Back to Journals » Patient Preference and Adherence » Volume 9
The German version of the Individualized Care Scale – assessing validity and reliability
Authors Köberich S, Suhonen R , Feuchtinger J, Farin E
Received 13 November 2014
Accepted for publication 30 January 2015
Published 23 March 2015 Volume 2015:9 Pages 483—494
DOI https://doi.org/10.2147/PPA.S77486
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Stefan Köberich,1,2 Riitta Suhonen,3 Johanna Feuchtinger,4 Erik Farin1
1Institute for Quality Management and Social Medicine, Medical Center – University of Freiburg, Freiburg, Germany; 2Pflegedirektion, Heart Center – University of Freiburg, Freiburg, Germany; 3Department of Nursing Science, University of Turku, Turku, Finland; 4Quality and Development in Nursing Care, Medical Center – University of Freiburg, Freiburg, Germany
Aim: To assess validity and reliability of the German version of the Individualized Care Scale (ICS).
Background: Individualized nursing care plays a pivotal role in establishing patient-centered care. To assess individualized nursing care and to compare it in different settings and countries, valid and reliable instruments are needed. No psychometric-tested instrument for comparing individualized nursing care with other countries is available in Germany.
Design: Cross-sectional study.
Methods: Data were collected between September 2013 and June 2014 from 606 patients in 20 wards in five hospitals across Germany. Unidimensionality of the ICS scales ICSA (patients’ views on how individuality is supported through nursing interventions) and ICSB (patients’ perceptions of individualized nursing care) was analyzed by confirmatory factor analysis. Internal consistency was assessed by calculating Cronbach’s alpha. The Smoliner Scale (patients’ perceptions of the decision-making process in nursing care) and results from participating hospitals’ assessment of the nursing care delivery systems were used to assess known-groups validity and concurrent validity.
Results: Fit indices of confirmatory factor analysis indicate unidimensionality of the ICSA (Comparative Fit Index: 0.92; Tucker-Lewis Index: 0.902; root mean square error of approximation: 0.09; standardized root mean square residual: 0.05) and the ICSB (Comparative Fit Index: 0.91; Tucker-Lewis Index: 0.89; root mean square error of approximation: 0.09; standardized root mean square residual: 0.05). Internal consistency using Cronbach’s alpha was 0.95 (95% confidence interval: 0.94–0.95) for ICSA and 0.93 (95% confidence interval: 0.92–0.94) for the ICSB. Concurrent validity was established by a significant relationship between the Smoliner Scale and ICSA (r=0.66; P<0.01) and ICSB (r=0.72; P<0.01). Known-groups validity was approved by ICSA/ICSB score differences related to nursing care delivery systems and patients’ perceptions of decision-making style.
Conclusion: The German version of the ICS is deemed a valid and reliable instrument for use in practice and research with hospitalized patients.
Keywords: patient-centered care, hospitals, psychometrics, nursing, Individualized Care Scale, ICS
Introduction
In the last 2 decades patient-centered care has attracted increasing attention in all settings of the health care system and it is advocated by international health and patient organizations.1,2 Patient-centered care can be defined as a holistic care delivery approach that puts the patient at the center of the care process which is holistic, individualized, tailored, respectful, and empowering.3,4 It respects and acknowledges patients’ needs, values, and individuality,4 and is associated with better patient outcomes across the nursing and medical settings. Introduction of patient-centered nursing care (PCNC) principles improves patients’ self-care ability,5,6 satisfaction with care,5,7,8 and autonomy,9 as well as quality of life.5,9 To establish a reliable link between PCNC and patient outcomes, valid and reliable instruments are needed. A recently conducted systematic review10 identified four instruments measuring PCNC with robust psychometric properties that could be used in practice and research: the Individualized Care Scale (ICS),11,12 the Client-Centred Care Questionnaire,13 the Oncology Patients’ Perceptions of the Quality of Nursing Care Scale14 and the Smoliner Scale.15 All of these instruments assess patients’ perceptions of patient-centered care which might be different from the patient-centered care approaches perceived by health care providers.
The ICS is the most often reported and most extensively tested instrument, used in many different countries (Finland, Sweden, Greece, Cyprus, Canada, USA, Portugal, Turkey, Great Britain, the Czech Republic, and Hungary).16–18 The application of such a widely used instrument makes it possible to compare the degree of perceived PCNC as well as the factors influencing it. Although the ICS has been translated into the German language, psychometric properties have been assessed only with a modified version within the psychiatric setting.19 Therefore, the aim of this study was to assess the validity and reliability of the German version of the ICS using data from non-psychiatric hospitalized patients.
The study
For the purpose of this study, we used the German version of the ICS for use in somatic hospital settings, developed by Pöhler19 before adaptation to psychiatric settings. The aspects of validity and reliability assessed were: construct validity (structural validity and validity with known-groups), criterion validity (concurrent validity), and internal consistency reliability.
Design
This study used a cross-sectional survey design and was conducted between September 2013 and June 2014.
Study population
Five hospitals across Germany took part in this study (Table 1). All patients on the designated wards at the participating hospitals staying longer than 2 days within the data collection period were eligible to take part in this study. The data collection periods were scheduled by the hospitals and lasted from 2 to 9 months. Exclusion criteria were: age <18 years; disorientation in one of the following perspectives: time, person, situation or location; cognitive impairment or documented diagnosis of dementia; patient is unable to fill in the questionnaire according to the judgment of a designated member of the nursing staff; patient is incapable of reading or understanding the German language; and visual disability.
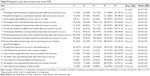
  | Table 1 Characteristics of participating wards |
Sample size
While there is no consensus on optimal sample size to evaluate validity and reliability of an assessment instrument, our target sample size was based on the statistical procedure requiring the largest sample size (hierarchical linear model). This study of ICS validity and reliability was part of a broader study to detect and determine influencing factors on patients’ perceptions of individualized care using a two-level hierarchical linear model. Since consensus about the optimal sample size for a two-level hierarchical linear model does not exist we applied a rule-of-thumb of 30 patients per ward, which for 20 wards yields a total of 600 patients.
Procedure
Eligible patients were approached at the earliest 2 days before discharge by a designated member of the nursing staff on the participating wards. An envelope containing a cover letter of invitation, a questionnaire, and a self-addressed envelope for returning the questionnaire was handed to the patient by a member of the nursing staff. The cover letter provided information about the study aim and assured potential participants that the data provided would be kept confidential. They received further information about the study from the nurse if they so desired. Voluntary consent was assumed if the patient returned the questionnaire. The questionnaire was returned by the patient to the nurses using a prepaid, closed envelope and was sent to the principal investigator. The self-administered questionnaire collected data about patients’ perceptions of PCNC using the ICS and the “Experience” subscale of the Smoliner Scale as well as socio-demographic and disease-specific data.
In addition, some hospitals provided us with their results from an assessment aiming to determine the nursing care delivery system on participating wards. It was not explicitly part of this study but rather part of the organizational development of the participating hospitals.
Measurement
The ICS
The ICS is a bipartite questionnaire and measures patients’ perceptions of individualized nursing care during a hospital stay at the time of hospital discharge. It was originally developed by Suhonen et al within the Finnish health care system.11,12 Suhonen et al assumed that individualized care will be promoted if nurses’ activities take a patient’s individuality into account and facilitate his/her participation in decision-making about nursing care. A first draft of the ICS contained two dimensions labeled “Patient’s individuality” and “Participation in decision-making”.
In 2005 the operationalization of the elements of patients’ individualized care was refined and the ICS was revised. The scale now consisted of two scales (patients’ views on how individuality is supported through nursing interventions – ICSA; patients’ perceptions of individualized nursing care – ICSB) with three subscales in each scale, labeled “clinical situation” (ClinA/ClinB), “personal life situation” (PersA/PersB), and “decisional control over care” (DecA/DecB). The scales comprise 19 items each, with seven items in the subscale “clinical situation”, five items in “personal life situation”, and seven items in “decisional control over care”.20
A further revision was made in 2010 after testing the ICS’s cross-cultural validity using patient data from five different countries (Sweden, Finland, Greece, USA, UK). Two items were deleted from the ICSA and ICSB each, leaving each scale containing 17 items.
Internal consistency of the revised ICS using Cronbach’s alpha was above the recommended level of 0.7 for each scale- and subscale-version, except for the alpha of subscales ClinA in the USA sample and DecB in each of the Finnish and USA samples. Exploratory factor analysis supported the scale’s conceptual structure, explaining 58%–79% of the total variance.17
German version of ICS
In 2010 the ICS was translated into German19 and retranslated into the English language. The retranslated version of the ICS was checked for inconsistencies with the original English version by a panel of two nurses and one official translator. Conceptual ambiguities were clarified with the scale’s original author and with the help of a psychologist.
The German version was then adapted for use in the psychiatric setting and psychometrically tested in 90 psychiatric patients. Internal consistency using Cronbach’s alpha was satisfactory with values of 0.93 and 0.91 for scales ICSA and ICSB and 0.65–0.90 for the subscales. Test–retest reliability using Pearson’s r revealed a stable instrument with r-values of 0.698–0.878 for the subscales, and 0.887 and 0.876 for ICSA and ICSB. To assess construct validity, exploratory factor analysis was conducted with ambiguous results. Some items could not be clearly allocated to one factor. Convergent validity was assessed using the “Experience” subscale of the Smoliner Scale which evaluates patients’ perceptions of the decision-making process in nursing care.15 The result reveal a medium correlation between the ICS and the Smoliner Scale (r=0.61).
The German version of the ICS consists of two scales containing 17 items in each scale. The items are rated via a 5-point Likert Scale (1= “strongly disagree”; 5= “strongly agree”). Sum scores of the ICS and its scales are calculated as mean values of all responses within a theoretical range of 1 to 5, with higher values indicating more individualized care.
Instrument to assess nursing care delivery systems
To assess the nursing care delivery system, the “Instrument to assess nursing care delivery systems” (Instrument zur Erfassung von Pflegesystemen – IzEP) was used. It was developed by a group of German, Austrian, and Swiss nursing scientists, nursing managers, and nurse practitioners, with the aim of evaluating nursing care delivery systems in different health care settings.21
IzEP consists of nine questionnaires of different lengths. The questionnaires assess five characteristics which define a ward’s nursing care delivery system: head or staff nurse’s role perception, communication, nursing care process, realization of the nursing concept, and responsibility and continuity in the assignment of nurses to patients. To assess these characteristics, head and staff nurses, patients, relatives, therapists, physicians, and external contacts are interviewed using standardized questionnaires, and patient records as well as duty rosters are analyzed. To determine the existing nursing care delivery systems, results from the questionnaires are triangulated to an overall score.
Overall scores range from 0 to 100. Cut-off values for task-oriented nursing, zone nursing, and patient-oriented nursing are 10, 40, and 75, respectively. Task-oriented nursing is defined as a nursing care model in which the head nurse has case responsibility for all patients. Nursing tasks are assigned by the head nurse to staff members and nursing tasks are usually executed in rounds. In a zone nursing model, the head nurse also has case responsibility. However, nurses are responsible for a certain area or group of patients for a limited time period. In the patient-oriented care model (eg, primary nursing), case responsibility is decentralized. A dedicated nurse (primary nurse) has case-responsibility for one or more patients. This system is considered more patient-centered than other nursing care delivery systems.22 Different aspects of the validity and reliability have been assessed and confirmed.23
Smoliner Scale
To assess patients’ perceptions of the decision-making process in nursing care, the “Experience” subscale of the Smoliner Scale was used, which is only available in German. The Smoliner Scale is an instrument measuring patients’ wishes and perceptions of various stages of the decision-making process about his/her nursing care (information exchange, deliberation, and deciding on treatment to implement) and is based on the model of treatment decision-making described by Charles et al.24 Construct validity and internal consistency of the total Smoliner Scale and its subscales have been assessed and psychometric properties found satisfactory. Cronbach’s alpha for the “Experience” subscale was 0.86.15
The “Experience” subscale consists of three parts measuring patients’ perceptions: a) of the information exchange and deliberation process; b) of being involved in decision-making about specific nursing tasks (eg, hygiene, sleep, and rest); and c) of the kind of decision-making process about nursing care. To assess patients’ perceptions of information exchange and the deliberation process, the patient rates five statements using a 6-point Likert Scale ranging from 1 “never” to 6 “always”. The summed score of this part ranged from 6 to 30.
To assess patients’ perceptions of the decision-making process, each patient was asked to indicate which of four statements best reflected his/her experience. The four statements address three types of decision-making processes: paternalistic, shared, and informed. Two of the four statements could be assigned to a paternalistic decision-making process, one to shared, and one to the informed decision-making process. Within the paternalistic decision-making process, the health care provider is the person who makes the decision about the appropriate treatment. The shared decision-making process is characterized by an exchange of all relevant information between the health care provider and patient to enable him/her to make the right decision about the treatment together with the health care provider. If the patient receives all the relevant information from the health care provider for making a decision, is able to discuss this information with potential others, and comes to a decision on his/her own, the decision-making process is regarded as informed.24 For the purpose of our study we used only those parts assessing patients’ perceptions of the information exchange, deliberation, and decision-making process about nursing care.
Socio-demographic and disease-related data were collected with a self-administered questionnaire. The patient was asked to state sex, age, nationality (German or other), marital status, educational level, hospital stay (planned, unplanned), length of hospital stay, and self-rated health. Self-rated health was assessed using a 6-point Likert Scale with 1 for “very good” and 6 for “very bad”.
Ethical consideration
The study protocol was approved by the ethics committee at Albert Ludwig University of Freiburg, Germany (EK-Freiburg 318/13). The study conforms to the principles outlined in the Declaration of Helsinki. Furthermore, the data protection protocol was approved by the data protection officer of the Medical Center – University of Freiburg, Freiburg, Germany.
Data analysis
For statistical data analysis we used IBM SPSS Statistics (version 22) and IBM SPSS AMOS (version 21). Missing data were handled as follows: cases were excluded from the analysis if more than 20% of items were missing on any one of the three scales (ICSA, ICSB, or the “Experience” subscale of the Smoliner Scale). All other questionnaires were included.
Descriptive statistics were used to describe patients’ socio-demographic and disease-specific characteristics. Numbers and percentages were calculated if variables were nominally-scaled; interval-scaled variables were displayed using mean and standard deviation (SD) if normally distributed. Otherwise they are displayed as medians and interquartile ranges. Normal distribution was tested using the Shapiro–Wilk test.
To describe every single item in the ICS, response patterns, mean values, SD, median, and interquartile range were calculated. We also calculated inter-item correlation.
Confirmatory factor analysis was used to assess the unidimensionality of the ICS scales. Missing data in the ICSA or ISCB were imputed using the expectation-maximization algorithm by Norm (version 2.03) software. The Comparative Fit Index, Tucker-Lewis Index, root mean square error of approximation and the standardized root mean square residual were used as indicators of model fit. According to Hu and Bentler,26 Comparative Fit Index and Tucker-Lewis Index values >0.90 suggest an acceptable fit while values >0.95 suggest a good fit. Root mean square error of approximation values of <0.10 or <0.05 indicate a moderate or good model fit, respectively. The standardized root mean square residual should not exceed 0.08. A model fit was assumed if at least three of the fit indices showed values indicating model fit.
Internal consistency was assessed using item-total correlations and Cronbach’s alpha and its 95% confidence interval. According to Streiner and Norman26 an item should correlate with the total score at least with r>0.2. According to a matrix of adequate internal consistency provided by Ponterotto and Ruckdeschel,28 appraisal of Cronbach’s alpha values depends on the number of items per scale and sample size used to calculate alpha (Table 2). We used this matrix to appraise alpha values of the ICSA, ICSB, and their subscales as indicators of internal consistency.
  | Table 2 Appraisal of Cronbach’s alpha |
To assess construct validity, in terms of validity with known groups, ICSA/ICSB scores were compared among different groups in the nursing care delivery system (task-oriented nursing, zone nursing, and patient-oriented nursing care) and different groups of patients’ perceptions of the decision-making process about nursing care (paternalistic, informed, shared) using the Kruskal–Wallis test. Our hypothesis was that ICSA/ICSB scores would differ significantly depending on the nursing care delivery system and the perceived decision-making style respectively. We assumed that patients’ perceptions of individualized care would increase if the decision-making process about nursing care and nursing care delivery system is more patient-oriented. As a post hoc analysis, we also analyzed differences in ICSA/ICSB among the different nursing care delivery systems. To assess concurrent validity, correlations were measured between ICSA/ICSB scores and the sum score of the “Experience” subscale in the Smoliner Scale which reflects patients’ overall perception of the information exchange and deliberation process in nursing care. Based on previous work,19 we hypothesized that this part of the “Experience” subscale in the Smoliner Scale would display a medium correlation with the ICS-Scales (Pearson’s r≥0.5). As there is no standardized interpretation of Pearson’s r, we used the classification proposed by Bühl.28 Bühl classified r-values between 0 and 0.2 as a very low correlation, values between 0.2 and 0.5 as low correlation, values between 0.5 and 0.7 as a medium correlation, values between 0.7 and 0.9 as high correlation, and values above 0.9 as very high correlation.28
We followed the terminology of validity and reliability as proposed by Mokkink et al29 which is based on the results of the “COnsensus-based Standards for the selection of health Measurement INstruments” (COSMIN) study.
A P-value of ≤0.05 was deemed statistically significant for all tests.
Results
Of 884 questionnaires distributed a total of 699 (79.1%) were returned. Ninety-three (13.3%) data-sets contained more than 20% missing data on one of the three scales (ICSA, ICSB, or Smoliner Scale) and were subsequently excluded from further analysis, leaving 606 cases for analysis.
Sample characteristics
Patients were predominantly male, with a mean age of 57.5 years. Most patients were German, married, and had an educational level of 9 years at most. Numbers of planned and unplanned hospital stays were almost equal and the median length of hospital stay was 8 days. Median of self-rated health was 3 (satisfactory). Most patients were recruited from a cardiology ward. Details of patients’ characteristics are summarized in Table 3.
Item analysis
The response pattern, mean value, SD, median and interquartile ranges for all items are displayed in Table 4 (ICSA) and 5 (ISCB). Mean values for the total ICSA-scale ranged from 2.9 to 4.4 and 3.4 to 4.7 for the ICSB. The median ranged from 3 to 5 for both scales. Not all items were normally distributed. One item in the ICSA (Item 3) and seven items in the ICSB (Items 3, 12–17) showed answer distributions with more than 50% of the answers assigned to the upper extreme of the Likert Scale (“Fully agree”).
  | Table 4 Response to each item and total score of the ICSA |
  | Table 5 Response to each item and total score of the ICSB |
Inter-item correlations ranged from 0.22 to 0.78 for the ICSA and from 0.16 to 0.83 for the ICSB.
Construct validity
Structural validity
Fit indices for proof of ICSA/ISCBs’ unidimensionality are displayed in Table 6. For the ICSA all fit indices reached the threshold for at least moderate model fit. For the ICSB the Tucker-Lewis Index was lower than 0.9.
Known-groups validity
Differences among the different nursing systems regarding ICSA and ICSB were only detected in the ICSB. The Kruskal–Wallis test revealed P-values of 0.07 and 0.03 for differences in ICSA and ICSB, respectively. ISCA and ISCB scores differed between patient-oriented care and zone nursing on a statistically significant level (ICSA: P=0.02; ICSB: P=0.01). There were no statistical differences in ICSA and ICSB scores between task-oriented nursing care and zone nursing (ICSA: P=0.64; ICSB: P=0.33) and task-oriented nursing care and patient-oriented care (ICSA: P=0.23; ICSB: P=0.52). Patients perceived their care as most individualized within a patient-oriented care model (Table 7).
We observed statistically significant differences in patients’ perceptions of individualized care depending on their perceptions of the decision-making process. ICSA and ICSB differed across the three modes of the decision-making process: paternalistic, shared, and informed (P<0.001 for ICSA and ICSB). Patients perceived their care as most individualized within the shared decision-making process (Table 8).
Criterion validity
Concurrent validity
Scores on the part of the Smoliner Scale which assesses patients’ perceptions of the information exchange and deliberation process ranged from 5 to 30 with a mean score of 25.33 (SD: ±5.21). Significant correlations between ICSA/ICSB and this part of the “Experience” subscale in the Smoliner Scale were as we had hypothesized. Pearson’s r was 0.66 (P<0.01) for the correlation between ICSA and the Smoliner Scale, indicating a medium correlation. ICSB and the Smoliner Scale correlated highly (r=0.72, P<0.01).
Internal consistency
Corrected item-total scale correlation ranged from 0.49 to 0.81 for the ICSA and from 0.34 to 0.82 for the ICSB. Cronbach’s alpha for the ICSA and ICSB were 0.95 and 0.93, respectively. Alpha for the subscales ranged from 0.77 (PersB) to 0.92 (ClinB) (Table 9).
  | Table 9 Internal consistency values of scales and subscales |
Discussion
This is the first study assessing validity and reliability of the German version of the ICS in a somatic clinical setting and demonstrating psychometric properties that indicate the use of the ICS for practice and research. Our data support the hypothesis of unidimensionality of the ISCA and ISCB and scales and subscales revealed moderate to excellent internal consistency. Furthermore, convergent and known-groups validity as well as concurrent validity were confirmed.
The distribution of items was not normal and some items presented answer distributions with more than 50% of the answers allocated to “Fully agree”, reflecting the upper extreme of the Likert Scale. These items mostly reflect patients’ perceptions of their control over decisions regarding nursing care; the response pattern on the DecB subscale (Items 12–17) in particular suggests that patients perceived their control over the decision-making process in nursing care as very high. This is in line with other studies wherein those items achieved the highest mean values.16,17 In consequence, after implementing PCNC strategies, changes in patients’ perceptions of individualized nursing care, especially regarding their control over nursing care decisions, might be difficult to measure (ceiling effect).
The unidimensionality of the ICSA and ICSB could be confirmed by confirmatory factor analysis. At least three of four fit indices attained the necessary threshold to indicate model fit for both scales. According to the matrix of Ponterotto and Ruckdeschel,27 alpha values indicated excellent internal consistency for the scales and moderate to excellent internal consistency for the subscales. Our results are similar to those from other studies assessing the internal consistency of the ICS. As in all other studies (except for a study assessing internal consistency in a Finnish-patient population)17, Cronbach’s alpha of the ClinB subscales shows the lowest alpha, followed by the alpha-value of the DecB subscale. Although deleting Item 3 in the ICSA and ICSB would increase Cronbach’s alpha we decided to keep this item for the following reasons. Some authors suggest that alpha should be at least 0.7 but should not exceed 0.9.26 An alpha value exceeding 0.9 might be an indicator of redundancies in measuring intended construct within items. However, to assess a construct, items should measure a broad range of construct indicators. In our case, deleting Item 3 would have increased alpha, however, we worried that this would lead to a decrease in content validity. In addition, we doubt that an increase in alpha would really improve the scale.
In line with our hypothesis, our findings indicate that the highest level of individualized care was experienced in a patient-oriented care setting. It was surprising to observe, however, that the second highest level of perceived individualization in nursing care took place in task-oriented nursing care systems, which tend to be regarded as the least patient-centered. From our clinical experience, one explanation for this result is that in task-oriented nursing care systems the same nurses fulfill the same tasks for quite a long period of patients’ hospital stay and that the patient thus perceives this as a sort of continuity in nursing care. In addition, in task-oriented nursing care systems, one nurse, in general the head nurse, has case responsibility for all patients, which also might contribute to patients’ perceptions of care continuity. Even though these differences in perceived individualization of nursing care are related significantly to the nursing care system, it is questionable whether a difference in ICSB scores of 0.09 (patient-oriented care versus task-oriented nursing care) to 0.24 (zone nursing versus patient-oriented care) within a theoretical range of 0 to 5 is clinically relevant. Further studies will have to be implemented to investigate this issue in greater depth.
Regarding the different stages in the decision-making process about nursing care, it turned out that our patients perceived their care as most individualized when decisions about nursing care were made together with the nurse (shared decision-making), followed by a paternalistic and informed decision-making style. Perhaps patients feel a bit overwhelmed if they have to decide about their nursing care on their own, even though they have received all the necessary information. Sharing the burden of decision-making might be seen as being a more individualized nursing-care approach by taking a patient’s uncertainty about what is the right decision into account. This assumption is reinforced by study results about shared decision-making in nursing care showing that patients prefer to adopt a more passive role in the decision-making process.30–32
Concurrent validity was assessed calculating the correlation between the ICSA/ICSB and a Smoliner Scale subscale reflecting patients’ perceptions of the information exchange and deliberation process in nursing care. Pearson’s r indicates a medium correlation on a statistically significant level, confirming our hypothesis. There are similarities in the meaning of individual items on the ICSB and the Smoliner Scale which account for the high correlation. However, the items do not have the same wording. For example, one item on the ICSB and the Smoliner Scale assessed the consideration of patients’ everyday activities within nursing care, (ISCB: “My everyday activities [eg, work, leisure activities] have been taken into account in my care”; Smoliner Scale “I was able to inform the nurse about my everyday activities and experiences with nursing care”).
Strengths
We conducted a study to assess aspects of validity and reliability of the German version of the ICS for use in somatic hospital settings. Our large sample consisting of more than 600 patients from different hospitals and different wards ensures reliable estimates.
Furthermore, we assessed construct validity of the ICS in terms of validity with known groups, a method that has not been applied to assess the validity of the ICS until now.
Limitations
To assess construct validity and criterion validity we used other instruments inter-related with the ICS. Evidence of construct validity and criterion validity were attainable if the related instruments were valid. Otherwise, if related instruments were biased, the interpretation of correlation results must be questioned. Porter33 called this the “correlation fallacy in validity research”. Although we try to use instruments that have been sufficiently tested for validity we cannot exclude a systematic validity bias within these instruments.
In our study, test–retest reliability as part of the evidence of ICS’s reliability was not assessed. Although there is no gold standard regarding the optimal time interval to measure test–retest reliability, Streiner and Norman26 suggest that using a time interval of 2 to 14 days is acceptable. To assess patients’ perceptions about individualized care during their entire hospital stay, the ICS should be filled out immediately before discharge. To assess test–retest reliability, patients would have had to fill out the questionnaire for the second time at home, a different situation that would result in a change in their perception of nursing care. Therefore, we decided not to assess test–retest reliability. Although this decision is understandable, some might consider it as a limitation of this study.
A further limitation is that we had a relatively high percentage of non-responders and questionnaires with missing values exceeding 20% in one of the three scales we used (ICSA/ICSB/Smoliner Scale).
Conclusion
The results of this study provide evidence of the validity and reliability of the German version of the ICS. In addition, due to similar results regarding construct validity and internal consistency, equivalence with the original version can be assumed.
Furthermore, this study provides nurses with evidence that individualized care depends on the nursing care delivery system and how patients are supported in their decision-making process about their care. A patient-oriented nursing care delivery system (eg, primary nursing) and a decision-making process in which the patients receive all the important information they need and in which they feel supported in their decision-making seem to foster individualized care. However, to determine factors influencing perceived individualized care, further studies should be conducted.
Acknowledgments
We would like to thank all the participating patients for their cooperation. We are also deeply grateful to all the nurses who recruited patients for this study, and to the nursing directors at participating hospitals for giving us the opportunity to conduct this study.
Funding
The study was funded by the young scientists’ program of the German network “Health Services Research Baden-Württemberg” of the Ministry of Science, Research and Arts, in collaboration with the Ministry of Employment and Social Order, Family, Women and Senior Citizens, Baden-Württemberg, Germany.
The article processing charge was funded by the German Research Foundation (DFG) and the Albert Ludwigs University Freiburg in the funding programme Open Access Publishing.
Disclosure
The authors have no conflict of interest to declare.
References
International Alliance of Patients’ Organizations (IAPO). What is Patient-Centred Healthcare? A Review of Definitions and Principles. London: IAPO; 2007. Available from: http://iapo.org.uk/sites/default/filesfiles/IAPO%20Patient-Centred%20Healthcare%20Review%202nd%20edition.pdf. Accessed February 22, 2015. | ||
World Health Organization Europe. Towards people-centred health systems: An innovative approach for better health outcomes. Copenhagen: WHO Europe; 2013. | ||
Lauver DR, Ward SE, Heidrich SM, et al. Patient-centered interventions. Res Nurs Health. 2002;25(4):246–255. | ||
Morgan S, Yoder LH. A concept analysis of person-centered care. J Holist Nurs. 2012;30(1):6–15. | ||
Poochikian-Sarkissian S, Sidani S, Ferguson-Pare M, Doran D. Examining the relationship between patient-centred care and outcomes. Can J Neurosci Nurs. 2010;32(4):14–21. | ||
Sidani S. Effects of patient-centered care on patient outcomes: An evaluation. Res Theory Nurs Pract. 2008;22(1):24–37. | ||
Suhonen R, Papastavrou E, Efstathiou G, et al. Patient satisfaction as an outcome of individualised nursing care. Scand J Caring Sci. 2012;26(2):372–380. | ||
Wolf DM, Lehman L, Quinlin R, Zullo T, Hoffman L. Effect of patient-centered care on patient satisfaction and quality of care. J Nurs Care Qual. 2008;23(4):316–321. | ||
Suhonen R, Välimäki M, Katajisto J, Leino-Kilpi H. Provision of individualised care improves hospital patient outcomes: an explanatory model using LISREL. Int J Nurs Stud. 2007;44(2):197–207. | ||
Köberich S, Farin E. A systematic review of instruments measuring patients’ perceptions of patient-centred nursing care. Nurs Inq. Epub 2014 Sep 12. | ||
Suhonen R, Välimäki M, Katajisto J. Developing and testing an instrument for the measurement of individual care. J Adv Nurs. 2000;32(5):1253–1263. | ||
Suhonen R, Välimäki M, Katajisto J. Individualized care in a Finnish healthcare organization. J Clin Nurs. 2000;9(2):218–227. | ||
de Witte L, Schoot T, Proot I. Development of the client-centred care questionnaire. J Adv Nurs. 2006;56(1):62–68. | ||
Radwin L, Alster K, Rubin KM. Development and testing of the Oncology Patients’ Perceptions of the Quality of Nursing Care Scale. Oncol Nurs Forum. 2003;30(2):283–290. | ||
Smoliner A, Hantikainen V, Mayer H, Ponocny-Seliger E, Them C. Entwicklung und testtheoretische Analyse eines Erhebungsinstruments zu Präferenzen und Erleben von Patienten in Bezug auf die Beteiligung an pflegerischen Entscheidungen im Akutspital. [Development and test-theoretical analysis of an instrument for data collection on patients’ preferences and experiences concerning participation in nursing care decisions in acute hospitals]. Pflege. 2009;22(6):401–409. German. | ||
Petroz U, Kennedy D, Webster F, Nowak A. Patients’ perceptions of individualized care: evaluating psychometric properties and results of the Individualized Care Scale. Can J Nurs Res. 2011;43(2):80–100. | ||
Suhonen R, Berg A, Idvall E, et al. Adapting the Individualized Care Scale for cross-cultural comparison. Scand J Caring Sci. 2010;24(2):392–403. | ||
Suhonen R, Efstathiou G, Tsangari H, et al. Patients’ and nurses’ perceptions of individualised care: an international comparative study. J Clin Nurs. 2012;21(7–8):1155–1167. | ||
Pöhler A. Übersetzung und psychometrische Überprüfung der Individualized Care Scale (ICS) [Translation and psychometric testing of the Individualized Care Scale (ICS)]. Berlin: Department of Nursing Science, Charite – Universitätsmedizin Berlin; 2010. | ||
Suhonen R, Leino-Kilpi H, Välimäki M. Development and psychometric properties of the Individualized Care Scale. J Eval Clin Pract. 2005;11(1):7–20. | ||
Abderhalden C, Boeckler U, Schippers A, et al. Ein Instrument zur Erfassung von Pflegesystemen (IzEP): Vorgehen bei der Intrumentenentwicklung [The development of an instrument to assess key elements of nursing care delivery systems]. Pr Inter Net. 2006;8:420–424. | ||
Tiedeman ME, Lookinland S. Traditional models of care delivery: What have we learned? J Nurs Adm. 2004;34(6):291–297. | ||
Arbeitsgruppe Instrument zur Erfassung von Pflegesystemen AG IzEP. Instrument zur Erfassung von Pflegesystemen. IzEP-Handbuch [Instrument to assess nursing care delivery systems. IzEP-handbook]. 2nd Aufl. ed. Bern: Verl. Forschungsstelle Pflege und Pädagogik, Universitäre Psychiatrische Dienste Bern; 2008. | ||
Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49(5):651–661. | ||
Hu L, Bentler P. Cutoff criteria for fit indexes in covariance struture analysis: Conventional criteria versus new alternatives. Structural Equation Modeling Multidisciplinary Journal. 1999;6(1):1–55. | ||
Streiner D, Norman G. Health Measurement Scales: A practical guide to their development and use. 4th ed. ed. Oxford: Oxford University Press; 2008. | ||
Ponterotto JG, Ruckdeschel DE. An overview of coefficient alpha and a reliability matrix for estimating adequacy of internal consistency coefficients with psychological research measures. Percept Mot Skills. 2007;105(3 Pt 1):997–1014. | ||
Bühl A. SPSS Version 16. Einführung in die moderne Datenanlyse [SPSS Version 16. Introduction to modern data analysis]. 11. aktualisierte Aufl. ed. Hallbergmoos: Addison-Wesley Verlag; 2008. | ||
Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745. | ||
Abrahamsen C, Draborg E, Norgaard B. Patient participation – to what extent? A survey of patients’ perceptives. Journal of Nursing Education and Practice. 2014;4(10):101–108. | ||
Florin J, Ehrenberg A, Ehnfors M. Patient participation in clinical decision-making in nursing: A comparative study of nurses’ and patients’ perceptions. J Clin Nurs. 2006;15(12):1498–1508. | ||
Smoliner A, Hantikainen V, Mayer H, Ponocny-Seliger E, Them C. Präferenzen und Erleben von Patienten zur Beteiligung an pflegerischen Entscheidungen im Akutspital – Eine Analyse der Übereinstimmung von Präferenz und Erleben sowie der Einflussfaktoren bezogen auf verschiedene Entscheidungstypen. [Patients’ preferences and experience regarding participation in nursing care decisions in acute hospitals – an analysis of conformity of preferences and experience, and factors influencing different types of decision making]. Pflege. 2009;22(6):411–419. German. | ||
Porter S. Do college students surveys have any validity? Rev High Educ. 2011;35(1):45–76. | ||
Suhonen R, Leino-Kilpi H, Välimäki M. Development and psychometric properties of the Individualised Care Scale. J Eval Clin Pract. 2005;11(1):7–20. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




