Back to Journals » Patient Preference and Adherence » Volume 16
The Effect of Self-Administration of Medication During Hospitalization on Patient’s Self-Efficacy and Medication Adherence After Discharge
Authors van Herpen-Meeuwissen LJ , van Onzenoort HA , van den Bemt PM , Maat B , van den Bemt BJ
Received 13 June 2022
Accepted for publication 19 August 2022
Published 28 September 2022 Volume 2022:16 Pages 2683—2693
DOI https://doi.org/10.2147/PPA.S375295
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Loes JM van Herpen-Meeuwissen,1,2 Hein AW van Onzenoort,1,3 Patricia MLA van den Bemt,4 Barbara Maat,2 Bart JF van den Bemt1,5
1Department of Pharmacy, Radboud University Medical Centre, Radboud Institute for Health Sciences, Nijmegen, the Netherlands; 2Department of Pharmacy, Elisabeth-TweeSteden Hospital, Tilburg, the Netherlands; 3Department of Clinical Pharmacy and Toxicology, Maastricht University Medical Center+, Maastricht, the Netherlands; 4Department of Clinical Pharmacy and Pharmacology, University Medical Center Groningen, University of Groningen, Groningen, the Netherlands; 5Department of Pharmacy, Sint Maartenskliniek, Nijmegen, the Netherlands
Correspondence: Loes JM van Herpen-Meeuwissen, Department of Pharmacy, Radboud University Medical Centre, PO Box 9101, Nijmegen, the Netherlands, Tel +31 624 3617744, Email [email protected]
Purpose: The effect of self-administration of medication (SAM), in which capable hospitalized patients administer medication themselves on medication self-efficacy is inconclusive. The aim of this study was to evaluate the effect of SAM on medication self-efficacy, adherence and patient satisfaction.
Patients and Methods: A prospective pre-post intervention study on the orthopedic ward of the Sint Maartenskliniek (Nijmegen) was conducted from January 2020 to July 2021. All adults admitted to this ward were eligible for participation. The primary outcome was the level of medication self-efficacy measured by the Self-Efficacy for Appropriate Medication Use Scale (SEAMS) one week after discharge. Secondary outcomes were SEAMS-score three months after hospitalization, medication adherence measured by the Medication Adherence Rating Scale (MARS) one week and three months after hospitalization and patient satisfaction expressed on a five-point Likert scale in patients who experienced SAM. The differences in median SEAMS-scores and non-adherence pre- versus post-implementation of SAM were statistically analyzed. Patients’ agreement regarding satisfaction with SAM was calculated as proportion per Likert scale answer.
Results: Of the 197 patients participating in the study, 96 were included pre- and 101 post-implementation of SAM. Median SEAMS-scores one week after discharge were 35 [IQR 31– 38] and 34 [IQR 30– 36] pre- and post-intervention respectively (p = 0.08). There was no difference in the proportion of non-adherent patients at one week and three months after discharge pre- and post-intervention, 52.4%, 53.2%, 57.9% and 64.4% respectively. Of the patients that experienced SAM 32% agreed and 49% strongly agreed that they would like to self-manage medication again during a future hospitalization.
Conclusion: In this orthopedic population with high medication self-efficacy scores at discharge, SAM did not affect patients’ medication self-efficacy nor medication adherence after hospitalization. Most patients preferred SAM. Additional studies should focus on the effect of SAM in other patient populations.
Keywords: self-administration of medication, medication self-efficacy, medication adherence, patient participation, patient satisfaction, hospitalization
Introduction
Multiple studies have demonstrated that medication adherence decreases after hospitalization.1–3 It can be hypothesized that this is due to shift in responsibilities in medication management from patients to healthcare professionals back to patients, before, during and after hospitalization respectively. This discontinuity of care is the result of the lack of involvement of patients in these transitions of care causing patients to lose control over their medication management.4–6
Although medication non-adherence has multiple causes,7 low self-efficacy is accepted as an important contributor to non-adherence.8–10 Self-efficacy refers to patients’ perceived capabilities for disease management and believed influence on their own healthcare outcomes.8,11,12 Furthermore, it is an operationalization of patient empowerment.8 Therefore, by empowering patients to participate in their medication management medication self-efficacy could be improved which in turn may enhance medication adherence.8,13
A strategy to empower patients during hospitalization is self-administration of medication (SAM). With SAM hospitalized patients have access to their own medication, which is self-administered under the condition that they are capable to do so.6,14 SAM is a multidimensional concept and has many potential benefits in terms of medication safety, patient participation and efficient use of healthcare resources, such as saving time of healthcare professionals.15–18 It may also improve medication self-efficacy. Only a few studies looked into the effect of SAM on medication self-efficacy, with conflicting results.19,20 Research showed that SAM could improve medication self-efficacy of cardiovascular disease patients.19 This effect was not seen in allogeneic hematopoietic stem cell transplantation patients.20 Moreover, these studies did not fully empower patients to be responsible for their inpatient medication management as, amongst others, patients only were allowed to administer medication in the presence of a nurse. Thus, evidence about the effect of SAM on patients’ medication self-efficacy when SAM is fully implemented is lacking. Therefore, the aim of this study was to evaluate the effect of SAM on medication self-efficacy, adherence and patient satisfaction after hospitalization in orthopedic patients.
Methods
Study Design and Setting
A prospective pre-post intervention study comparing SAM with nurse-led medication administration was conducted at the orthopedic ward of the Sint Maartenskliniek in Nijmegen. The Sint Maartenskliniek is a tertiary hospital specialized in orthopedics, rehabilitation and rheumatology. Data were collected pre-intervention from December 2019 to May 2020 and directly after implementation of SAM from March to July 2021 (post-intervention period).
Study Population
Adults admitted to the orthopedic ward were eligible for participation if they stayed for at least one night. Exclusion criteria were as follows: no informed consent, legally incompetent (eg, mentally retarded) and a life expectancy of less than three months. After the pre-intervention period, SAM was implemented as standard of care on the entire ward. Therefore, all eligible patients were included in the post-intervention study period (irrespective of whether the patient actually self-administrated medication).
Pre-Intervention Period
During the pre-intervention period SAM was not routinely offered to patients. Instead, nurses were responsible for medication administration. During hospitalization medication was supplied by the hospital pharmacy. Based on computerized medication orders by a physician, pharmacy technicians performed medication cart filling for the upcoming 24 hours. These carts were distributed to the ward where nurses administered the medication during the four medication rounds every day. Nurses were also responsible for documentation of this administration in the electronic Medication Administration Record (eMAR). During administration nurses checked the “five rights”, being the right patient, medication, dose, route and time; with the exception of nadroparin which was checked by scanning the bar code.
Implementation of SAM
SAM was implemented as standard clinical practice for capable patients starting from March 2021. It was based on the principle of using Patient’s Own Medication (POM): patients bring their own medication to use while in hospital.21 In case of an acute hospitalization, patients’ relatives were asked to bring patients’ medication within 24 hours. POM was checked by a nurse or pharmacy technician for completeness, identifiability (medication should be brought in the original primary package), quality (by observation; eg, expiration date), and quantity (supply sufficient for two weeks). This medication was stocked at patients’ bedside. Patients were provided with information about the medication and were given a medication intake schedule as guidance for medication administration. When medication was scheduled to be administered, patients took it from their own stock, administered the medication by themselves and recorded the administration on the intake schedule. During the medication round nurses asked patients if they had any questions related to the self-administration. Furthermore, they recorded the administrations on the eMAR based on information provided by the patient and the information on patients’ medication intake schedule. Newly started medication and medication changes, such as increased dosages, were discussed with and if necessary dispensed to the patient. Patients were provided with a new medication intake schedule and thereafter patients self-managed this medication as well.
Intravenous medication or medication that patients typically do not administer themselves in the outpatient setting were excluded from SAM and administered by nurses during the standard medication rounds. Each day, patients were assessed if they were capable for self-administration by a nurse based on the nurse’s experience and opinion. In case patients were not capable of performing SAM, nurses were responsible for patients’ medication administration.
Post-Intervention Period
During the post-intervention period SAM was considered fully implemented as standard of care.
Outcome Measures
The primary outcome was medication self-efficacy one week after hospitalization, measured with a Dutch version of the Self-Efficacy for Appropriate Medication Use Scale (SEAMS; see Appendix 1). The SEAMS was translated from English to Dutch according to Beaton’s guideline.22 The SEAMS is a reliable (Cronbach’s α = 0.89) and valid 13-item questionnaire with a minimum score of 13 and a maximum score of 39, a higher score indicating more medication self-efficacy.23 The items of the SEAMS assess patient’s confidence in correct medication use at a certain moment of time or situation.23 Answer options were as follows: unconfident, fairly confident, or extremely confident resulting in a one, two or three score respectively.23
To investigate if a potential change in SEAMS was sustained, the SEAMS-score at three months after discharge was a secondary outcome. Other secondary outcomes were the medication adherence at one week and three months after hospitalization, assessed using a Dutch version of the Medication Adherence Rating Scale (MARS; see Appendix 2). The MARS consists of five statements describing an attitude or behavior towards medication during the past week.24 Statements are rated with a 5-point Likert scale: always, often, sometimes, rarely, and never, which correspond to an ascending score from one to five resulting in a total score range of five (low adherence) to 25 (high adherence). Medication adherence was dichotomized into adherent (a MARS greater than or equal to 23) and non-adherent (a MARS smaller than 23)25 and is presented as the proportion of non-adherent patients.
These primary and secondary outcome measures were collected in both the pre- and the post-intervention period.
Finally, patient satisfaction with SAM was assessed in the post-intervention period. Patients experiencing SAM were asked about their agreement with the statement “I would like to self-manage my medication again during a future hospitalization”, using a 5-point Likert scale (strongly disagree, disagree, neither agree nor disagree, agree or strongly agree).
Data Collection
In both study periods patients were asked to fill out a paper questionnaire at the last day of hospitalization. This questionnaire consisted of general questions to collect patient characteristics, a SEAMS at discharge assessment and in the post-intervention period the patient satisfaction statement. The questionnaire was handed over to the patient and collected at the same day. One week and three months after hospitalization patients were invited by email to digitally fill out a questionnaire consisting of the SEAMS and MARS. In case the questionnaire was not returned, a reminder e-mail was sent four days (for the second questionnaire) and two weeks (for the third questionnaire) later. For practical reasons, patients were allowed to return the questionnaire within 7–14 days and 3–4 months respectively. In addition the following data were collected for all participants: year of birth, gender, medication use (name, dose, frequency) at hospital admission and discharge based on medication reconciliation, date of admission, date of discharge, number of newly started medications at discharge, body part of surgery, type of surgery (primary, follow-up as planned, follow-up unplanned), the American Society of Anesthesiologists physical status classification system (ASA) score,26 educational level, living situation, medication management at home (by themselves, with the help of a relative, with professional help) and how medication is stored at home (original packages, pill box or medication pre-packaged by an automated dispensing system). The first eleven items were collected from the hospital’s electronic patient record, the other items were asked in the paper questionnaire.
Sample Size
Based on a previous study, we hypothesized that SAM would lead to a relevant increase of medication self-efficacy with 3 points.27 Based on literature a baseline SEAMS-score of 32.9 was assumed.13,28–32 To reject the null hypothesis of no difference in medication self-efficacy one week after discharge between patients included pre- versus post-intervention period, with an alpha of 0.05 and a power of 0.9, a minimum of 42 patients were needed (21 per study period). To allow for 20% loss to follow up, we aimed to include at least 50 patients, but as SAM was implemented in routine practice all eligible patients were included.
Data Analysis
Descriptive data were presented in proportions for categorical data, means (standard deviation [SD]) for parametric continuous variables and median (interquartile ranges [IQR]) for non-parametric continuous data. In the primary analysis, an intention to treat analysis was performed to compare pre- and post-intervention SEAMS-scores after one week. This implicates that data of all patients (irrespective of whether they experienced SAM in the post-intervention period or not) were included for analysis. For this comparison a Mann–Whitney U-test was applied. In order to adjust for possible imbalance between the pre- and post-intervention group a multivariate linear regression analysis was performed with the SEAMS at one week as dependent variable and the intervention-group and potential confounders as independent variables. All covariates with a P-value <0.1 in the univariate analysis were entered into the multivariate analysis. As not all patients in the post-intervention group experienced SAM, a per-protocol analysis was performed. In this analysis, pre- and post-intervention SEAMS-scores after one week were compared, including for the post-intervention group only data of patients that actually experienced SAM. Differences in non-adherence between pre- and post-intervention one week and three months after patient’s discharge were determined using a Fisher’s Exact test. P-values of <0.05 were considered statistically significant. Regarding satisfaction with SAM, patient proportions were calculated per Likert scale answer. Data were analyzed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corp, Armonk, NY, USA).
Results
Of the 197 patients participating in the study, 96 were included in the pre-intervention period and 101 in the post-intervention period (Table 1). Patient characteristics differed between the study periods with respect to age (62.8 versus 57.0 years pre- and post-intervention respectively), SEAMS-score at discharge (37 versus 35), newly started medication at discharge (3 versus 4 medications) and living situation (more patients lived alone in the post-intervention group).
 |
Table 1 Study Population Demographics |
Main Outcome
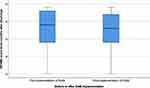
Median SEAMS-scores one week after discharge were 35 [IQR 31–38] and 34 [IQR 30–36] in the pre- and post-intervention period respectively (p = 0.08; Figure 1). Adjustment for SEAMS-score at discharge, (non-)adherence and living status in multivariate analysis did not change this result. Per-protocol analysis results were comparable: 35 [IQR 31–38] versus 34 [IQR 30–36] (p = 0.22; Figure 2).
Secondary Outcomes
Median SEAMS-scores at three months after discharge were 34 [IQR 29–38] and 33 [IQR 29–37] pre- and post-intervention respectively (p = 0.27; Figure 3).
The proportion of non-adherent patients at one week after discharge was 52.4% and 57.9% pre- and post-intervention, respectively (p = 0.54). At three months after discharge this was 53.2% and 64.4% pre- and post-intervention, respectively (p = 0.16).
Of the patients that experienced SAM 32.4% agreed and 49.3% strongly agreed that they would like to self-manage medication again during a future hospitalization (Figure 4).
 |
Figure 4 Pie chart that shows patient satisfaction (n = 71) with inpatient self-administration of medication (SAM). |
Discussion
This study showed that patient’s medication self-efficacy one week and three months after hospitalization did not differ between patients experiencing SAM compared to patients who had nurse-led medication administration. There was also no difference in self-reported medication adherence between the pre- and post-intervention study groups one week and three months after hospitalization. The majority of patients that experienced SAM preferred to self-manage their medication during hospitalization.
A lack of an effect on medication self-efficacy may be due to the characteristics of our study population. Compared to other studies, our population had a high level of medication self-efficacy at discharge, was relatively young and used less medication.13,19,27,29 Other studies report baseline medication self-efficacy levels of 22 to 32.19,29 Though in a different population than ours, Polito et al recently also showed that SAM did not increase self-efficacy.20 Participants in their study were also relatively young and had a high baseline SEAMS. These characteristics therefore might enhance patient’s capability to self-administer medication. Although not studied, we indeed experienced that the majority of our population was capable of performing SAM. On the other hand, Beigloo et al did establish a significant increase on patients’ medication self-efficacy due to SAM.19 In this study participants had a low mean SEAMS-score at admission leaving room for improvement and were younger compared to our population.19 So, given these specific circumstances future studies should focus on patient characteristics that hamper self-efficacy in relation to the potential added value of SAM.
Furthermore, non-adherence was high in our population. In other studies that investigated medication non-adherence, self-reported non-adherence was lower as rates ranged between 18% and 22%.33,34 The high non-adherence rate found in our study might be due to the methodological choice of using the MARS as outcome measure. Indeed, research using other outcomes did show an improvement of adherence due to SAM.15,17 The MARS is often used in patients with chronic medication use, but our study population used multiple post-surgery short-term and as-needed medications like analgesics and anti-emetics. Consequently, the MARS items may have been less suitable to assess adherence for this type of medication. This might have resulted in an overestimation of patient’s medication non-adherence. It might even be reasoned that not taking as-needed pain medication may indicate that patients have more knowledge on how and when to use this medication, potentially resulting in better pain control and shorter usage of pain medication decreasing the risk of addiction.35
Despite not finding an effect of SAM, the majority of patients that experienced SAM preferred to self-manage their medication during hospitalization. This preference of self-administration was also seen in previous research16,18,19 and may indicate that other aspects than self-efficacy (independence, respect of autonomy, feeling to be more in control, thought on medication safety) drive patient’s preference. Future studies should explore this in more detail, and such studies should also look into the effect of SAM in patients that prefer SAM compared to patients who do not.
The choice of the outcome measure self-efficacy may also be responsible for the lack of effect in our study. Studies with other outcome measures did show potential benefits of SAM. First, it might enhance medication safety during hospitalization as the number of medication errors decrease.15,16 Furthermore, SAM may lead to less medication safety problems beyond hospitalization as literature showed that there are less deviations in patients’ medication lists after hospitalization.15,16 Next to the possible effects on medication safety, SAM may result in an efficient use of healthcare assets, as it saves healthcare professionals’ time, reduces re-hospitalization rates and decreases the number of general practitioner consults after hospitalization.15,16,20,21,36 Therefore, we recommend to implement SAM in clinical practice, especially from a patient’s perspective, and collect further data to determine its value.
Some possible limitations of this study should be considered. First, the SEAMS-score at discharge was collected differently from the outcome SEAMS-scores at one week and three months after hospitalization, respectively by paper and digitally. This may have led to small variations in responses, but does not seem to outweigh the benefit of digital questionnaires.37,38 Second, post-intervention data were collected directly after implementing SAM. This may have resulted in a discrepancy in results as hospital’s staff was not habituated to the new work method yet. Therefore, for future research, we recommend a time series method to increase validity. Third, in general, the validity of patient reported outcome measures is suboptimal. Therefore, more reliable methods to determine medication adherence, such as dispensing records or actual pill counts, should be used in addition to patient reported outcomes. Nevertheless, these methods have generally acknowledged disadvantages too, because they are time consuming and less suitable for measurements during hospitalization. Moreover, the assumption is made that all dispensed medication is administered, which is not always the case.39 Fourth, in this study the patient characteristics differed between the pre- and post-intervention population. However, after adjustment for these potential confounders in a multivariate analysis, still no difference in SEAMS-scores could be demonstrated. The difference in characteristics might be time related as the pre-intervention period was before the COVID-19 pandemic and the post-intervention period was during the pandemic. During the pandemic different patients might be admitted due to shortages healthcare, eg, staffing, and patients may have avoided healthcare, eg, because of the fear of getting infected during hospitalization. Moreover, due to the specific patient characteristics of our study population, as mentioned before, the results might not be generalized to other patient populations. Therefore, we recommend to conduct future research in other study populations, such as patients with low SEAMS-scores at inclusion, admitted to other hospital wards, with longer hospital stay or who do not prefer SAM.
Conclusion
In conclusion, in this orthopedic population with high medication self-efficacy scores at discharge, SAM did not affect medication self-efficacy or medication adherence after hospitalization. Most patients prefer SAM. Additional studies should focus on the effect of SAM in other patient populations.
Abbreviations
SAM, self-administration of medication; eMAR, electronic Medication Administration Record; SEAMS, Self-Efficacy for Appropriate Medication Use Scale; MARS, Medication Adherence Rating Scale; ASA, American Society of Anesthesiologists physical status classification system.
Data Sharing Statement
Data will be available upon reasonable request.
Ethics Approval and Informed Consent
The regional medical ethics committee (METC Brabant) waived the requirement for ethical approval including informed consent (file: NW2019-50), as the Dutch Medical Research Involving Human Subjects Act (WMO) was not applicable for this study.
Consent for Publication
All authors have consented to publish.
Acknowledgments
The authors would like to thank the participants who took part in the study. Moreover, they would like to thank the healthcare professionals of the Sint Maartenskliniek, in special Eward Melis, for the successful implementation of self-administration of medication (SAM). Last, they would like to thank all research interns for their help (Anne Jansen, Annemieke Louters, Esmee Kanters and Seyma Taspinar).
Author Contributions
All authors contributed significantly to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
To conduct this research a grant from ZonMw (project number: 848022007) was received.
Disclosure
Dr Hein AW van Onzenoort reports grants from The Netherlands Organisation for Health Research and Development (ZonMw), during the conduct of the study. All authors declared to have no conflicts of interest in this work.
References
1. Fallis BA, Dhalla IA, Klemensberg J, Bell CM. Primary medication non-adherence after discharge from a general internal medicine service. PLoS One. 2013;8(5):e61735. doi:10.1371/journal.pone.0061735
2. Pasina L, Brucato AL, Falcone C, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31(4):283–289. doi:10.1007/s40266-014-0163-7
3. Mitchell B, Chong C, Lim WK. Medication adherence 1 month after hospital discharge in medical inpatients. Intern Med J. 2016;46(2):185–192. doi:10.1111/imj.12965
4. Billstein-Leber M, Carrillo COLJD, Cassano AT, Moline K, Robertson JJ; American Society of Health-System Pharmacists. ASHP guidelines on preventing medication errors in hospitals. Am J Health-Syst Pharm. 2018;75(19):1493–1517. doi:10.2146/ajhp170811
5. Vanwesemael T, Van Rompaey B, Petrovic M, Boussery K, Dilles T. SelfMED: self-administration of medication in hospital: a prevalence study in Flanders, Belgium. J Nurs Scholarsh. 2017;49(3):277–285. doi:10.1111/jnu.12290
6. Vanwesemael T, Boussery K, Dilles T. Self-administration of medication in hospital: a literature review. Nurs Sci Q. 2020;33(3):249–257. doi:10.1177/0894318420921155
7. The ABC Project team. Ascertaining Barriers for Compliance: policies for safe, effective and cost-effective use of medicines in Europe; 2012. Available from: http://abcproject.eu/img/ABC%20Final.pdf.
8. Nafradi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PLoS One. 2017;12(10):e0186458. doi:10.1371/journal.pone.0186458
9. Oshotse C, Zullig LL, Bosworth HB, Tu P, Lin C. Self-efficacy and adherence behaviors in rheumatoid arthritis patients. Prev Chronic Dis. 2018;15:E127–E127. doi:10.5888/pcd15.180218
10. Silva K, Miller VA. Does self-efficacy mediate the link between impulse control and diabetes adherence? J Pediatr Psychol. 2020;45(4):445–453. doi:10.1093/jpepsy/jsaa007
11. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi:10.1037/0033-295X.84.2.191
12. Bandura A. Self-efficacy and Health. In: Smelser NJ, Baltes PB, editors. International Encyclopedia of the Social & Behavioral Sciences. Pergamon; 2001:13815–13820.
13. Martin D, Kripalani S, Durapau VJ
14. Salmon K, Shaw T, Sanders K. Self administration of medicines and the re-use of patients’ own drugs. Foundation of Nursing Studies Dissemination Series; Vol.1, 2002.
15. Kaday R, Ratanajamit C. Inpatient self-administered medication under the supervision of a multidisciplinary team: a randomized, controlled, blinded parallel trial. Pharm Pract. 2020;18(2):1766. doi:10.18549/PharmPract.2020.2.1766
16. Sørensen CA, de Thurah A, Lisby M, Olesen C, Sørensen SB, Enemark U. Cost-consequence analysis of self-administration of medication during hospitalization: a pragmatic randomized controlled trial in a Danish hospital setting. Ther Adv Drug Saf. 2020;11:2042098620929921. doi:10.1177/2042098620929921
17. Hajialibeigloo R, Mazlum SR, Mohajer S, Morisky DE. Effect of self-administration of medication programme on cardiovascular inpatients’ medication adherence and nurses’ satisfaction: a randomized clinical trial. Nurs Open. 2021;8(4):1947–1957. doi:10.1002/nop2.870
18. Deeks PA, Byatt K. Are patients who self-administer their medicines in hospital more satisfied with their care? J Adv Nurs. 2000;31(2):395–400. doi:10.1046/j.1365-2648.2000.01286.x
19. Beigloo RHA, Mohajer S, Eshraghi A, Mazlom SR. Self-administered medications in cardiovascular ward: a study on patients’ self-efficacy, knowledge and satisfaction. Evid Based Care J. 2019;9(1):16–25. doi:10.22038/ebcj.2019.36298.1937
20. Polito S, Ho L, Pang I, Dara C, Viswabandya A. Evaluation of a patient self-medication program in allogeneic hematopoietic stem cell transplantation. J Oncol Pharm Pract. 2021;3:10781552211043525.
21. van Herpen-Meeuwissen LJM, van den Bemt BJF, Derijks HJ, et al. Economic impact of patient’s own medication use during hospitalisation: a multicentre pre-post implementation study. Int J Clin Pharm. 2019;41(6):1658–1665. doi:10.1007/s11096-019-00932-1
22. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25(24):3186–3191. doi:10.1097/00007632-200012150-00014
23. Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the Self-efficacy for Appropriate Medication Use Scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15(3):203–219. doi:10.1891/106137407783095757
24. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi:10.1016/S0920-9964(99)00130-9
25. Mårdby AC, Akerlind I, Jörgensen T. Beliefs about medicines and self-reported adherence among pharmacy clients. Patient Educ Couns. 2007;69(1–3):158–164. doi:10.1016/j.pec.2007.08.011
26. American Society of Anesthesiologists. ASA physical status classification system; 2022. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
27. Davis C, Jacobson TA, Vaccarino V, Kripalani S. Effect of a low-literacy intervention on self-efficacy and medication adherence; 2011.
28. Wu JR, Song EK, Moser DK. Type D personality, self-efficacy, and medication adherence in patients with heart failure-A mediation analysis. Heart Lung. 2015;44(4):276–281. doi:10.1016/j.hrtlng.2015.03.006
29. Kripalani S, Schmotzer B, Jacobson TA. Improving Medication Adherence through Graphically Enhanced Interventions in Coronary Heart Disease (IMAGE-CHD): a randomized controlled trial. J Gen Intern Med. 2012;27(12):1609–1617. doi:10.1007/s11606-012-2136-z
30. Pedrosa RB, Rodrigues RC. Adaptation and evaluation of the measurement properties of the Brazilian version of the self-efficacy for appropriate medication adherence scale. Rev Lat Am Enfermagem. 2016;24:e2692. doi:10.1590/1518-8345.0167.2692
31. Huang YM, Shiyanbola OO, Smith PD. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Prefer Adherence. 2018;12:793–802. doi:10.2147/ppa.S153312
32. Shiyanbola OO, Unni E, Huang YM, Lanier C. Using the extended self-regulatory model to characterise diabetes medication adherence: a cross-sectional study. BMJ Open. 2018;8(11):e022803. doi:10.1136/bmjopen-2018-022803
33. Huiskes VJB, van den Ende CHM, van Dijk L, Burger DM, van den Bemt BJF. Association between healthcare practitioners’ beliefs about statins and patients’ beliefs and adherence. Br J Clin Pharmacol. 2021;87(3):1082–1088. doi:10.1111/bcp.14467
34. van Heuckelum M, van den Ende CHM, van Dulmen S, van den Bemt BJF. Electronic monitoring feedback for improving medication adherence and clinical outcomes in early rheumatoid arthritis: a randomized clinical trial. Patient Prefer Adherence. 2021;15:1107–1119. doi:10.2147/ppa.S297170
35. Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med. 2015;162(4):276–286. doi:10.7326/m14-2559
36. Houlind MB, McNulty HBO, Treldal C, et al. One-stop dispensing: hospital costs and patient perspectives on self-management of medication. Pharmacy. 2018;6:2.
37. Bot AG, Menendez ME, Neuhaus V, Mudgal CS, Ring D. The comparison of paper- and web-based questionnaires in patients with hand and upper extremity illness. Hand. 2013;8(2):210–214. doi:10.1007/s11552-013-9511-z
38. Ebert JF, Huibers L, Christensen B, Christensen MB. Paper- or web-based questionnaire invitations as a method for data collection: cross-sectional comparative study of differences in response rate, completeness of data, and financial cost. J Med Internet Res. 2018;20(1):e24. doi:10.2196/jmir.8353
39. Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:217047. doi:10.1155/2015/217047
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.