Back to Journals » Clinical Ophthalmology » Volume 17
The Effect on Patients’ Visual Acuity and Grade, Secondary to Non-Attendance at Treatment Centers, Post Referral from Diabetic RetinaScreen Ireland
Authors Harmon J, Kelly S, Acheson R, Keegan D, McMahon S, Kavanagh H, O'Toole L
Received 16 September 2022
Accepted for publication 30 December 2022
Published 11 January 2023 Volume 2023:17 Pages 183—190
DOI https://doi.org/10.2147/OPTH.S388988
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Joanne Harmon,1 Stephen Kelly,2 Robert Acheson,1 David Keegan,2 Shane McMahon,1 Helen Kavanagh,2 Louise O’Toole1
1NEC Care, Cork, Ireland; 2Diabetic RetinaScreen, Heath Service Executive, Dublin, Ireland
Correspondence: Louise O’Toole, NEC Care, 55 South Mall (2nd Floor), Cork, T12 RR44, Ireland, Tel +35318858656, Fax +35318858658, Email [email protected]
Background: Patient non-attendance following referral to hospital is a significant challenge, in particular, for persons with diabetes.
Aim: We sought to determine the impact on both visual acuity and the subsequent follow-up retinopathy grade of patients when they fail to attend Diabetic Retinopathy Treatment (DRT) Centers following referral from Diabetic RetinaScreen (DRS).
Methods: A retrospective analysis of patients discharged from DRT due to multiple consecutive missed appointments between January 2016 and June 2021. Patients discharged for non-attendance were compared with patients discharged from completed treatment.
Results: Of the 24,945 NEC patients referred to DRT, 5900 (24%) and 9345 (37%) were discharged back to DRS due to non-attendance and completed treatment, respectively. Those discharged for non-attendance were younger (60.7 v 63.4, p < 0.001) and had higher proportions of males (67% v 63%, p < 0.001) and people with type 1 diabetes (27% v 18%, p < 0.001). After attending rescreening after discharge, those discharged for non-attendance were significantly more likely to have a worsening of DR grade (26% v 8%, p < 0.001).
Conclusion: Despite being notified that further investigation (with possible treatment) was required post DRS, many diabetic patients failed to attend for further management of their eye care in DRT. These patients had worse visual outcomes compared to those that attended. Improved patient education and communication are required to mitigate against the consequences of non-attendance.
Keywords: maculopathy, follow up, HES, DNA, compliance
Introduction
Diabetic retinopathy is the leading cause of preventable blindness among adults of working age worldwide.1 It is estimated that it will reach a global prevalence of 10.7% (700 million people) by 2045.2 However, diabetic retinopathy is no longer the leading cause of blindness in working age adults in either England, Wales or Iceland, secondary to the implementation of very effective retinal screening programmes.3–5 It is estimated that diabetes mellitus affects approximately 5.2% of the population of Ireland.3
Diabetic RetinaScreen was launched in Ireland in 2013 as a free service to all diabetic patients over the age of 12 years. As of 2018, 4.5% of the over 12 population was on the eligible (to be screened) register.4,5 The ratio of Type 1 to Type 2 diabetes is 1:9, and the proportion of males to females on the register is 59.8% male and 40.2% female.5 There are two service providers for DRS, both follow identical national guidelines and use the same data management software – OptoMize. At their DRS appointment, the patient’s best corrected visual acuities are obtained when wearing their usual distance correction, or if their vision is 6/9 or worse a pinhole correction method is used. Two 45-degree mydriatic digital photographs of the retina centred on the macula and the optic disc are taken. Individuals with R1M1, R2M0 and R2M1 screen-positive retinopathy and maculopathy are referred by routine pathways to their local DRT. A grade R3 when active or stable triggers an urgent referral to DRT. If there is active neovascular AMD or other urgent diagnoses such as papilloedema or retinal detachment, this generates an urgent NDED referral to DRT. Routine DRT referrals comprise glaucoma, branch or central retinal artery occlusions, branch or central retinal vein occlusions, pigmented retinal lesions, arterial emboli, and retinitis. A diagnosis of referrable diabetic retinopathy takes precedence over routine NDED when making a referral.
There is a strong relationship between good screening compliance and favourable visual outcomes.6 High non-attendance rates at DRS programmes reduce their cost-effectiveness.7 In England, there is an uptake level of 82.8% of the National Health Service Diabetic Eye Screening Programme (NHSDESP), and the uptake in Ireland is 67.2%.4,8 For comprehensive care to succeed, there must be a seamless interface between DRS and the DRT centres. Ireland should be in a good position as one of the few linked screening and treatment programmes in the world, but it does not seem to be and could be better.4 If patients do not attend their treatment appointments, then despite considerable investment in health care, the benefits of an effective screening program in detecting sight-threatening retinopathy are lost.9 The aim of this study is to investigate how patient’s eye status changed after being discharged from treatment centres secondary to non-attendance.
Materials and Methods
Study Population
This was a retrospective analysis study carried out by one of the two service providers (NEC) for DRS in Ireland. The DRS centres for photography are sited so that most patients do not have to travel more than 25 km, whereas DRT centres may be more than 200 km away.5 There are nine DRT centres in Ireland, 8 centres discharge patients after 2 consecutive missed appointments, one centre discharges patients after one single missed appointment. The analysis identified patients from January 2016 to June 2021 who were discharged from DRT for non-attendance or completed treatment. Those discharged from DRT received follow-up appointments in DRS by letter. Data were extracted from the OptoMize patient management program. This included information on age, sex, diabetes type, VA, DR grade, distance from screening to treatment centre and time between last attended appointment and re-screening. Patients were excluded from analysis if they had missing information, were labelled as NDED disease or were ungradable. The geographical area studied encompassed 17 of the more rural counties within the Republic of Ireland. Of note due to COVID 19 restrictions between March 17th and July 1st 2020, no DRS was carried out but urgent DRT care continued and routine Diabetic care was as per national guidelines.10 The list of those non-attenders was revalidated by DRS, individuals were removed who had become medically unfit, died, deconsented or who had moved outside the provider’s catchment area. For the purpose of this study, the recorded Snellen acuity was converted to LogMAR. For patients with bilateral diabetic retinopathy, the diabetic retinopathy grade in the worst eye was used for analysis.
Data Analysis
A comparative analysis of patients discharged for non-attendance and those discharged for completed treatment was carried out. The baseline characteristics of these groups (sex, age, diabetes type, etc.) were compared using appropriate statistical tests. A secondary analysis comparing the rates of VA or DR grade worsening was also carried out. A worsening DR grade was defined as an increase in the retinopathy or maculopathy grade.
All analyses were carried out in R (version 4.2.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
Population Statistics
From January 1st, 2016, up to June 30th, 2021, 24,945 NEC patients were referred from DRS to DRT. A total of 5900 (24%) of these referred patients were discharged from DRT secondary to non-attendance, and 9345 (37%) were discharged for completed treatment. Of these 15,245 discharges, only 5788 (from 5037 patients) met the inclusion criteria for study. Summary statistics of these groups can be found in Table 1. Of the total discharges, 2057 were from females and 3731 were from males.
 |
Table 1 Summary Statistics of the Study Population |
The annual non-attendance rate at DRT ranged between 12% and 29% (Table 2). In May 2021, the computer systems in multiple DRT centres fell victim to a cyberattack on the Health Service Executive. DRT had no access to OptoMize, and so very few patients were discharged. This explained the low rate of 12% in the first two-quarters of that year.
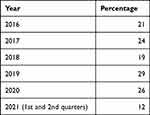 |
Table 2 Number of Patients Discharged from DRT Secondary to Non-Attendance per Annum |
The distribution of pre-discharge DR grades for both groups can be found in Figure 1. The most frequent grade in both groups was R1M1 (80% v 60% for non-attenders and treatment complete respectively), with the non-attendance group having a slightly higher proportion of worse grades. The distribution of pre-discharge VA was similar (Figure 2), with both groups having a median of 0.18 LogMAR. There was a notable difference in the post-discharge DR grades, with 87% of the treatment complete group having a grade of R1M1 or better, compared to 57% of the non-attendance group (Figure 3).
 |
Figure 1 Distribution of worst pre-discharge DR grades by discharge group, for patients included in analysis. |
 |
Figure 2 (A and B) Distribution of pre-discharge VA in right and left eyes for by discharge group. |
 |
Figure 3 Distribution of worst post-discharge DR grades by discharge group for patients included in analysis. |
Comparative Analysis
Those discharged from DRT for non-attendance differed from those discharged for completed treatment. They were on average younger (60.7 v 63.4, p < 0.001), more likely to have T1DM (27% v 18%, p < 0.001) and more likely had further to travel from screening to treatment (50.0km v 42.2km, p < 0.001). While both groups had a higher ratio of males to females, the DNA discharge group had a higher proportion (0.67 v 0.63, p < 0.001). The modal and median DR grade in both groups was R1M1. There was no difference in the pre-discharge VA between the groups.
When considering how VA and DR grade changed between discharge and re-screening, again there were statistically significant differences between the groups (Table 3). Those discharged for non-attendance were much more likely to have a worse DR grade (26% v 8%, p < 0.001). They were also more likely to have a worsening of their visual acuity in both eyes (0.38 v 0.32, p < 0.001 in left eye and 0.36 v 0.32, p = 0.02 in right eye).
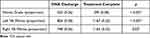 |
Table 3 Rates of Worsening DR Grade or VA After Discharge from DRT |
The distance patients would have to travel to their treatment centre was captured for 5480 patients. Of these patients, 48% had less than 50km to travel, and 14% had less than 5 km to travel to their treatment centre. The mean time between clinical encounters was 22 months (range 5–82) (Figure 4).
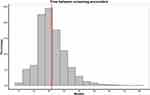 |
Figure 4 Number of months between pre- and post-discharge screening encounters for non-attenders. The red vertical bar represents the mean of 22 months. |
Discussion
This is the first study to study patients who have been discharged from diabetic retinopathy treatment centres within Ireland. We have shown that patients who are discharged from treatment centres for non-attendance have different demographics to those discharged for completed treatment. We have also shown that patients who are discharged for non-attendance are more likely to re-attend screening with worse DR grade and VA.
Non-Attendance in Diabetes Care
Comparisons between attendance at DRT after referral from DRS, with attendance rates at hospital outpatient appointments after referral from other screening programmes are not straightforward. Patients attending for cervical screening or mammography tend to be otherwise healthy and unburdened with multiple hospital clinic appointments. Conversely, screening for the diabetic patients continues for life, along with the need for their attendance at other multidisciplinary consultations. As sight is known to be valued by diabetic patients, they are willing to exchange years of remaining life for good vision.11 It would be expected that diabetic patients would be in good compliance with attendance at both the DRS and DRT programs. Often, however, this is not the case.
Wolff et al found that patients with diabetes mellitus miss one in every 20 hospital appointments.12 Philpott-Morgan et al compared non-attendance or “did not attend” (DNA) rates for outpatient hospital appointments in the NHS across different specialities. They found that hepatology ranked first (17%) followed by diabetic medicine (16%) followed by ophthalmology (15%)13 We determined the average non-attendance rate at DRT over a five-year period to be 23%. A similar value of 19% was found by Greenan et al who looked at 1200 referrals from DRS to DRT with an equivocal geographic base.14 Faes et al reported a DNA rate of 32% and 28% from DRS to HES, for face to face, and virtual consultations, respectively.15 Keenum et al found that 24% of patients referred with STDR had no record of attendance at the ophthalmology service two years after initial referral.16
The non-attendance rate for all patients in Ireland (at screening) is 18.5%, it increases to 33.9% in patients that have missed more than one appointment – this was identified as a significant risk factor in that analysis. In addition, risk of non-attendance increased by 24% for each decade and the patient is older or younger than 70 years old.5 Our study population had a higher proportion of rural patients and different age profiles, so some differences are expected. In the United States, Schoenfeld et al examined adherence rates to diabetic vision care guidelines and, similarly to the current study, found younger patients to be less adherent (51 compared to 56 years of age).17 Other studies found that non-attendance at DRS is more frequent among young adults aged 18–34.16,17 These studies were based in London, where the population is fluid. However, in Greenan’s DRT study, there was an almost twice as high a DNA rate recorded in the under-40 cohort compared to the over 40-year olds.14
We found that more males than females did not attend their appointments and this has been mirrored in DRS studies,16,17 as well as general diabetic clinic attendances,18,19 and referrals from DRS to DRT.14 Our findings contrast with RetinaScreen DRS, who also used OptoMize, reporting that being female was associated with an increased DNA rate (6%), and also being aged further away from 70 years was associated with higher DNA rates.5 Each decade change whether up or down from 70 years shifted the DNA rate up by 23%. Kelly’s study had a different geographic coverage, as well as including the rural catchment area of our cohort, it also captured patients from the capital city Dublin and its more populated environs.
Although there are disparities between non-attendance studies regarding both age and gender, a very consistent association has been noted between increased socioeconomic deprivation and reduced DRS attendance.16,20–23
Non-Attendance and Outcomes
Diabetic patients who default for hospital medical appointments have significantly more risk factors and complications than those who keep their appointments.18 Forster et al found that patients who had not attended DRS for 24 months, upon rescreening, had 10.84 times higher odds of referable diabetic retinopathy, compared to those who had attended annual examination.19 Our results were in keeping with these findings, and we showed a significant increase in ocular morbidity in non-attenders. A quarter (26%) of the patients showed a deterioration in their grade of retinopathy between initial referral and subsequent rescreen.
System-level reasons for DNAs need to be rectified, including updating and validating patients’ addresses and timely issue of appointments.20 Virtual HES had an equivalent non-attendance rate to our study; however, this may fall as patients become more familiar with and comfortable with this relatively new mode of consultation.
Non-attendance at hospital outpatient appointment is a challenge for healthcare systems. In 2016, the non-attendance rate for hospital appointments in Ireland was 15%, costing the Health Service Executive over 20 million Euros.21 Non-attendance has been calculated to cost the UK National Health Service £1 billion each year13 and the healthcare system in the US 150 billion dollars per annum.22 It is important that this challenge is recognised and addressed.
Interventions
A “reminder” is shown to be highly effective at increasing attendance rates at DRS.5 Multiple patient reminders are more effective than single reminders in improving DRS attendance rates; however, improvement appears only after the second reminder, with no significant improvement observed following additional reminders.23
Physician recommendation for regular DRS has been shown to improve patient attendance rates at DRS.24 Patient education around diabetes and eye disease has also been shown to increase compliance with attendance at DRS appointments.25 It is important that both nurses and physicians continue to educate their diabetic patients on the need for DRS and DRT and encourage them to attend their appointments.
Strengths and Limitations
One limitation of this study is the lack of biomarker data available for these patients, such as HbA1c. As poor glucose control is a major risk factor in worsening of DR, it would have been of interest to include this in the progression analysis. A major strength of the study is that both the population screening service (DRS) and the treatment centres (DRT) use the same electronic medical record software (Optomize). Because of this, we were able to follow patients from screening centres, to treatment and back again after discharge. The study population also comes from a large geographic region covering most of the country, giving a representative sample of both urban and rural populations.
Future Work
Our study has shown that there exists a subgroup of patients who are likely to be discharged from treatment centres for repeated non-attendance. As a result, they are at risk of missing out on sight-saving treatments. Future work on investigating the risk factors for non-attendance in treatment centres is a crucial first step in tackling this issue. Once this is accomplished, effective targeted interventions, such as those discussed above, could be implemented.
Conclusion
Patient non-attendance at DRT centres in Ireland is a significant challenge, with one in five patients defaulting. Increased patient engagement is important to mitigate patient visual loss and progression of ophthalmic pathology. An increased distance from treatment centre was shown to correlate with poor appointment compliance, and this is a factor to be considered when planning a diabetic screening and treatment programme. Further work needs to be done to better understand the reasons for non-attendance as well as factors that contribute to worsening eye status between discharge and rescreening.
Ethics Statement
This study meets the categorization of clinical audit as per the National Office of Clinical Audit (NOCA) GDPR Assessment table. Further ethics review was not required by the Reference Research Ethics Committee Midlands Area and Corporate (Regional Health Area B), in accordance with research regulations of Ireland.
Disclosure
J Harmon, R Acheson, S McMahon and L O′Toole are either employed by or have contractual agreements with NEC. L O′Toole also reports personal fees from Novartis and Bayer, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124–136. doi:10.1016/S0140-6736(09)62124-3
2. Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
3. Tracey M, Racine E, Riordan F, et al. Understanding the uptake of a national retinopathy screening programme: an audit of people with diabetes in two large primary care centres. HRB Open Res. 2019;2:17. doi:10.12688/hrbopenres.12926.3
4. Pandey R, Morgan MM, Murphy C, et al. Irish national diabetic RetinaScreen programme: report on five rounds of retinopathy screening and screen-positive referrals. (INDEAR study report no. 1). Br J Ophthalmol. 2022;106:409–414. doi:10.1136/bjophthalmol-2020-317508
5. Kelly SR, Loiselle AR, Pandey R, et al. Factors associated with non-attendance in the Irish national diabetic retinopathy screening programme (INDEAR study report no. 2). Acta Diabetol. 2021;58(5):643–650. doi:10.1007/s00592-021-01671-4
6. Zoega GM, Gunnarsdóttir P, Björnsdóttir S, et al. Screening compliance and visual outcome in diabetes. Acta Ophthalmol Scand. 2005;83(6):687–690. doi:10.1111/j.1600-0420.2005.00541.x
7. James M, Turner DA, Broadbent DM, et al. Cost effectiveness analysis of screening for sight threatening diabetic eye disease. Br Med J. 2000;320:1627–1631. doi:10.1136/bmj.320.7250.1627
8. Scanlon PH. The English national screening programme for diabetic retinopathy 2003–2016. Acta Diabetol. 2017;54(6):515–525. doi:10.1007/s00592-017-0974-1
9. Broadbent DM, Wang A, Cheyne CP, et al. Safety and cost-effectiveness of individualised screening for diabetic retinopathy: the ISDR open-label, equivalence RCT. Diabetologia. 2021;64(1):56–69. doi:10.1007/s00125-020-05313-2
10. Covid-19 HSE Clinical Guidance and Evidence. HSE interim clinical guidance on management of diabetes during the COVID-19 pandemic 118. HLI at Health Library Ireland @ HSE.
11. Brown MM, Brown GC, Sharma S, Shah G. Utility values and diabetic retinopathy. Am J Ophthalmol. 1999;128(3):324–330. doi:10.1016/s0002-9394(99)00146-4
12. Wolff DL, Waldorff FB, Von Plessen C, et al. Rate and predictors for non-attendance of patients undergoing hospital outpatient treatment for chronic diseases: a register-based cohort study. BMC Health Serv Res. 2019;19(1):1–11. doi:10.1186/s12913-019-4208-9
13. Philpott-Morgan S, Thakrar DB, Symons J, et al. Characterising the nationwide burden and predictors of unkept outpatient appointments in the national health service in England: a cohort study using a machine learning approach. PLOS Med. 2021;18(10):e1003783. doi:10.1371/journal.pmed.1003783
14. Greenan E, Salim M, Coakley DN, James M. The effect of geodemographic factors on the attendance rates at a regional diabetic retinopathy treatment centre. Ir J Med Sci. 2019;188(4):1207–1212. doi:10.1007/s11845-019-02009-4
15. Faes L, Fu DJ, Huemer J, et al. A virtual-clinic pathway for patients referred from a national diabetes eye screening programme reduces service demands whilst maintaining quality of care. Eye. 2021;35(8):2260–2269. doi:10.1038/s41433-020-01240-z
16. Keenum Z, McGwin G, Witherspoon CD, et al. Patients’ adherence to recommended follow-up eye care after diabetic retinopathy screening in a publicly funded county clinic and factors associated with follow-up eye care use. JAMA Ophthalmol. 2016;134(11):1221–1228. doi:10.1001/jamaophthalmol.2016.3081
17. Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines: baseline findings from the diabetic retinopathy awareness program. Ophthalmology. 2001;108(3):563–571. doi:10.1016/S0161-6420(00)00600-X
18. Griffin SJ. Lost to follow-up: the problem of defaulters from diabetes clinics. Diabet Med. 1998;15(Suppl 3):S14–24.
19. Forster AS, Forbes A, Dodhia H, et al. Non-attendance at diabetic eye screening and risk of sight-threatening diabetic retinopathy: a population-based cohort study. Diabetologia. 2013;56(10):2187–2193. doi:10.1007/s00125-013-2975-0
20. Strutton R, Du Chemin A, Stratton IM, Forster AS. System-level and patient-level explanations for non-attendance at diabetic retinopathy screening in Sutton and Merton (London, UK): a qualitative analysis of a service evaluation. BMJ Open. 2016;6:1–6. doi:10.1136/bmjopen-2015-010952
21. Murphy R, Taaffe C, Unit P, Division A. Patients’ reasons for non-attendance at outpatient appointments: a literature synthesis table of contents; 2019.
22. Carreras-García D, Delgado-Gómez D, Baca-García E, Artés-Rodriguez A. A probabilistic patient scheduling model with time variable slots. Comput Math Methods Med. 2020;2020:9727096. doi:10.1155/2020/9727096
23. Halbert RJ, Leung KM, Nichol JM, Legorreta AP. Effect of multiple patient reminders in improving diabetic retinopathy screening. A randomized trial. Diabetes Care. 1999;22:752–755. doi:10.2337/diacare.22.5.752
24. Dervan E, Lillis D, Flynn L, et al. Factors that influence the patient uptake of diabetic retinopathy screening. Ir J Med Sci. 2008;177(4):303–308. doi:10.1007/s11845-008-0192-5
25. Moinul P, Barbosa J, Qian J, et al. Does patient education improve compliance to routine diabetic retinopathy screening? J Telemed Telecare. 2020;26:161–173. doi:10.1177/1357633X18804749
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
