Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
The Efficacy, Feasibility And Acceptability Of A Remotely Accessible Use Of CIRCuiTS, A Computerized Cognitive Remediation Therapy Program For Schizophrenia: A Pilot Study
Authors Palumbo D, Mucci A , Giordano GM, Piegari G , Aiello C, Pietrafesa D, Annarumma N, Chieffi M, Cella M, Galderisi S
Received 2 July 2019
Accepted for publication 29 August 2019
Published 8 November 2019 Volume 2019:15 Pages 3103—3113
DOI https://doi.org/10.2147/NDT.S221690
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Davide Palumbo,1 Armida Mucci,1 Giulia Maria Giordano,1 Giuseppe Piegari,1 Carmen Aiello,1 Daria Pietrafesa,1 Nicola Annarumma,1 Marcello Chieffi,1 Matteo Cella,2 Silvana Galderisi1
1Department of Psychiatry, University of Campania Luigi Vanvitelli, Naples, Italy; 2Institute of Psychiatry, Psychology and Neuroscience (ioppn), King’s College London, London, UK
Correspondence: Armida Mucci
Department of Psychiatry, University of Campania Luigi Vanvitelli, L.go Madonna delle Grazie 1, 80138 Naples, Italy
Tel +39-81-5665153
Email [email protected]
Introduction: The Computerized Interactive Remediation of Cognition – Training for Schizophrenia (CIRCuiTS) is a form of cognitive remediation therapy developed to target neurocognitive and metacognitive deficits of people with schizophrenia, which have a detrimental impact on real-life functioning. The English version of CIRCuiTS demonstrated good acceptability and feasibility. A recent randomized controlled trial provided evidence that the program improves memory and functioning, and that the impact on functional outcome is mediated by metacognition. The next steps in the development of CIRCuiTS include both: 1) the translation and adaptation of the program in different cultural settings; and 2) the demonstration of feasibility, acceptability and effectiveness of a standardized method to administer CIRCuiTS remotely.
Purpose: To implement the CIRCuiTS Italian version and to assess acceptability, feasibility and efficacy of a standardized method to administer CIRCuiTS remotely.
Methods: Participants were assessed at baseline and received up to 40 CIRCuiTS therapy sessions, three times a week, for about 1 hr over a three-month period. Participants were reassessed post-treatment.
Results: The program demonstrated good feasibility and high acceptability when assessed by the number of dropouts and evaluation of patients’ satisfaction. Participants improved in learning, speed of processing, working memory and executive control. They showed a reduction in disorganization and improvement in self-esteem, functional capacity, and real-life functioning.
Conclusion: In this study, a standardized protocol for using CIRCuiTS from home was implemented. The first set of data showed in the paper is encouraging. The proposed procedure could lead to a dropout reduction while maintaining the efficacy of the program.
Keywords: cognition, cognitive training, metacognition, real-life functioning
Introduction
Cognitive impairment is considered a core feature of schizophrenia.1–5 Deficits in several cognitive domains are present at the onset of the disorder and are relatively stable throughout the course of the disease. Cognitive impairment is also considered a prodromal factor of the disease, suggesting that early cognitive remediation intervention may improve the prognosis.6 Meta-analytic results demonstrate that, unlike available pharmacological treatments, cognitive remediation in people with schizophrenia has beneficial effects on cognition, which generalize to real-life functioning, especially when associated with other psychological interventions.7,8 Recently, mechanisms underlying the positive effects of cognitive remediation have been explored.9 One of the factors proposed to mediate and facilitate the transfer of the therapeutic gains to real-life functioning is an improvement in metacognition.10,11 This cognitive domain is defined as the ability to understand own cognitive skills (metacognitive knowledge) and to regulate the application of these skills to real-life tasks (metacognitive regulation or executive control).12,13 Several studies have demonstrated deficits of metacognition in patients with psychotic disorders, and an association of these deficits with poor real-life functioning.14,15 In light of these findings, a new cognitive remediation intervention focusing on the development of metacognitive skills has recently been developed: Computerized Interactive Remediation of Cognition – Training for Schizophrenia (CIRCuiTS). CIRCuiTS provides the possibility to administer the program remotely, in order to avoid dropouts and reduce program implementation cost. The patient can practice at home and the therapist can monitor the progress of the CIRCuiTS training sessions by accessing patients’ profile remotely. Acceptability and feasibility of the English version of CIRCuiTS were evaluated in previous investigations.16,17 Encouraging findings from a randomized controlled trial (RCT) demonstrated that CIRCuiTS improves memory and functioning compared to treatment as usual and that the impact on functional outcome might be mediated by executive control.18 In this RCT study, the therapists administered CIRCuiTS remotely according to their clinical judgment, therefore no data are available on the acceptability, feasibility and efficacy of a standardized protocol to provide CIRCuiTS remotely.
For these reasons next steps in the development of CIRCuiTS include 1) the validation of a standardized protocol to administer CIRCuiTS remotely and 2) the demonstration of CIRCuiTS feasibility and acceptability in different cultural and linguistic settings in order to conduct further studies to test its efficacy using large-scale multinational randomized controlled trials.
In the light of this background, we 1) translated and adapted the program for the Italian context and 2) implemented a protocol to administer CIRCuiTS from home in order to assess its feasibility, acceptability and effectiveness.
Methods
Design
The first step of the study was the translation and adaptation of the CIRCuiTS Italian version. The translation was performed in collaboration with Spika, the company that built the English version of the program and provided the manual for translation (Circuits 2.0 Translation Manual). During the first phase of the translation procedure, a psychiatrist of our University Department received an accurate CIRCuiTS training at King’s College in London. After about 3 months of training, the psychiatrist, in collaboration with a psychologist and a psychiatric rehabilitation technician, adapted the translation at our University Department. Where possible it consists in a faithful translation, while in other cases it was necessary to adapt the content to the Italian context.
Successively participants were recruited and assessed at baseline (neuropsychological and clinical assessments) and then received up to 40 therapy sessions, three times a week, for about 1 hr. The training lasted for approximately 3 months and participants were reassessed at post-treatment on the same neuropsychological and clinical variables.
In the first 3 weeks, the therapist helped patients use the program to optimize the comprehension of the software. Subsequently, one session per week was independently handled by the patient from their home.
Participants
Participants were recruited from the outpatient unit for Schizophrenia spectrum disorders of our University Department of Mental Health. The inclusion criteria for the study were: 1) age between 18 and 55 years 2) confirmed DSM-IV diagnosis of schizophrenia 3) a stable clinical status, as evaluated with validate scales, that permitted reliable cognitive assessment (patients did not show acute psychotic symptoms that may have affected the neuropsychological testing); and 4) verified cognitive impairment assessed with a neuropsychological test battery. The exclusion criteria were: 1) brain and metabolic disorders known to cause neuropsychological impairments; 2) substance dependence within the last 6 months; and 3) IQ below 70.
This study was approved by the ethics committee of the University of Campania “Luigi Vanvitelli” Hospital and participants provided a written informed consent, after a comprehensive explanation of the study procedures. All study procedures were in accordance with the Declaration of Helsinki.
Materials
Neuropsychological Assessment
Neurocognitive functions were rated using the MATRICS Consensus Cognitive Battery (MCCB) which includes tests assessing different cognitive domains.19,20 Assessed domains included processing speed, attention/vigilance, working memory, visual learning, verbal learning, reasoning and problem solving and social cognition. Standardized T-scores for each domain and for the neurocognitive composite index were used in the analyses. Cognitive flexibility was evaluated using the Wisconsin Card Sorting Test (WCST), computerized version.21 This task assesses abstract reasoning and cognitive flexibility. The WCST performance measures include categories achieved, perseverative errors and non-perseverative errors. In this study, numbers of categories achieved, perseverative errors and total errors were used to assess cognitive flexibility. For perseverative errors and total errors, higher scores indicate worse performance.
Functional Capacity Assessment
Functional capacity was evaluated by the short version of the University of California San Diego (UCSD) Performance-based Skills Assessment Brief (UPSA-B),22 a performance-based instrument that assesses “financial skills” (counting money and paying bills) and “communication skills” (to dial a telephone number for emergency or reschedule an appointment by telephone). The total score, ranging from 0 (worst functional capacity) to 100 (best functional capacity), was used in the analyses.
Self-Esteem Assessment
Self-esteem was evaluated using the Self-Esteem Rating Scale (SERS), a 40-item self-rating scale with scores in the range −120 to 120, with higher scores denoting higher self-esteem.23
Psychopathological Assessment
The Positive And Negative Syndrome Scale (PANSS) was used to rate symptom severity. For this study, we used the five-factor solutions proposed by Wallwork et al,24 this includes dimensions such as “disorganization” (sum of the scores on Conceptual Disorganization, Poor Attention and Difficulty in Abstraction), “positive symptoms” (sum of the scores on Delusions, Hallucinatory Behavior, Grandiosity, Unusual thought content) and “negative symptoms” (sum of the scores on Blunted affect, Emotional withdrawal, Poor rapport, Passive/apathetic social withdrawal, Lack of spontaneity and flow of conversation, Motor retardation).
Real-Life Functioning Assessment
Real-life functioning was assessed using the Specific Level of Functioning Scale (SLOF), a hybrid instrument that examines several aspects of functioning. This measure is based on key caregiver’s judgment on behavior and functioning of patients and consists of 43 items including six domains: physical efficiency, self-care, interpersonal relationships, social acceptability, community activities (e.g., shopping, using public transportation), and working abilities. According to Sabbag et al25 the “physical efficiency” dimension was not used in this study both because ceiling effects was expected and because it did not assess everyday functioning. The Italian version of the scale was validated as part of the Italian Network for Research on Psychoses activities.26 For this scale, the higher the total score, the better the overall functioning of the subject (total score ranges from 43=poorest functioning to 215=best functioning).
User Satisfaction
To evaluate the participants’ level of satisfaction with the treatment, the Client Satisfaction Questionnaire-8 (CSQ-8) was used. Scores for this measure range between 8 and 32, with a higher score indicating greater satisfaction.27
Intervention
Computerised Interactive Remediation of Cognition Training for Schizophrenia “CIRCuiTS” is a computerized cognitive therapy program for people with a diagnosis of schizophrenia or schizoaffective disorder.17,28 It is a psychological treatment aimed at improving cognitive functioning and metacognitive skills. It does not have the purpose of directly addressing the content of thought, beliefs or emotions but, through the use of non-emotional material, teaches basic thinking skills that could facilitate more complex social behaviors and life skills. CIRCuiTS uses a variety of techniques, such as errorless learning and scaffolding, which, according to empirical studies, contribute to improving cognitive performance.28 CIRCuiTS aims to enhance cognitive abilities including long-term memory; working memory, attention, problem-solving, speed of processing, comprehension, flexibility of thought, and planning. Specifically, CIRCuiTS targets metacognitive difficulties by helping clients to improve their metacognitive knowledge (knowledge of their cognitive skills) and metacognitive regulation (the ability to monitor and control the application of cognitive skills). Metacognitive difficulties are explicitly targeted through specific software and therapy components. Metacognitive regulation is encouraged by asking the participant to develop a plan, to estimate the difficulty before beginning a task than monitor and finally review task performance. In particular, before each task, the participant rates the difficulty of the task, estimates how long the task will take and identifies strategies to complete the task. After the task, the participant sees his/her scores and rates how difficult he/she found the task and how useful he/she found the selected strategy. CIRCuiTS allows both to exercise in a safe environment to improve neurocognitive skills and to increase the awareness of own cognitive abilities and finally to structure useful strategies to transfer these skills from laboratory to the real world.
CIRCuiTS includes a maximum of 40 sessions, with a frequency of 3 sessions per week. Each session lasts about 1 hr; however, as participant concentration may be limited, due to attentional impairment, the session duration can be shorter for the initial sessions and gradually increased over sessions, to match the subject’s improvement in attention. Each session includes a series of tasks (usually about 4 to 8) that target different cognitive domains. Each task may concern verbal or nonverbal skills or both. The workflow can be modified, and tasks can be repeated or skipped to individualize therapy to the subjects’ needs.
CIRCuiTS provides: 1) Abstract tasks that use abstract material and are designed to improve some cognitive functions in an abstract context (for example, numbers or geometrical shapes); and 2) complex tasks designed to be more “ecological”, i.e., similar to activities that could be carried out in everyday life (e.g. planning a trip or a meal, reading a letter, or recalling a shopping list). There are up to 15 difficulty levels for each task; the program presents first the lowest and gradually progresses to the highest levels, depending on their performance CIRCuiTS automatically regulates the level of difficulty for individual users using a built-in algorithm. This is done to maintain performance positive feedback high. The program is based on the rationale that neurocognitive abilities learned in an abstract context can be gradually incorporated into real-life activities through the training of metacognitive skills and the development of new behavioral strategies. The ultimate goal is that the trained subjects gradually transfer the acquired cognitive skills to daily life.
Sessions are supported by a therapist whose role is to support the implementation of the program components and to support the clients' motivation.
Home Sessions
In our study, the CIRCuiTS program included an initial period (3 weeks) in which the therapist and patient met 3 times a week for 1 hr. After 3 weeks (period of time in which the patient could become able to use the program autonomously) the patient met the therapist in two weekly sessions and in one session the patient carried out CIRCuiTS independently from the home computer. The duration of the home session is similar to the session length received at the hospital. The therapist can monitor the client’s progress on the software by accessing the subject’s user profile remotely. The patient is required to note any difficulties encountered in performing the exercises and discuss them in the next meeting with the therapist. The ability to carry out tasks autonomously is designed both to facilitate access to training for patients who have greater difficulty in reaching the clinic, to promote autonomy and to reduce the program implementation cost. The rationale adopted to promote this method (1/3 session from home and not 2/3 sessions from home) is due to: 1) the importance of the therapist–patient relationship to promote new cognitive strategies and their generalization29 2) the importance of the therapist–patient relationship to promote and maintain the patient’s motivation.29–31
Procedure
Potential participants were identified via the outpatient unit for Schizophrenia spectrum disorders of our University Department of Mental Health. If the inclusion criteria were met, and the participants signed the informed consent, a psychiatrist and a psychologist completed neuropsychological and clinical baseline evaluations. Two psychiatric rehabilitation technicians conducted the therapy for 4 patients each. Psychiatric rehabilitation technicians were trained by a psychiatrist from our research group, expert in cognitive remediation, who was trained at King’s College in London for 2 months and was involved in the Italian translation and adaptation of the program. Participants maintained their usual pharmacological treatment regime (e.g., antipsychotic medication) throughout the study. After the therapy sessions were completed, the same baseline evaluator administered the post-treatment neuropsychological evaluation and clinical assessment.
Statistical Analysis
The proportion of recruited service users who agreed to participate in the study, together with attendance and attrition rates, was recorded and represented the indicators of intervention feasibility.
Acceptability was assessed through the user satisfaction questionnaire. Measures of cognition, self-esteem, psychopathology, functional capacity and real-life functioning was assessed to evaluate the effectiveness of the program.
For the MCCB cognitive indices (speed of processing, attention/vigilance, working memory, verbal learning, visual learning, reasoning and problem solving, social cognition and neurocognitive composite score) T-scores were calculated by the MCCB Computer Scoring Program with correction of the raw scores by age and gender based on the normative Italian data32 Using this standardization method, all test scores, domain scores, and the composite scores are standardized to the same measurement scale with a mean of 50 and SD of 10.
The numbers of categories achieved, total errors and perseverative errors on the Wisconsin Card Sorting test were obtained by the E.M.S. software Test System v1.0.12 produced by the E.M.S. srl. in Bologna, Italy.33 Scores of functional capacity, self-esteem and real-life functioning were obtained as the sum of their respective items.
As to psychopathological indices the PANSS scores for positive, negative and disorganization dimensions were calculated from the sum of the individual items included in the respective dimension by the consensus factor analysis by Wallwork et al.24
Student’s t-test for the same sample was used to test pre-post treatment changes.
If the efficacy of the program will be confirmed, a correlation analysis will be conducted in order to assess which variables (cognition, self-esteem, symptomatology) are correlated with the improvement of functioning (functional capacity and real-life functioning). First, only variables with a significant post-intervention change will be analyzed. Second, it will be analyzed the amount of change of each variable between the pre and post (with a subtraction: post-pre). Finally, the changes in each variable will be correlated with changes in real-life functioning domains and functional capacity.
For all statistical tests, the level of significance was set at p<0.05. All the analyses have been conducted using STATISTICA version 10.
Effect size (Cohen’s d) for post- vs pre-training score changes was calculated as the mean difference between the pre-treatment and post-treatment scores, divided by the standard deviation, taking into account the association between pre and post-treatment scores.34
Results
Ten participants affected by schizophrenia were found to be eligible for the study, eight (80%) consented to participate. Two out of 8 had never participated in any rehabilitation intervention. The remaining 6 had participated in different types of rehabilitation interventions (social skills training, other cognitive remediation interventions, psychoeducation). These other interventions were completed at least 18 months before starting the present study. The baseline characteristics and medication status of the sample are presented in Table 1. Participants attended an average of 37.5 sessions to complete the program (min 29, max 40). Of these, 30.3% were carried out from home (91 out of 300 total sessions). At baseline, participants performed on average 1 ½ to 3 ½ SD below the normative mean (Table 1), indicating moderate to large impairment on MCCB domains. The mean number of total errors and perseverative errors on WCST were in the range of moderate impairment (about 1 SD above the normative mean).
 |
Table 1 Baseline Characteristics And Medication Status (N=8) |
Feasibility
In total, 10 patients were assessed as eligible and were offered the therapy. Eight consented to participate (80%). Two patients refused to participate due to the distance between their home and the Department of Mental Health. All the remaining 8 subjects completed the intervention program. Figure 1 illustrates the recruitment process, therapy completion and dropouts.
 |
Figure 1 Consort diagram. |
Acceptability
The participants’ average score reported for CIRCuiTS on the CSQ was 29.3 indicating a high level of satisfaction according to Kelly et al 2018.35
Effectiveness
Neurocognitive Indices
Compared to baseline, post-treatment scores were significantly improved for the MCCB Neurocognitive composite (t(7)=−4.35, p<0.01), as well as for the following domains: speed of processing (t(7)=−5.27, p<0.01), working memory (t(7)=−3.03, p<0.02), verbal learning (t(7)=−2.46, p<0.05) and visual learning (t(7)=−2.37, p<0.05) (Figure 2). Post-treatment total errors (t(7)=2.85, p<0.05) and perseverative errors (t(7)=2.53, p<0.05) on the WCST were also significantly reduced with respect to baseline, while the number of categories achieved did not show a statistically significant change (Figure 3).
 |
Figure 3 Treatment effects on Wisconsin Card Sorting Test. Notes: *Significant improvement post-treatment (p<0.05). The y-axis shows the WCST-score. |
The confidence interval and the effect size of these changes in neurocognitive scores are reported in Table 2. The MCCB neurocognitive pre and post-treatment scores of each subject are presented in Table 3. All but one subject (Case 7) improved by at least 0.5 to 1 SD in at least 2 cognitive domains. In four subjects there was a change in severity level (from moderate-severe to absent-mild) in 1 or more domains.
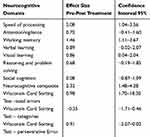 |
Table 2 Pre-Post Treatment Effect Size On Neurocognitive Domains |
Functional Capacity
The UPSA-B total score showed a significant improvement at the end of the cognitive remediation program, with respect to baseline (t(7)=−7.65, p<0.01; effect size=2.72) (Table 3).
Self-Esteem
A significant improvement of the self-esteem, evaluated by SERS, was also found (t(7)=−3.1, p<0.02; effect size=1.13) (Table 4).
 |
Table 4 Treatment Effects On Functional Capacity, Self-Esteem And Symptomatology |
Psychopathological Indices
A significant improvement was observed on the PANSS disorganization dimension after the intervention (t(7)=3.52, p<0.01; effect size=1.88). No significant effect was found for the other PANSS dimensions, although there was a mild reduction of the negative symptom dimension (Table 4).
Real Life Functioning
After the end of the intervention, a significant improvement of real-life functioning, as assessed by the SLOF total score, was observed (t(7)=−3.54; p<0.01). Considering the change in each SLOF subscale, significant improvements of “self-care” (t(7)=−3.66; p<0.01), “interpersonal relationships” (t=−3.32; p<0.02), “social acceptability” (t=−3.64; p<0.01) and “working abilities” (t(7)=−4.10; p<0.01) were found (Table 5).
 |
Table 5 Treatment Effects On Real-Life Functioning |
Correlation Analysis Between Changes In Functioning, Functional Capacity, Cognition, Self-Esteem And Disorganization
The correlation analysis showed no correlation between the SLOF total or domain score improvement and any other significantly improved variable. For the correlation between UPSA-b total score and the other variables, only the MCCB composite showed a significant correlation (r=0.709, p<0.05, Table 6).
 |
Table 6 Correlational Analysis Between Variables Showing Significant Improvement Post-Treatment |
Discussion
This study aimed to implement the CIRCuiTS Italian version and to assess the acceptability, feasibility and efficacy of a standardized method to administer the program remotely. The results showed that the Italian version of the program administered according to our protocol was feasible and acceptable to service users. It suggests that the remote use may have important implications in terms of access to cognitive rehabilitation for patients with schizophrenia. Of the 10 eligible patients, 8 (80%) agreed to attend and all of them completed the treatment. It is difficult to compare this feasibility study to large-scale randomized trials present in the literature, but the absence of dropouts is an encouraging result. The two patients who refused the therapy attributed the decision to the cost of transportation from their home to the University Department, for the scheduled 2–3 weekly sessions.
Regarding acceptability, the participants evaluated the therapy as useful and satisfactory. The average CSQ score is “High” according to the table proposed by Kelly et al.35 These results are in line with previous findings from a consumer-led survey on the experience of CIRCuiTS.17,28
Our study is the first study assessing CIRCuiTS efficacy using the MCCB neurocognitive battery to analyze the results on cognitive domains. The MATRICS initiative was launched to foster the development of a cognitive consensus battery for use in clinical trials.19,20 The MCCB battery has been translated into several languages, showing a high reliability and validity of the construct.19,36–39 MCCB data show that CIRCuiTS participants improve significantly post-intervention on the neurocognitive composite score and on 4 on the 7 cognitive domains considered (Speed of Processing, Working Memory, Visual Learning and Verbal Learning). The rest of the cognitive domains (Attention/Vigilance, Reasoning & Problem Solving) did not show significant improvements but, with the exception of Social Cognition, there is a general improvement. It is very likely that the lack of statistical significance for Attention/Vigilance and Reasoning & Problem Solving is due to the better baseline performance of our patients on these compared to the other domains. The lack of changes in Social Cognition is most likely due to the absence of a targeted training for this cognitive domain in CIRCuiTS.
A general positive effect was found also for the cognitive flexibility measured by WCST perseverative errors and total errors. Our results are in line with data on the CRT effectiveness present in the literature. Indeed, CRT has shown a significant effect on the various neurocognitive domains as reported by several meta-analyses7,8 and literature data on the effectiveness and feasibility of CIRCuiTS. In fact, in a recent study16 researchers reported a moderate effect of CIRCuiTS short version (the protocol included a total of 6 sessions) on global cognition and memory in a sample of inpatients with acute psychosis. In anotherCIRCuiTS feasibility study,17 on a small sample of young adults affected by schizophrenia, emerged a positive effect of CIRCuiTS on Attention, Problem Solving and Episodic Memory. Furthermore, in the recent randomized controlled trial (CIRCuiTS vs Treatment as Usual), the participants showed a significant improvement in visual memory, maintained at 3-month follow-up with the program. In addition, CIRCuiTS was found to protect from cognitive decline.18
Our study showed a generalization of the effects also to other variables: i.e. functional capacity, self-esteem, disorganization and real-life functioning.
Interestingly, our results showed no correlation between SLOF improvement and changes in any other variables improved post-treatment. Vice versa, MCCB composite score improvement correlated with the improvement of functional capacity. These results are in line with the hypothesis that the neurocognitive skills are directly associated with functional capacity, and functional capacity could be a bridge between cognition and real-life functioning.5,40 In line with this model, CIRCuiTS could indirectly promote the improvement on the real-life functioning of the patient affected by schizophrenia.
Finally, these positive results suggest that the Italian translation of CIRCuiTS was faithful to the original and the autonomous use of the program (1 session out of 3) is feasible, acceptable and effective.
Limitations
There are a number of limitations to this pilot study. Our results are limited to the restricted number of subjects and there was no control condition. It would be necessary in the future to evaluate the effectiveness of the intervention by comparing in a randomized controlled trial the experimental group with a control group and a treatment as usual group.
A future study should also include a follow-up evaluation in order to assess the duration of treatment effects.
Conclusion
This is the first study in which the efficacy of a standardized protocol to administer the Italian version of CIRCuiTS remotely was assessed. The participants, after an accurate therapist’s training, were able to handle the program independently from home. The results showed that this protocol was feasible and well accepted by service users and confirmed the data obtained in other studies on the efficacy of the program. The autonomous use of CIRCuiTS (1/3 session) does not worsen the effectiveness of training but can reduce dropouts and implementation costs while increasing the possibility of access to treatment. Furthermore, in our pilot-study CIRCuiTS is effective also in patients with a long illness duration, who have previously been involved in other psychological treatments. A large-scale, controlled trial is needed to confirm the data of this preliminary study and to identify the patients’ profiles that are more likely to benefit from CIRCuiTS intervention.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. General sources of potential conflict of interest, considered unrelated to this work, include the following: Armida Mucci has received fees as consultant and/or advisor to Janssen Pharmaceutica NV, Gedeon Bulgaria, Pierre Fabre and Lundbeck; Silvana Galderisi has been a consultant and/or advisor to or has received honoraria or grants from: Millennium Pharmaceuticals, Innova Pharma - Recordati Group, Janssen Pharmaceutica NV, Sunovion Pharmarmaceuticals, Janssen-Cilag Polska Sp. z o.o., Gedeon Richter-Recordati, Pierre Fabre, Otsuka, Angelini. Davide Palumbo, Giulia Maria Giordano, Giuseppe Piegari, Carmen Aiello, Daria Pietrafesa, Nicola Annarumma, Marcello Chieffi and Matteo Cella reported no conflicts of interest.
References
1. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12(3):426–445. doi:10.1037/0894-4105.12.3.426
2. Elvevag B, Goldberg TE. Cognitive impairment in schizophrenia is the core of the disorder. Crit Rev Neurobiol. 2000;14(1):1–21. doi:10.1615/CritRevNeurobiol.v14.i1
3. Liddle PF. Cognitive impairment in schizophrenia: its impact on social functioning. Acta Psychiatr Scand Suppl. 2000;400:11–16. doi:10.1111/j.0065-1591.2000.007s021[dash]3.x
4. Wilk CM, Gold JM, McMahon RP, Humber K, Iannone VN, Buchanan RW. No, it is not possible to be schizophrenic yet neuropsychologically normal. Neuropsychology. 2005;19(6):778–786. doi:10.1037/0894-4105.19.6.778
5. Galderisi S, Rossi A, Rocca P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. 2014;13(3):275–287. doi:10.1002/wps.20167
6. Eack SM, Hogarty GE, Cho RY, et al. Neuroprotective effects of cognitive enhancement therapy against gray matter loss in early schizophrenia: results from a 2-year randomized controlled trial. Arch Gen Psychiatry. 2010;67(7):674–682. doi:10.1001/archgenpsychiatry.2010.63
7. McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164(12):1791–1802. doi:10.1176/appi.ajp.2007.07060906
8. Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472–485. doi:10.1176/appi.ajp.2010.10060855
9. Wykes T, Spaulding WD. Thinking about the future cognitive remediation therapy–what works and could we do better? Schizophr Bull. 2011;37(Suppl 2):S80–S90. doi:10.1093/schbul/sbr064
10. Lysaker PH, Shea AM, Buck KD, et al. Metacognition as a mediator of the effects of impairments in neurocognition on social function in schizophrenia spectrum disorders. Acta Psychiatr Scand. 2010;122(5):405–413. doi:10.1111/acp.2010.122.issue-5
11. Wykes T, Reeder C, Huddy V, et al. Developing models of how cognitive improvements change functioning: mediation, moderation and moderated mediation. Schizophr Res. 2012;138(1):88–93. doi:10.1016/j.schres.2012.03.020
12. Cella M, Reeder C, Wykes T. Group cognitive remediation for schizophrenia: exploring the role of therapist support and metacognition. Psychol Psychother. 2016;89(1):1–14. doi:10.1111/papt.12062
13. Cella M, Reeder C, Wykes T. Lessons learnt? The importance of metacognition and its implications for cognitive remediation in schizophrenia. Front Psychol. 2015;6:1259. doi:10.3389/fpsyg.2015.01259
14. Lysaker PH, Gumley A, Luedtke B, et al. Social cognition and metacognition in schizophrenia: evidence of their independence and linkage with outcomes. Acta Psychiatr Scand. 2013;127(3):239–247. doi:10.1111/acps.2013.127.issue-3
15. Medalia A, Thysen J, Freilich B. Do people with schizophrenia who have objective cognitive impairment identify cognitive deficits on a self report measure? Schizophr Res. 2008;105(1–3):156–164. doi:10.1016/j.schres.2008.07.007
16. Tsapekos D, Taylor R, Cella M. Feasibility and acceptability of brief cognitive remediation targeting metacognition in acute inpatients with psychosis: a case series. Neuropsychol Rehabil. 2017;1–15.
17. Cellard C, Reeder C, Paradis-Giroux -A-A, et al. A feasibility study of a new computerised cognitive remediation for young adults with schizophrenia. Neuropsychol Rehabil. 2016;26(3):321–344. doi:10.1080/09602011.2015.1019891
18. Reeder C, Huddy V, Cella M, et al. A new generation computerised metacognitive cognitive remediation programme for schizophrenia (CIRCuiTS): a randomised controlled trial. Psychol Med. 2017;1–11.
19. Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165(2):203–213. doi:10.1176/appi.ajp.2007.07010042
20. Kern RS, Nuechterlein KH, Green MF, et al. The MATRICS Consensus Cognitive Battery, part 2: co-norming and standardization. Am J Psychiatry. 2008;165(2):214–220. doi:10.1176/appi.ajp.2007.07010043
21. Axelrod BN, Goldman RS, Heaton RK, et al. Discriminability of the Wisconsin Card Sorting Test using the standardization sample. J Clin Exp Neuropsychol. 1996;18(3):338–342. doi:10.1080/01688639608408991
22. Mausbach BT, Harvey PD, Goldman SR, Jeste DV, Patterson TL. Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull. 2007;33(6):1364–1372. doi:10.1093/schbul/sbm014
23. Nugent WR, Thomas JW. Validation of a clinical measure of self-esteem. Res Social Work Prac. 1993;3(2):191–207. doi:10.1177/104973159300300205
24. Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the positive and negative syndrome scale for schizophrenia. Schizophr Res. 2012;137(1–3):246–250. doi:10.1016/j.schres.2012.01.031
25. Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, Harvey PD. Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophr Res. 2012;137(1–3):190–195. doi:10.1016/j.schres.2012.02.002
26. Mucci A, Rucci P, Rocca P, et al. The specific level of functioning scale: construct validity, internal consistency and factor structure in a large Italian sample of people with schizophrenia living in the community. Schizophr Res. 2014;159(1):144–150. doi:10.1016/j.schres.2014.07.044
27. Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. doi:10.1016/0149-7189(79)90094-6
28. Reeder C, Pile V, Crawford P, et al. The feasibility and acceptability to service users of CIRCuiTS, a computerized cognitive remediation therapy programme for schizophrenia. Behav Cogn Psychother. 2016;44(3):288–305. doi:10.1017/S1352465815000168
29. Cella M, Wykes T. The nuts and bolts of cognitive remediation: exploring how different training components relate to cognitive and functional gains. Schizophr Res. 2019;203:12–16. doi:10.1016/j.schres.2017.09.012
30. Saperstein AM, Medalia A. The role of motivation in cognitive remediation for people with schizophrenia. Curr Top Behav Neurosci. 2016;27:533–546.
31. Best MW, Bowie CR. A review of cognitive remediation approaches for schizophrenia: from top-down to bottom-up, brain training to psychotherapy. Expert Rev Neurother. 2017;17(7):713–723. doi:10.1080/14737175.2017.1331128
32. Mucci A, Galderisi S, Green MF, et al. Familial aggregation of MATRICS consensus cognitive battery scores in a large sample of outpatients with schizophrenia and their unaffected relatives. Psychol Med. 2017;1–10.
33. Avaialable from: http://emsmedical.net/.
34. Lenhard W, Lenhard A Calculation of effect size; Published 2016. Available from: https://www.psychometrica.de/effect_size.html.
35. Kelly PJ, Kyngdon F, Ingram I, Deane FP, Baker AL, Osborne BA. The client satisfaction questionnaire-8: psychometric properties in a cross-sectional survey of people attending residential substance abuse treatment. Drug Alcohol Rev. 2018;37(1):79–86. doi:10.1111/dar.2018.37.issue-1
36. Shi C, Kang L, Yao S, et al. The MATRICS Consensus Cognitive Battery (MCCB): co-norming and standardization in China. Schizophr Res. 2015;169(1–3):109–115. doi:10.1016/j.schres.2015.09.003
37. Rodriguez-Jimenez R, Bagney A, Garcia-Navarro C, et al. The MATRICS consensus cognitive battery (MCCB): co-norming and standardization in Spain. Schizophr Res. 2012;134(2–3):279–284. doi:10.1016/j.schres.2011.11.026
38. Kaneda Y, Ohmori T, Okahisa Y, et al. Measurement and treatment research to improve cognition in schizophrenia consensus cognitive battery: validation of the Japanese version. Psychiatry Clin Neurosci. 2013;67(3):182–188. doi:10.1111/pcn.2013.67.issue-3
39. Kenney J, Anderson-Schmidt H, Scanlon C, et al. Cognitive course in first-episode psychosis and clinical correlates: a 4 year longitudinal study using the MATRICS consensus cognitive battery. Schizophr Res. 2015;169(1–3):101–108. doi:10.1016/j.schres.2015.09.007
40. Galderisi S, Rucci P, Kirkpatrick B, et al. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry. 2016;75(4):396–404. doi:10.1001/jamapsychiatry.2017.4607
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


