Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
The relationship between sleep disturbance and health status in patients with COPD
Authors Ban WH, Joo H , Lim JU, Kang HH, Moon HS, Lee SH
Received 8 March 2018
Accepted for publication 9 May 2018
Published 28 June 2018 Volume 2018:13 Pages 2049—2055
DOI https://doi.org/10.2147/COPD.S167678
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Woo Ho Ban,1 Hyonsoo Joo,1 Jeong Uk Lim,1 Hyeon Hui Kang,2 Hwa Sik Moon,2 Sang Haak Lee2
1Division of Pulmonary, Critical Care and Sleep Medicine, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea; 2Division of Pulmonary, Critical Care and Sleep Medicine, Department of Internal Medicine, St Paul’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
Introduction: The detection of insomnia in patients with COPD is assumed to be significantly lower than the actual prevalence. In this study, we investigated the prevalence of insomnia and the relationship between insomnia and health status in patients with COPD using two fairly simple and straightforward questionnaires: COPD assessment test (CAT) and insomnia severity index (ISI).
Patients and methods: A cross-sectional study was conducted using data from patients undergoing treatment for COPD at St Paul’s Hospital, The Catholic University of Korea, between December 2015 and August 2016. Patients were classified into three groups according to the ISI score: a “clinical insomnia” group (ISI≥15), a “subthreshold insomnia” group (ISI 8–15), and a “non-insomnia” group (ISI<8). Clinical parameters including past medical history, pulmonary function tests, and questionnaire data were collected and analyzed.
Results: A total of 192 patients were recruited, of which 25.0% were found to have clinical insomnia (ISI≥8). Insomnia severity was related to all CAT component items except for cough, and patients with higher CAT scores generally had more severe insomnia. Logistic regression analysis revealed that CAT score was significantly associated with insomnia in these patients (odds ratio, 1.23; 95% CI, 1.13–1.34; p<0.0001). CAT score was also a significant predictor of insomnia (area under receiver operating characteristic curve, 0.779; p<0.001). The optimal predictive cutoff value was a CAT score >14, giving a sensitivity and specificity of 66.7% and 71.5%, respectively.
Conclusion: CAT score was closely related to insomnia severity in patients with COPD. The use of CAT scores to assess for the presence and severity of insomnia in these patients may allow for better detection and management and improve clinical practice.
Keywords: chronic obstructive, maintenance disorders, pulmonary disease, sleep initiation
Introduction
COPD is an inflammatory respiratory disease characterized by irreversible air flow limitation. It is predicted to become the fourth leading cause of death worldwide by the year 2030.1 Patients with COPD often have multiple comorbidities, such as cardiovascular disease and lung cancer, making their care costly and complex.2 The economic burden of COPD is, therefore, immense, costing the US ~$36 billion in 2010. This cost is expected to increase to $49.0 billion by 2020.3
Insomnia is a common and important comorbidity in patients with COPD.4 Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, waking too early, or waking feeling unrefreshed. Several studies have been conducted evaluating the clinical impact of insomnia in patients with COPD. In these patients, insomnia and related sleep disturbances were found to be associated with deterioration in overall quality of life.5 Disturbed sleep was also related to more frequent symptomatic exacerbations and worse clinical outcomes, including an increase in mortality.6
The current estimated prevalence of insomnia in patients with COPD is ~30%. This is assumed be a significant underestimate of the actual prevalence, owing to a low clinical detection rate.7 There are several proposed reasons for this low detection rate, including a lack of awareness about the impact of insomnia by both patients and clinicians and the lack of a simple and effective diagnostic tool. As such, insomnia treatment has been a neglected aspect of overall care in this patient population.
The insomnia severity index (ISI) is a brief, effective instrument to evaluate sleep disturbance8 that consists of seven self-reported items to assess the degree of sleep difficulties. It has been found to be reliable, and has been validated against several other sleep questionnaires including the Epworth sleepiness scale and the Pittsburgh sleep quality index.9 The COPD assessment test (CAT) is a simple and validated tool that measures the health status of patients with COPD.10 As with the ISI, it is self-reported, and evaluates eight aspects of health and quality of life, including respiratory symptoms, activity, confidence, and sleep. The ISI and the CAT are both widely used in routine practice.
In this study, we assessed the prevalence of insomnia and the relationship between sleep disturbance and health status in patients with COPD using ISI and CAT scores.
Patients and methods
Study population and data collection
A cross-sectional study was conducted using data from patients undergoing treatment for COPD at St Paul’s Hospital, The Catholic University of Korea, between December 2015 and August 2016. Self-reported questionnaire data were used to evaluate the relationship between insomnia and CAT scores in these patients. Patients were enrolled according to the Global Initiative for Chronic Obstructive Lung Disease criteria.11 Patients were over 40 years of age, had a smoking history of >10 pack-years, and had an obstructive pattern on pulmonary function tests, specifically, a post-bronchodilator forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) ratio (FEV1/FVC ratio) of <0.70. Exclusion criteria included the following: patients with significant comorbid lung disease caused by lung cancer, tuberculosis, interstitial lung disease, or pneumonia; patients with psychiatric comorbidities such as depression, panic disorder, alcoholism (who drink more than one bottle of soju or four bottles of beer almost daily); patients with obstructive sleep apnea; patients with active malignancy; and those with an exacerbation of COPD at the time of enrollment. In total, 192 patients were recruited and they underwent a thorough chart review. After obtaining written informed consent from all the patients, clinical information including age, sex, body mass index, comorbidities, smoking history, exacerbation history, and medication use was gathered. Pulmonary function test data were also collected, including FVC, FEV1, FEV1/FVC ratio, and diffusion capacity of the lung for carbon monoxide. Sleep quality and health status were assessed by both the ISI and the CAT. This study was approved by the Institutional Review Board Ethics Committee of St Paul’s Hospital, The Catholic University of Korea (PC16QISI0017).
Statistical analysis
Analysis of variance and the Kruskal–Wallis test were used to estimate the difference between groups for continuous variables. The Jonckheere–Terpstra test was used to assess trends in CAT scores versus insomnia severity. To compare categorical variables, the chi-squared test and the Fisher’s exact test were used. Univariate statistical analyses were used to demonstrate the relationship between insomnia and all other values. Values that were found to be significantly associated with insomnia (p<0.2) were analyzed using multivariate stepwise regression to determine significance. A receiver operating characteristic (ROC) curve was plotted to determine the most appropriate cutoff value for ISI score when attempting to detect insomnia in patients with COPD. The two-sided significance level was set at a p-value <0.05. All statistical analyses were performed using SPSS statistical software (version 21.0 Medical, IBM SPSS Statistics; IBM Corporation, Armonk, NY, USA).
Results
Insomnia prevalence and clinical characteristics of the study population
A total of 192 patients with COPD satisfied the inclusion criteria and were recruited into this study. Patients were classified into three groups based on ISI score: a clinical insomnia group (ISI≥15; n=14), a subthreshold insomnia group (ISI 8–14; n=34), and a non-insomnia group (ISI<8; n=144). The prevalence of insomnia (classified as ISI≥8) in patients with COPD was 25%. The clinical characteristics of the study population are shown in Table 1. There were no significant differences in age, sex, BMI, comorbidities, smoking history, or medication among the three groups. Post hoc analysis revealed significant differences in the prevalence of chronic bronchitis and the number of COPD exacerbations in the previous year between the clinical insomnia and the non-insomnia groups. However, pulmonary function parameters were similar among all three groups. Among patients with insomnia (ISI ≥8; n=48), only seven patients (14.8%) were receiving proper management for their condition.
CAT scores according to insomnia severity
The CAT scores of the three groups are presented in Figure 1. Total CAT scores, and all individual item scores, except for cough, tended to increase significantly with increased insomnia severity. Increased insomnia severity was particularly associated with increased total CAT scores, breathlessness, activity, and sleep items.
  | Figure 1 CAT scores according to insomnia severity. |
Insomnia frequency and severity according to COPD assessment scores
Patients were classified into three categories based on CAT scores: a low-impact group (CAT score<10), a medium impact group (CAT score 10–20), and a high-impact group (CAT>20). The frequency of insomnia increased with increasing CAT scores, and the severity of insomnia, as evaluated by the ISI score, showed a similar trend (Figure 2). The proportion of patients who had clinical or subthreshold insomnia was significantly higher in the high-impact group (p=0.029).
  | Figure 2 Frequency of insomnia according to CAT scores. |
Clinical factors associated insomnia in patients with COPD
The clinical factors associated with insomnia (ISI≥8) in patients with COPD were assessed using univariate analysis (Table 2). Total CAT score, the prevalence of chronic bronchitis, and the number of exacerbations in the previous year were found to be significantly associated with insomnia. Subsequently, a multivariate analysis was performed that included age, diabetes mellitus, chronic renal disease, CAT scores, the use of a inhaled corticosteroid/long-acting β2-agonist inhaler, a chronic bronchitis phenotype, and the number of exacerbations in the previous year. Total CAT score was the only statistically significant factor associated with insomnia in these patients (odds ratio, 1.23; 95% CI, 1.13–1.34; p<0.0001).
Predictive value of CAT for insomnia in COPD
The ability to predict insomnia in COPD patients using CAT score was found using a ROC curve (Figure 3). A model for using the CAT score to predict insomnia was found to be statistically significant (area under the ROC curve, 0.779; p<0.001). The optimal cutoff value was CAT>14. At this value, the sensitivity and specificity were 66.7% and 71.5%, respectively.
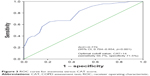  | Figure 3 ROC curve for insomnia versus CAT score. |
Discussion
COPD is a chronic inflammatory airway disease. Patients with COPD often have significant, chronic comorbidities including diabetes, cardiovascular disease, lung cancer, and psychiatric disorders.12–14 Insomnia is commonly comorbid in COPD patients and remains underdiagnosed and undertreated. The presence of insomnia, and its severity, is often underappreciated by both clinicians and patients due to both a lack of awareness and the inconvenience of objective measurement and diagnosis.
In this study, we attempted to detect insomnia in patients with COPD using ISI and CAT scores, both of which are widely used in clinical practice and fairly simple to administer. The ISI is a brief, validated questionnaire designed to assess the nature and severity of insomnia in adults. The reported prevalence of insomnia in COPD patients varies between studies, ranging from 27% to 44%.5,7 Using ISI score, our study estimated that the prevalence of insomnia in the COPD population was 25%. Of note, our study found that most COPD patients with insomnia were not receiving appropriate treatment for their sleep disturbance. It is possible that many patients considered their insomnia symptoms to be an inevitable complication of COPD and, thus, did not make a request for thorough evaluation.
Several studies have sought to assess the clinical impact of insomnia on patients with COPD. Budhiraja et al5 reported that COPD patients with insomnia had worse quality of life and a higher prevalence of daytime sleepiness. Recently, Omachi et al6 reported that COPD patients with disturbed sleep had more frequent COPD exacerbations and respiratory-related emergencies. Moreover, they found that sleep disturbance was a significant predictor of mortality in these patients. Similar trends were observed in the present study. Clinical insomnia was related to both a chronic bronchitis phenotype and more frequent exacerbations; however, these relationships were not statistically significant in multivariate analysis. Patients with chronic bronchitis phenotype usually have worse respiratory symptoms including nocturnal awakenings and higher risk of exacerbations.15 Also, they tend to have increased basal systemic inflammation and sympathetic tone.7,16 These are regarded as one of the possible hypotheses of their poor prognosis. Therefore, further detailed studies which focus on precise physiology and molecular aspect in this field are needed. We demonstrated that total CAT scores and most component CAT items tended to increase as insomnia severity increased. Additionally, global health status declined as insomnia severity increased. We were able to present a clear association between decreased quality of life and insomnia severity in this patient population.
In our study, CAT was the only clinical parameter associated with insomnia in patients with COPD. Recently, Xiang et al17 observed that physical illness and severe depression were significantly associated with insomnia in Hong Kong COPD patients. In the present study, we indirectly measured physical and emotional distress using the CAT score, a test that is commonly used in COPD. However, pulmonary function tests, which represent an objective assessment of the respiratory burden of COPD, were not significantly related to insomnia. This lack of association has been noted in several earlier studies.5,17
Finally, we attempted to correlate ISI and CAT scores. We found that total CAT scores were significantly associated with ISI scores, and both may be useful parameters for predicting the severity of insomnia in patients with COPD. Sleep is a component of the CAT score and the quality of sleep is rated from 0 to 5. However, few studies have assessed the ability of the sleep item alone to predict the presence or severity of insomnia. Sleep disturbances arise in patients with COPD for several reasons including persistent cough, hypoxemia, depression, and the effects of medications such as steroids or beta agonists on sleep initiation and maintenance.18 Therefore, it is likely that a global assessment of physical and emotional well-being would be more appropriate for estimating sleep quality in patients with COPD than the CAT sleep item alone.
Limitations
This study had several limitations. First, this study was cross-sectional and prevented comment on any potential causative relationship between ISI, CAT, and COPD. Second, this study was conducted at a single respiratory center and included a relatively small sample size. However, we found similar patient characteristics and prevalence of insomnia as observed in previous studies.5 It is likely that the findings of this study are representative and applicable to clinical practice and management. Third, this study did not include any objective information about patients’ sleep. A further large-scaled, multicenter, prospective study would be needed to strengthen the rationale for using CAT scores in the assessment of insomnia in patients with COPD.
Conclusion
The current study investigated the ability of the CAT score to predict the presence and severity of insomnia in patients with COPD. It showed that the total CAT score was closely related to insomnia severity. The regular use of CAT scores to assess patients with COPD may allow for better detection of sleep disturbances and improve the clinical management of insomnia in these patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. | ||
Sin DD, Anthonisen NR, Soriano JB, et al. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28:1245–1257. | ||
Ford ES, Murphy LB, Khavjou O, et al. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥18 years in the United States for 2010 and projections through 2020. Chest. 2015;147:31–45. | ||
Lim SW, Kim L. Insomnia in medical illnesses: the secondary insomnia. Sleep Med Psychol. 2005;12:11–16. | ||
Budhiraja R, Parthasarathy S, Budhiraja P, et al. Insomnia in patients with COPD. Sleep. 2012;35:369–375. | ||
Omachi TA, Blanc PD, Claman DM, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med. 2012;13:476–483. | ||
Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med. 2015;11:259–270. | ||
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. | ||
Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. | ||
Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34:648–654. | ||
Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Respirology. 2017;22:575–601. | ||
Worth H, Buhl R, Criée CP, Kardos P, Mailänder C, Vogelmeier C. The “real-life” COPD patient in Germany: the DACCORD study. Respir Med. 2016;111:64–71. | ||
Gershon AS, Mecredy GC, Guan J, Victor JC, Goldstein R, To T. Quantifying comorbidity in individuals with COPD: a population study. Eur Respir J. 2015;45:51–59. | ||
Camiciottoli G, Bigazzi F, Magni C, et al. Prevalence of comorbidities according to predominant phenotype and severity of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2229–2236. | ||
Kim V, Han MK, Vance GB, et al. The chronic bronchitic phenotype of COPD: an analysis of the COPDGene Study. Chest. 2011;140:626–633. | ||
Wedzicha JA, Calverley PM, Rabe KF. Roflumilast: a review of its use in the treatment of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:81–90. | ||
Xiang YT, Wong TS, Tsoh J, et al. Insomnia in older adults with chronic obstructive pulmonary disease (COPD) in Hong Kong: a case-control study. COPD. 2014;11:319–324. | ||
George CF, Bayliff CD. Management of insomnia in patients with chronic obstructive pulmonary disease. Drugs. 2003;63:379–387. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


