Back to Journals » Vascular Health and Risk Management » Volume 18
The Predictive Role of Inflammatory Biochemical Markers in Post-Operative Delirium After Vascular Surgery Procedures
Authors Pasqui E , de Donato G, Brancaccio B, Casilli G, Ferrante G , Cappelli A, Palasciano G
Received 2 April 2022
Accepted for publication 25 July 2022
Published 14 September 2022 Volume 2022:18 Pages 747—756
DOI https://doi.org/10.2147/VHRM.S368194
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mirna N Chahine
Edoardo Pasqui, Gianmarco de Donato, Brenda Brancaccio, Giulia Casilli, Giulia Ferrante, Alessandro Cappelli, Giancarlo Palasciano
Vascular Surgery Unit, Department of Medicine, Surgery and Neuroscience, University of Siena, Siena, Italy
Correspondence: Edoardo Pasqui, Vascular Surgery Unit, Department of Medicine, Surgery and Neuroscience, University of Siena, Viale Bracci, Siena, 53100, Italy, Tel +39 3428009201, Email [email protected]; [email protected]
Abstract:
Background: Post-operative delirium (POD) is a common complication, especially in elderly patients who underwent vascular surgery procedures. The aim of this study was to evaluate the relation of inflammatory biochemical markers as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and systemic inflammation index (SII) with POD occurrence.
Methods: This was a single-center, retrospective, observational study. We analyzed the perioperative data of patients who had undergone elective vascular surgery procedures. The occurrence of delirium after procedure was used to divide the population in two groups: POD-pos and POD-neg group. ROC curves were performed to find the appropriate cut-off values of NLR, PLR and SII. Multivariate analysis was used to identify the independent predictors for POD.
Results: A total of 646 patients were enrolled. Mean age was 76.2± 9.8 years, 68.4% were male. Seventy-three patients (11.3%) developed POD. Mean hospital stay was significantly increased in the POD-pos group (6.1± 5.4 vs 3.2± 2.8 days, p=0.0001). In-hospital reinterventions were more frequent in the POD-pos group (8.2% vs 3.8%). Blood values analysis reported significant differences: Hb, NLR, PLR, SII, creatinine and RCP were strongly increased (p< 0.05) in the POD-pos group. ROC curves identified cut-off values for NLR> 3.57, PLR> 139.2 and SII> 676.4. Multivariate analysis revealed that age, Renal Failure, peripheral revascularization procedures, major amputation, general anesthesia, hospitalization in the previous month, NLR> 3.57 and SII> 676.4 were independent risk factors for POD.
Conclusion: POD represents a common complication of vascular surgery patients. Our study demonstrated that NLR, PLR and SII are reliable and readily available laboratory predictors of POD in vascular surgery that could help in POD risk-stratification.
Keywords: delirium, vascular disease, risk assessment, vascular surgery, elderly
Introduction
Delirium is an extensive and serious problem, and it is incontestably a marker for vulnerability, and is associated with adverse outcomes in a number of different settings as surgical, medical, intensive care and care-homes.1–3 Fundamentally, the syndrome represents a decompensation of cerebral function in response to one or more pathophysiological stressors.4 Specifically, post-operative delirium (POD) is considered to be a geriatric syndrome caused by a complex interrelationship between predisposing and precipitating factors that occurred during the perioperative period. POD often starts in the recovery room and occurs up to 5 days after surgery. Usually, the onset is around the first 24-hours post-operatively and resolves in most patients within 48 hours. Very early onset of POD in the immediate post-anaesthesia period before or on arrival at the recovery room is referred to as emergence delirium.5,6 Different kinds of surgical procedures are related to variables’ rates of POD. Overall, the incidence of POD is estimated to be nearly 10% in patients following major elective non-cardiac surgery. Patients undergoing cardiovascular, major abdominal and orthopedic surgery are most prone to develop symptoms of POD.7,8 An interesting metanalysis by Raats et al revealed that the highest delirium incidence was observed after open aortic surgery as well as after surgery for critical limb ischemia.9
Those patients usually present with the hyperactive form of delirium, commonly characterized by restlessness, agitation, hallucinations, and delusions. In contrast, the hypoactive delirium, characterized by reduced movements, paucity of speech, and unresponsiveness, can be misdiagnosed as depression, anxiety, or even as a calm and comfortable patient when proper screening is not performed.
It is increasingly evident that delirium is associated with poor outcome and increased health care costs and its timely diagnosis is crucial to prevent patients from developing severe long-lasting complications. Due to its impact on patients’ hospitalization is recommended to screen for POD in all patients undergoing surgery starting in the recovery room and in each shift up to post-operative day 5. In addition, it’s recommended using a validated delirium score for POD screening.10
The pathophysiology of delirium remains uncertain due to a cumulative and additional effect of multiple intertwined variables.11 An increasing number of data supports the hypothesis of the prominent role of the systemic inflammation and/or neuroinflammation in which the immune response to a physical stress or an acute damage could result in delirium. Many inflammatory markers have been explored and linked to cognitive dysfunction such as C-reactive protein and neutrophil-to-lymphocyte ratio (NLR). NLR and other surrogates, such as platelet-to-lymphocyte ratio (PLR), have been also advocated as potential important markers of poor outcomes in surgical patients who underwent interventional procedures, also in the cardiovascular field.12–14 Literature have been proven that these markers are related to POD occurrence in cardiac surgery15 and after acute ischemic stroke.16 A novel marker, called Systemic Inflammatory Index (SII) is becoming a reliable tool on establishing the baseline inflammatory status of patients. Firstly proposed in the oncology field,17,18 SII has also been linked to cardiovascular disease as coronary disease,19 peripheral artery disease20 and also to psychiatric disease.21 In this perspective, the aim of the present study was to evaluate the potential predicting role of biochemical inflammatory markers in the occurrence of POD in patients who underwent elective vascular surgery procedures.
Materials and Methods
Overview
A retrospective observational analysis of all patients who underwent elective vascular surgery procedures at the University of Siena was performed. The main outcome of the study was the incidence of post-operative delirium in patients undergoing a vascular surgery procedure.
All patients who underwent a vascular surgery procedure in an elective setting between January 2018 and December 2019 were included in the study. Day-surgery procedures were excluded due to the limited time of in-hospital stay.
Every hospitalization was retrospectively analysed in terms of anamnestic features, preoperative blood sample (hemoglobin, white blood count, neutrophil and lymphocyte subpopulation, platelets, creatinine and C-reactive protein), type of procedures performed and Intensive Care Unit Stay.
Coronary artery disease, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, renal disease (chronic renal insufficiency defined by serum creatinine >1.2 mg/dL), hemodialysis, smoking history (any current or past regular use of tobacco), congestive heart failure, history of cerebrovascular events (stroke and/or transient ischemic attacks), history of cancer (any current or past incidence if malignancy), dyslipidemia, atrial fibrillation and psychiatric disease were considered as comorbidities.
In details, biochemicals inflammatory markers were furthermore analysed calculating the preoperative NLR, PLR and SII. NLR and PLR were obtained dividing the absolute neutrophil and platelet counts by the lymphocyte count while SII was calculated by the following formula: (Neutrophil count × Platelet count)/Lymphocyte count.
The onset of post-operative delirium and its management was detected, reviewing hospitalization charts. Post-operative delirium was defined as an acute confusional state, which can also be a part of fluctuating neuropsychiatric clinical syndrome and clinically manifesting as a disturbed state of consciousness, cognitive dysfunction or alteration in perception and behavior. The occurrence of POD is registered during hospitalization using a dedicated form related to the Confusion Assessment Method (CAM).22 Delirium occurrence related to acute conditions with direct impact on cognitive status (ie acute bleeding, sepsis, metabolic acute alterations etc) were excluded from the analysis. Delirium management and related consecutive events were registered. In-hospital reinterventions, deaths and major cardiovascular events (MACE’s) were evaluated as secondary outcomes.
The institutional review board of University of Siena endorsed the study protocol. The ethical committee of the hospital was informed of the no-experimental design of the retrospective investigation and endorsed the study. Informed consent waiver was approved by the ethical committee due to its retrospective design based on patient records. We performed the study in accordance with the Declaration of Helsinki.
Analysis Path
Total population descriptive study was performed.
Two sub-population groups were identified: POD-pos group (post-operative delirium positive) and POD-neg group (post-operative delirium negative) respectively composed by patients who experienced POD and by patients who did not.
We used proportions to present categorical variables and Chi-square test for comparison between the groups. Continuous variables are presented as means with standard deviation. Student’s t-test was used to compare normally distributed variables. Mann–Whitney U tests were used to compare nonnormally distributed variables. Receiver operating characteristic (ROC) curves were performed to calculate the most appropriate cut-off values of NLR, PLR and SII. The obtained values were used and included in the subsequent stepwise multivariate analysis.
Data sets were analyzed using univariable methods with the aim of determining the risk factors correlated to the incidence of POD. The variables included in this part of statistical analysis were anamnestic features, pre-operative blood sample, NLR, PLR, SII, type of intervention and procedural characteristics.
Multivariate logistic regression analysis was performed to identify determinants independently associated with POD. Variables associated with POD in the univariable analyses with a p-value <0.10 were included in the multivariate analysis in a forward-stepwise manner. Independent predictor variables that contributed to the final multivariate model were considered as significant risk factors for POD occurrence if they achieved a two-sided p < 0.05.
All statistical analyses were performed with GraphPad Prism 9.0 (GraphPad Software Inc., San Diego, CA, USA) and StatPlus Build 7.1.1 (AnalysisSoft Inc., Walnut, CA, USA).
Results
Descriptive Analysis
A total of 646 patients were enrolled in this retrospective analysis. Mean age was 76.2±9.8 years and 442 (68.4%) were male. Full baseline population characteristics are listed in Table 1.
 |
Table 1 Baseline Characteristics of Study Population |
Details of all procedures included in the study are highlighted in Table 2.
 |
Table 2 Procedural Characteristics and In-Hospital Outcomes |
Seventy-three patients (11.3%) developed POD during hospitalization. Fifty had hyperactive POD that necessitated dedicated drugs administration, of them 17 also needed physical contention.
Descriptive analysis between the two study groups revealed that patients included in the POD-pos group were likely older, had a history of cardiac disease (heart failure and coronary artery disease), chronic renal failure and dialysis and had a pre-existing psychiatric disease. In addition, they were more likely to have a previous hospitalization within 1 month. In terms of drugs assumption, the POD-pos group was more likely to assume anticoagulant and antipsychotic drugs. In terms of vascular procedure performed, POD occurred more frequently in patients who underwent aortic open repair, endovascular revascularization procedures for chronic-limb-threatening-ischemia, and major amputation.
In addition, also patients who underwent general anesthesia were more prone to experience POD.
POD-Related Outcomes
Mean hospital stay was significantly increased (p=0.0001) in the POD-pos group (6.1±5.4 days), with respect to the POD-neg group (3.2±2.8 days).
The average duration of vascular intervention was increased in the POD-pos group even if with no statistical significance (p=0.29). In-hospital death and in-hospital MACE were not increased in the POD-pos group, while in-hospital reinterventions were more frequently performed in the POD-pos group with respect to the POD-neg group (8.2% vs 3.8%, p=0.11). Full data regarding perioperative outcomes are listed in Table 3.
 |
Table 3 Secondary Outcomes Between POD-Pos and POD-Neg Groups |
Inflammatory Biomarkers Analysis
Blood values analysis reported significant differences. Hb (11.5±2.9 vs 13.1±2.1, p=0.0001), WBC (9.56±3.88 vs 8.1±2.96, p=0.0001), neutrophil subpopulation (7.1±3.67 vs 5.4±2.5, p=0.0001), lymphocyte subpopulation (1.52±0.72 vs 1.8±0.86, p=0.0079), NLR (5.99±5.2 vs 3.77±3.2, p=0.0001), PLR (199.4±149.6 vs 158.5±103.8, p=0.0028), SII (1674.9±1067.7 vs 945.6±745.3, p=0.0001), Creatinine (1.46±0.7 vs 1.21±0.9, p=0.022) and C-reactive protein (2.42±1.2 vs 0.77±2.74, p=0.0001) were statistically different between POD-pos and POD-neg groups, respectively (Figure 1).
 |
Figure 1 Biochemical markers differences between POD-pos and POD-neg groups. Asterisks indicate high significant difference between the two groups (p=0.0001). |
In details, NLR, PLR and SII were further analyzed. ROC curves were performed to identify cut-off values of previous markers.
NLR cut-off value was 3.57 (sensitivity 64.38%, specificity 66.84%, area under the curve [AUC] 0.688, CI:0.626–0.75, p<0.0001)
PLR cut-off value was 139.2 (sensitivity 64.38%, specificity 53.05%, AUC 0.617, CI: 0.549–0.686, p=0.01)
SII cut-off value was 676.4 (sensitivity 68.5%, specificity 55%, AUC 0.667, CI: 0.6–0.733 p<0.0001). (Figure 2)
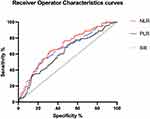 |
Figure 2 Receiver operating characteristic curves of the three biochemical markers (NLR, PLR and SII) evaluated. |
Univariable and Multivariable Analysis
All variables were considered for univariable and multivariable analysis. Variables identified as significant from the univariable analyses were entered in the multivariate logistic regression analysis. Age, CKD, PAD revascularization procedures (endovascular and surgical), major amputation, general anesthesia and hospitalization in the previous month were independent risk factors for POD incidence. Regarding biochemical inflammatory markers NLR>3.57 (1.76 CI [1.23–2.61]) and SII>676.4 (1.67 [1.57–3.12]) were found to be independent risk factors for POD incidence. In addition, Hb level<7 g/dl emerged to be a risk factor of POD. Full list of multivariate analysis outcomes is reported in Table 4.
 |
Table 4 Results from Multivariate Analysis: Effect of Various Variables Extrapolated from Univariate Analysis on POD Incidence |
Discussion
In our study, we investigated incidence and perioperative risk factors of POD after elective vascular surgery procedures with the aim of determine whether pre-operative systemic inflammatory markers as NLR, PLR and SII would predict the occurrence of POD. ROC curves highlighted that NLR > 3.57, PLR > 139.2 and SII > 676.4 were interesting markers for predicting POD. We also identified risk factors associated with POD and multivariable analysis revealed that age, CKD, PAD revascularization procedures (endovascular and surgical), major amputation, general anesthesia and hospitalization in the previous month were independent risk factors for POD incidence. Also, NLR > 3.57 and SII > 676.4 were found to be independent risk factors for POD occurrence. Delirium is common complication following elective and urgent/emergent surgery, especially in elderly patients. Although its limited temporary extension, POD represents a delicate issue in term of patients’ discomfort, increased risk of remaining in the hospital, in-hospital complications, accidental fallen, increased risk of early and long-term mortality and increased risk of physical dependency. From this perspective, the economic impact should be considered as a major concern. Understanding the mechanism of POD and identifying its possible predictors could help healthcare professionals to act with the aim of reducing POD’s incidence with all the beneficial consequences. In this light, a meta-analysis demonstrated that delirium during hospitalization doubles a patient’s risk of post-discharge institutionalization and death and increases risk of dementia up to 10-fold. Impressively, these poor outcomes were independent of common confounders like age, sex, and comorbidities.23
Delirium may occur through a variety of potential pathophysiologic mechanism:
One of them is the theory of systemic inflammation, neuroinflammation and neurotransmitters balance.
A direct measurement of brain inflammatory mediators may provide some clarity on the role of neuroinflammation in POD, but this is ethically and practically difficult.
So, the measurement of blood levels of inflammatory mediators could represent a reliable surrogate. A variety of markers could be taken in account, but many of them are expensive and are not usual part of routine blood exams as IL-6, IL-10, IL-1β.24,25 Indirect inflammatory markers could be obtained from routine blood examinations, such as NLR, PLR and SII. In recent years, they were profusely studied and interrelated with many pathological conditions.
A few papers have investigated possible connections between blood-sample inflammation markers and POD. Kinoshita et al, in their recent work, outlined the predictive role of NLR in POD occurrence in patients who underwent head and neck free-flap reconstruction surgery.26 A higher value of NLR (NLR > 3) was independently associated with POD. Again, He et al proved that in 780 elderly patients with total hip arthroplasty for hip fracture, NLR correlated with higher incidence of POD, confirmed also by multivariate analysis.27 Jiang et al evaluated the influence of PLR with the occurrence of delirium in critically ill patients admitted to Intensive Care Unit, confirming its predicting role as independent risk factor.28
Regarding cardiovascular disease, Koftis et al evaluated the potential interest of NLR, PLR and white blood cell count on the occurrence of POD after cardiac surgery. Platelet-to-WBC ratio was the most appropriate marker with the strongest correlation with POD.13 The same team identified that NLR > 4.86 could be a potential predictive marker for POD occurrence in patients with ischemic stroke.14
Up to now literature lacks evidence regarding the relation between SII and POD, SII remains an important index of poor outcomes in oncological patients.29,30
Our paper confirmed the interesting role of NLR, PLR and SII on the occurrence of POD. The outlined cut-off values are in line with similar reports that investigated inflammatory markers in other surgical fields. NLR > 3 and NLR > 3.5 was considered an independent risk factor for POD after head and neck free-flap reconstruction and arthroplasty for hip fracture, respectively,26,27 while PLR and SII were not consistently studied in order to identify a single value for discrimination.
The population study consisted majorly in elderly patients with a high complexity baseline characteristics. Numerous comorbidities were present, leading to define a typical patient archetype prone to in-hospital complications. POD is one of them, and as confirmed by our analysis, an elderly patient with pre-existing cardiac, renal and psychiatric disease has a higher risk to develop POD after vascular surgery. In addition, our report, highlighted that patients who underwent PAD endovascular revascularization procedures or major amputation have higher rates of POD occurrence. This could be explained by the patients’ poor clinical status especially in case of the necessity of a major amputation. A recent paper by Gutierrez et al31 found that 26% of the cases undergoing infrainguinal lower extremity bypass developed post-operative delirium, a very high rate with respect to the average of other kinds of procedure. Obviously, patients with chronic-limb-threatening ischemia have been already associated to high clinical and subclinical inflammation subset. Our study also confirmed that this condition represents an independent risk factor for POD development. Previous papers explored this topic proposing a similar scenario of POD-pos vascular surgical patients.32
Limitations
The paper has many limitations. First, the population examined is quite heterogeneous in terms of procedures performed (aortic surgery, carotid surgery, peripheral arterial surgery). This could be confounding, but the aim of our paper was to investigate POD occurrence during vascular surgery daily practice. Second, the retrospective nature of the study. Third, we are aware that POD is sometimes difficult to identify and consecutively some events could be missing. Fourth, our study was centered on evaluating the relation between inflammatory markers and POD. We are aware that several variables could have an impact on POD and some of them were not considered. In this light, our proposal was to overcome this limitation by increasing the numerosity of the study population and adding other variables of interest to create a more precise prediction model for POD occurrence.
Conclusion
POD represents a common complication in post-surgery patients, especially in elderly, fragile patients. In vascular surgery, this is the most common phenotype of patients for whom POD could lead to serious complications. Our study demonstrated that simple and readily available inflammatory markers as NLR, PLR and SII could be used as adjunctive novel tools in stratifying pre-operative patients’ risk for POD occurrence. Further studies are essential to define and validate more accurate cut-off values. The inclusion of these markers in more comprehensive risk-assessment score for POD occurrence could be an interesting use that could imply pre-emptive actions to reduce POD and its complications.
Abbreviations
POD, post-operative delirium; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio; SII, Systemic Inflammatory Index; MACE, major cardiovascular events; POD-pos group, post-operative delirium positive; POD-neg group, post-operative delirium negative; ROC, receiver operator characteristics.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding or grants have been received for this project.
Disclosure
The authors have no conflict of interest to declare for this work.
References
1. Marengoni A, Zucchelli A, Grande G, Fratiglioni L, Rizzuto D. The impact of delirium on outcomes for older adults hospitalised with COVID-19. Age Ageing. 2020;49(6):923–926. doi:10.1093/ageing/afaa189
2. Siddiqi N, Young J, House AO, et al. Stop Delirium! A complex intervention to prevent delirium in care homes: a mixed-methods feasibility study. Age Ageing. 2011;40(1):90–98. doi:10.1093/ageing/afq126
3. Girard TD, Pandharipande PP, Ely EW. Delirium in the intensive care unit. Crit Care. 2008;12(Suppl3):S3. doi:10.1186/cc6149
4. MacLullich AM, Hall RJ. Who understands delirium? Age Ageing. 2011;40:412–414. doi:10.1093/ageing/afr062
5. Olin K, Eriksdotter-Jönhagen M, Jansson A, Herrington MK, Kristiansson M, Permert J. Postoperative delirium in elderly patients after major abdominal surgery. Br J Surg. 2005;92(12):1559–1564. doi:10.1002/bjs.5053
6. Lepousé C, Lautner CA, Liu L, Gomis P, Leon A. Emergence delirium in adults in the post-anaesthesia care unit. Br J Anaesth. 2006;96:747–753. doi:10.1093/bja/ael094
7. Rasmussen LS, Jt M. Central nervous system dysfunction after anesthesia in the geriatric patient. Anesthesiol Clin North America. 2000;18:59–70. doi:10.1016/S0889-8537(05)70149-8
8. Duppils GS, Wikblad K. Acute confusional states in patients undergoing Hip surgery, a prospective observation study. Gerontology. 2000;46:36–43. doi:10.1159/000022131
9. Raats JW, Steunenberg SL, de Lange DC, van der Laan L. Risk factors of post-operative delirium after elective vascular surgery in the elderly: a systematic review. Int J Surg. 2016;35:1–6. doi:10.1016/j.ijsu.2016.09.001
10. Aldecoa C, Bettelli G, Bilotta F, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34(4):192–214. doi:10.1097/EJA.0000000000000594
11. McDaniel M, Brudney C. Postoperative delirium: etiology and management. Curr Opin Crit Care. 2012;18(4):372–376. doi:10.1097/MCC.0b013e3283557211
12. Pasqui E, de Donato G, Giannace G, et al. The relation between neutrophil/lymphocyte and platelet/lymphocyte ratios with mortality and limb amputation after acute limb ischaemia. Vascular. 2021;21:17085381211010012.
13. Aurelian SV, Adrian M, Andercou O, et al. Neutrophil-to-lymphocyte ratio: a comparative study of rupture to nonruptured infrarenal abdominal aortic aneurysm. Ann Vasc Surg. 2019;58:270–275. doi:10.1016/j.avsg.2018.11.026
14. Murakami Y, Saito H, Shimizu S, Kono Y, Shishido Y, Miyatani K. Neutrophil-to-lymphocyte ratio as a prognostic indicator in patients with unresectable gastric cancer. Anticancer Res. 2019;39(5):2583–2589. doi:10.21873/anticanres.13381
15. Kotfis K, Ślozowska J, Safranow K, Szylińska A, Listewnik M. The practical use of white cell inflammatory biomarkers in prediction of postoperative delirium after cardiac surgery. Brain Sci. 2019;2(9):308. doi:10.3390/brainsci9110308
16. Kotfis K, Bott-Olejnik M, Szylińska A, Rotter I. Could neutrophil-to-lymphocyte ratio (NLR) serve as a potential marker for delirium prediction in patients with acute ischemic stroke? A prospective observational study. J Clin Med. 2019;22(8):1075. doi:10.3390/jcm8071075
17. Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;1(20):6212–6222. doi:10.1158/1078-0432.CCR-14-0442
18. Li C, Tian W, Zhao F, et al. Systemic immune-inflammation index, SII, for prognosis of elderly patients with newly diagnosed tumors. Oncotarget. 2018;19(9):35293–35299. doi:10.18632/oncotarget.24293
19. Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50:e13230. doi:10.1111/eci.13230
20. Zhang Z, Chen Z. Higher Systemic Immune-Inflammation Index is Associated With Higher Likelihood of Peripheral Arterial Disease. Ann Vasc Surg. 2021;22:253.
21. Wang J, Zhou D, Dai Z, Li X. Association between Systemic Immune-Inflammation Index and diabetic depression. Clin Interv Aging. 2021;16:97–105. doi:10.2147/CIA.S285000
22. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;15(113):941–948. doi:10.7326/0003-4819-113-12-941
23. Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304:443–451. doi:10.1001/jama.2010.1013
24. Noah AM, Almghairbi D, Evley R, Moppett IK. Preoperative inflammatory mediators and postoperative delirium: systematic review and meta-analysis. Br J Anaesth. 2021;127(3):424–434. doi:10.1016/j.bja.2021.04.033
25. Brattinga B, Plas M, Spikman JM, Rutgers A, de Haan JJ, Absalom AR. The association between the inflammatory response following surgery and post-operative delirium in older oncological patients: a prospective cohort study. Age Ageing. 2022;51(2):afab237. doi:10.1093/ageing/afab237
26. Kinoshita H, Saito J, Takekawa D, Ohyama T, Kushikata T, Hirota K. Availability of preoperative neutrophil-lymphocyte ratio to predict postoperative delirium after head and neck free-flap reconstruction: a retrospective study. PLoS ONE. 2021;16(7):e0254654. doi:10.1371/journal.pone.0254654
27. He R, Wang F, Shen H, Zeng Y, Zhang L. Association between increased neutrophil-to-lymphocyte ratio and postoperative delirium in elderly patients with total Hip arthroplasty for Hip fracture. BMC Psychiatry. 2020;20(1):496. doi:10.1186/s12888-020-02908-2
28. Jiang X, Shen Y, Fang Q, Zhang W, Cheng X. Platelet-to-lymphocyte ratio as a predictive index for delirium in critically ill patients: a retrospective observational study. Medicine. 2020;99(43):e22884. doi:10.1097/MD.0000000000022884
29. Li C, Tian W, Zhao F, et al. Systemic immune-inflammation index, SII, for prognosis of elderly patients with newly diagnosed tumors. Oncotarget. 2018;9(82):35293–35299.
30. Huang H, Liu Q, Zhu L, et al. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer. Sci Rep. 2019;9(1):3284. doi:10.1038/s41598-019-39150-0
31. Gutierrez RD, Matthay ZA, Smith EJT, et al. Delirium associated adverse events and resource use after infrainguinal lower extremity bypass. Ann Vasc Surg. 2021;79:407–408. doi:10.1016/j.avsg.2021.12.061
32. Visser L, Prent A, Banning LBD, van Leeuwen BL, Zeebregts CJ, Pol RA. Risk factors for delirium after vascular surgery: a systematic review and meta-analysis. Ann Vasc Surg. 2021;76:500–513. doi:10.1016/j.avsg.2021.03.034
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
