CD, Kessels A, Willems D, Verhey FR, Severens JL. Performance of the EQ-5D and the EQ-5D+ C in elderly patients with cognitive impairments. Health Qual Life Outcomes. 2007;5:33. | |
Cavrini G, Broccoli S, Puccini A, Zoli M. EQ-5D as a predictor of mortality and hospitalization in elderly people. Qual Life Res. 2012;21(2):269–280. | |
Parsons C, Johnston S, Mathie E, et al. Potentially inappropriate prescribing in older people with dementia in care homes: a retrospective analysis. Drugs Aging. 2012;9(2):143–155. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.