Back to Journals » Clinical Optometry » Volume 14
The Effect of Home-Based Dichoptic Therapy on Young Adults with Non-Strabismic Anisometropic Amblyopia on Stereo Acuity
Authors Ojiabo SN , Munsamy AJ
Received 18 August 2022
Accepted for publication 18 October 2022
Published 28 November 2022 Volume 2022:14 Pages 237—247
DOI https://doi.org/10.2147/OPTO.S385845
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Sunday Nduka Ojiabo,1 Alvin J Munsamy2
1Department of Optometry, School of Health Science, University of KwaZulu-Natal, Westville Campus, Durban, South Africa; 2Discipline of Optometry, School of Health Science, University of KwaZulu-Natal, Westville Campus, Durban, South Africa
Correspondence: Sunday Nduka Ojiabo, Email [email protected]
Aim: To evaluate the effect of home-based dichoptic visual therapy using anaglyphic red-green filters on the stereo acuity in a sample of young adults with non-strabismic anisometropic amblyopia.
Methods: The study was observational and cross-sectional in design. Two groups (experimental vs control) were sourced using purposive sampling of young adults with non-strabismic amblyopia (experimental group) in comparison to an age-match control group without amblyopia. For the purpose of refractive adaptation, all participants in both groups were asked to wear their spectacle correction constantly for at least 16 weeks prior to exposure to home-based dichoptic therapy. Stereo acuity measurements using the Stereo Fly test were obtained before and after 40 hours exposure to home-based dichoptic therapy. The changes in stereo acuity post eight weeks (40 hours) training from baseline measurements was obtained. The difference in medians between the experimental and control groups using the Mann–Whitney U-test was measured with significance set at P value of < 0.05.
Results: A total of 38 young adults (19 males, 19 females) with a mean age of 24.05 ± 5.66 years were enrolled in this study. Nineteen anisometropic amblyopes comprised the experimental group, fifteen of which were classified as moderate amblyopia (6/12-6/36) and 19 non-amblyopes comprised the control group. Home-based dichoptic therapy used on the experimental group after 8 weeks showed a significant improvement in stereo-acuity with a mean improvement of 345.26 ± 184.85 sec arc− 1 [IQR:260;600; p< 0.001] when compared to the control group.
Conclusion: Home-based dichoptic therapy improved stereo-acuity in non-strabismic anisometropic amblyopes (moderate) in young adults. Thus suggesting that binocularity can improve in anisometropic adult amblyopes with a treatment modality that may be a convenient option better suit the demanding lifestyle of economically active adults who may not be able to comply with clinic-based therapy.
Keywords: adult amblyopia, stereo acuity, anisometropia, binocular vision, dichoptic therapy
A Letter to the Editor has been published for this article.
Introduction
Anisometropic amblyopia has the highest prevalence amongst all forms of amblyopia.1 The treatment of amblyopia including anisometropic amblyopia has been demanding for many eye care practitioners. Although the gold standard for treating amblyopia in children consists of optical correction followed by patching of the fellow eye, not everyone regains normal visual acuity following this therapy.1 Patching or occlusion therapy can be effective before the age of 13 years when the visual cortical development is still within the sensitive period.2 However, there is evidence of intact binocular mechanisms in the visual system of an adult amblyope which was rendered ineffective due to suppression under binocular viewing.3 In this study, our primary aim was to examine the effect of home-based dichoptic therapy on the stereo-acuity of adults who have passed the critical period of visual cortex development and to evaluate the potential usefulness of this type of therapy.
Achieving optimum outcomes with amblyopia treatment, where the visual functions of the amblyopic eye attain similarity with that of the good eye is always challenging in most patients and this is due to a lack of obvious structural causes that lead to this vision impairment.1
Dichoptic therapy was initially developed in the clinic using cumbersome psychophysical equipment. However, it has recently been translated to a more convenient hand-held device which can not only be used in the clinic but also at home.2 This has made it more convenient, especially for adults who have demanding schedules, in that they can now undergo the training in the convenience of their homes and this may improve compliance. A major consequence of amblyopia is the inability to fuse separate information seen by both eyes into one, causing impairment in depth perception or stereo-acuity. In the study, our primary outcome is the change in stereo-acuity. Stereo-acuity is a measure of the binocular visual functions which when improved in amblyopia results to an improvement in the quality of life.
Behavioral therapies have been shown to improve visual functions such as visual acuity, contrast sensitivity and stereo-acuity in adults with amblyopia who have passed the critical stage of visual cortex development.3–5 Recently, it has been shown that the cause of lack of binocular combination in amblyopia is due to suppression.6 Therefore, a reduction of suppression translates to an improvement in binocular vision. Dichoptic therapy is one of the forms of behavioral therapies that have been shown to reduce suppression in adults, thereby, improving stereo-acuity in other types of visual function. Long et al7 showed that clinic-based dichoptic therapy (Tetris game) using lenticular overlays improved stereo sensitivity by 0.0039 sec arc−1 in adults with anisometropic, strabismic and mixed amblyopia (combination of both). Similarly, Li et al3 showed that with the same parameters using head-mounted video games, improved stereo sensitivity by 0.0025 sec arc−1. In 2014, Hess et al4 showed that home-based dichoptic therapy (Tetris game) using both overlay and anaglyphic lens filters improved stereo sensitivity by 0.0077 sec arc−1 on anisometropic, strabismic and mixed amblyopic adults however he used six patients with anisometropic amblyopia and recommended study with a larger sample to confirm these findings.
Katsuki et al speculated that increasing contrast to the stimuli of the amblyopic eye might reinforce excitatory interactions through a reversed visual salience and attention process.8 This finding was recently supported by the result obtained in Chun et al's9 study where it was found that excitatory contribution to binocular interaction in the visual cortex is favourably reduced in amblyopia especially in strabismic amblyopia.
All these studies established that the use of dichoptic therapy both in a clinical and home setting can cause an improvement in stereo-acuity in adult amblyopes. However, the efficacy of dichoptic therapy using a red/green anaglyphic filter on an iPad Tetris game exclusively on anisometropic amblyopia has not been ascertained. This study attempts to determine the degree of change in stereo-acuity using only home-based dichoptic therapy on young adults with non-strabismic anisometropic amblyopia.
Materials and Methods
This prospective (observational, cross-sectional) study included 38 participants with an equal ratio of male to female in each group. Nineteen participants with anisometropic amblyopia (24.05 ± 5.74 years) were included in the amblyopic group and 19 without amblyopia in the control group (24.10 ± 5.70) were all recruited at the testing facility which is located in a private practice setting.
The sample size was calculated using sample size for an infinite population;
SS = {Z2P (1-P)}/C2
(SS = sample size,
Z; Z-value for confidence level of 95% = 1.96,
P; mean percentage of population in decimal = 0.01275,
C; confidence level in decimal = 0.05).
(From a previous study10 done on the prevalence of amblyopia in adults the percentage of population with amblyopia was found to be 2.5–2.6% and anisometropic amblyopia was estimated to be 50% of these values. Therefore, the mean percentage of population value for adults with amblyopia is estimated to be (2.5 + 2.6)/2 = 2.55%, and 50% of this gives 1.275%.)
SS = {1.962 x 0.01275 (1–0.01275)} / 0.052 = 19 per group
The study complied with the tenets of the Declaration of Helsinki, and was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal, Durban. Informed consents were obtained from all participants prior to commencement. The amblyopic participants were screened to meet the inclusion criteria with consideration to participants with at least a visual acuity of 0.2 Log MAR or worse on the amblyopic eye and two lines difference in Log MAR between the two eyes on the Log MAR visual chart with a stereo-acuity poorer than 40 sec of arc obtained using the Stereo Fly test. Nineteen randomly selected non-amblyopes who had best corrected visual acuity of 0.00 Log MAR and a stereo-acuity of less than 40 sec of arc formed the control group. The control group was made up of volunteers who were interested in participating in the study. Participants in both groups were each recruited upon meeting the inclusion criteria as demonstrated in Table 1. Some of these participants, especially in the control group, were given refreshment as incentives at the testing facility and transportation to and from the testing facility. The control group was included in this study to ascertain if the effect of dichoptic therapy noticed in the amblyopic group can be seen in the control group, which is a test of the validity of dichoptic therapy. All participants (control and amblyopic) were between the ages of 18 to 35 years (24.05 ± 5.66 years) with no history of vision therapy, surgery or previous amblyopic therapy. All participants spent their first 1 hour with the clinician learning how to play the game and were asked to continue at home to the satisfaction of the clinician that participants were knowledgeable on how to play the game. Visual examination such as visual acuity test, refraction, keratometry, slit lamp biomicroscopy, Worth Four dot test, color vision assessment, contrast sensitivity test, cover and uncover test, stereo acuity test and ocular motility test were done by a proficient optometrist on all participants prior to enrollment. Participants with stimulus deprivation amblyopia or any ocular comorbidity or neuronal defects were excluded.
 |
Table 1 Selection Criteria for Study Participants for the Amblyopic and Control Groups |
A case history was completed on all participants to ensure they were not undergoing any form of visual therapy, any ocular surgery and to rule out any pre-existing ocular or systemic conditions that may influence the outcome of dichoptic therapy. Thereafter, participants underwent a routine visual examination consisting of distance (6 m) and near (40 cm) visual acuity using Bailey-Lovie Log MAR charts and a cover and uncover test to rule out any form of strabismus. All participants in the amblyopic group with difference in best-corrected distance visual acuity of two or more lines between both eye on the Log MAR distance visual acuity chart, best-corrected visual acuity of 0.2 Log MAR or worse on the amblyopic eye and near visual acuity of less than N6 were included in the study.
Suppression testing was done using the Worth Four dot test at both 6 m and 33 cm on all participants without their habitual refractive correction to ascertain the presence of suppression as well as the suppressed eye. Color vision assessment was done monocularly using the Ishihara color test plates to screen for defects in the visual pathway followed by slit lamp biomicroscopy to screen for any anterior segment related pathology. Finally, the posterior segments were then thoroughly examined using an ophthalmoscope for intraocular pathologies to confirm the reduced acuity was from the amblyogenic factor of anisometropia.
A cycloplegic refraction was carried out on both eyes using 0.5% tropicamide eye drops with a table-mounted, made in Japan, Nidek ARK-1-510A auto-refractometer. Patients with a difference in astigmatism greater than 1.00 DC, hyperopia greater than 1.00 DS, and myopia greater than 1.50 DC were considered as anisometropic patients. For the purpose of refractive adaptation, all participants in both groups had worn appropriate spectacle correction constantly for at least 16 weeks prior to exposure to dichoptic therapy.
Data Collection
The participants were assigned to a home-based therapy regimen for 1 hour daily at 15 minute intervals for eight weeks duration to complete a total duration of 40 hours after the clinician had trained each participant on the dichoptic therapy using a Tetris game on an Apple IPad, 9.7 inches.4,5,12,13
Study Process
Stereo-acuity was measured using the Stereo Fly test. Pre-therapy stereo acuity was recorded at week zero before the commencement of dichoptic therapy. Participants were then asked to continue the therapy weekly at home for a total of 5 hours per week at an interval of 15 minutes four times a day to equate to an hourly training daily regimen after a one-hour training session in the clinic with the clinician.4,5,14 At the end of each week, their stereo-acuity measurements were repeated in the clinic and recorded as post-therapy stereo-acuity measurements for each week, making a total of 8 post stereo-acuity measurements. This process lasted for 8 weeks until each participant had completed their 40 hours of therapy. This marked the final post-stereo-acuity measurement. Each participant was constantly monitored from their game APP log history every week when they returned to the clinic. The APP has a time-recorder in the app which shows how long the game was played per day. The mean cumulative time recorded in the APP log history was used to measure the compliance rate in percentage and compliance was calculated based on the intended treatment of 5 days per week for 8 weeks. Two participants were found to exceed the game play time in the first week and were informed about the effect. The excess play-time for these participants was subtracted from the subsequent week. Seventy five percent (75%) and above play-time was regarded as a good compliance.
Dichoptic Therapy
A hand-held nine-inch Apple IPad device was used to display the Tetris game at a standard room illumination (150–500 lux), with a red green anaglyph lens filter worn with the red lens on the right eye and the green lens on the left eye regardless of the amblyopic eye. The Tetris game is made of red and green blocks. The red blocks which fall from the top of the screen were constantly alternated to form a scintillating block at the bottom of the screen and on reaching the bottom, they turned green. With the anaglyph lens filters, the images are dissociated and the participants see the red blocks with the eye behind the red filter and the green blocks with the eye behind the green filter.
Participants, in both groups were asked to wear their most recent spectacle correction for at least sixteen weeks prior to exposure to the therapy. A red-green anaglyph clip-on lens was placed over each eye, and the participants were expected to wear their spectacle correction constantly during the training period. The contrast on the good eye was reduced until the participant reports equality in contrast on both eyes. The percentage difference in contrast attained after contrast re-balancing was used as a measure of suppression at all stages of contrast re-balancing during the therapy process. The treatment is based on the fact that if contrast sensitivity is reduced on the good eye, there will be a value for fusion which will cause an improvement in contrast sensitivity of the amblyopic eye depending on the severity of the suppression.12,15 Over time, as the participant visited the clinic for a follow-up, this reduced contrast on the good eye was gradually increased by the examiner while fusion was maintained.
Stereo-Acuity
Stereo-acuity measurements were obtained at 40 cm using the Stereo Fly test which measures stereopsis from 3500 to 40 seconds of arc. The Stereo Fly test involves polarized vectographic plates which are made up of nine sets of four circles arranged in a diamond fashion with one circle per set distinguished from others (measures stereo-acuity from 800 to 40 sec of arc), three rows of five animals with one per row distinctive from others (measures stereo-acuity between 400 and 100 sec of arc) and a housefly (measures stereo-acuity from 3500 to 40 sec of arc).
Each participant was asked to wear polarized lenses over their best corrected habitual spectacle lenses and a housefly was presented under standard room illumination (500 lux). The participant was asked to pinch the wings of the housefly between the thumb and forefinger, successfully doing that above the plate shows that there was stereopsis present. They were then asked to view the group of four patterns and were expected to identify the circle in each group which is seen to “float” in front of others. The last group that was accurately identified was recorded as the stereo-acuity of the patient and regarded as the highest form of binocular coordination.
Statistical Analysis
All data were tested for normality using one sample Kolmogorov–Smirnov test. For the participants in the amblyopic group (D (19) = 0.632, p <0.05) it was found that they were not normally distributed, therefore, the Wilcoxon sign ranked test (one sample test) was used to test if the intervention caused changes on each individual by comparing the post therapy after eight weeks with the baseline measurement. The Wilcoxon sign ranked test was used to assess the changes in stereo-acuity in both the amblyopic and control group, the Kruskal–Wallis H-test was also done to ascertain if there are statistically significant differences between the groups before and after exposure to dichoptic therapy. t-test was performed to ascertain the mean difference in stereoacuity before and after 8 weeks of exposure to dichoptic therapy. The Mann–Whitney U-test (two sample test) was then used to test for the difference in medians between the amblyopic and control groups. Finally, a linear mixed model regression analysis was done to ascertain the influence of age and depth of amblyopia, and the severity of anisometropia and type of refractive error on changes in stereo-acuity. All this was done using STATA version 15.0, at a statistical significance set at a P-value of less than 0.05.
Results
Table 2 summarizes the baseline characteristics of the sample for the control and experimental (amblyopic) groups. For the amblyopic group, four (4) of the 19 participants were classified as having severe amblyopia (V/A worse than 0.80 Log MAR) prior to the therapy and 15 of the 19 were classified as having moderate amblyopia (V/A between 0.30 to 0.80 Log MAR).14 For the same group, five participants were classified as having moderate anisometropia (spherical difference between both eyes of ≥1.00 DS to <2.00 DS) and 14 of the 19 had severe anisometropia (spherical difference between both eyes of >3.00 DS).16 The type of refractive error was also considered, three participants had myopic astigmatism and 16 participants had hyperopic astigmatism.
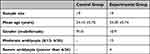 |
Table 2 Baseline Characteristics of the Control and Amblyopic Groups |
Stereo-Acuity and Home-Based Dichoptic Therapy
Table 3 shows that there was a statistically significant change in stereo-acuity for the amblyopic group only from week zero to week eight, and a significant difference was found in stereo-acuity after eight weeks of home-based dichoptic therapy between the changes in amblyopic and control groups. A linear mixed effect model showed that age did not influence the rate of change of stereo-acuity during the eight weeks of home-based dichoptic therapy (P = 0.544).
 |
Table 3 Change in Stereo-Acuity After Eight Weeks of Home-Based Dichoptic Therapy for the Control and Experimental (Amblyopic) Groups |
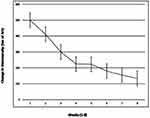
The study shows that all the participants gained improvement in stereo-acuity after eight weeks of home-based dichoptic therapy for the amblyopic group of anisometropic amblyopes with a mean improvement of 345.26 ± 184.85 seconds of arc. Figure 1 goes on to show the improvement started from week 2 with the largest changes occurring in week 3, which continued for weeks until week eight but at a reduced rate. From the linear mixed effect model, it showed that the severity of amblyopia does not have any significant effect on the rate of improvement in stereo-acuity (β = −40.42; 95% Cl: 96.10–15.26; P = 0.153). A mixed linear regression was performed to ascertain if there was a significant effect of age on the change in stereo-acuity using home-based dichoptic therapy (β = −0.89; 95% Cl: −4.95–3.17; p = 0.665).
The influence of the severity of anisometropia on change in stereo-acuity as seen in Figure 2 was analyzed using a multiple linear regression model, and it was shown that participants with moderate anisometropia (β = −158.39 (95% CI: −293.50, −23.29) P = 0.024) were significantly associated with a lower change in stereo-acuity as compared to participants with severe anisometropia. Furthermore, a linear regression showed the type of refractive error did not have an effect on the change in stereo-acuity using home-based dichoptic therapy (β = 126.13 (95% Cl: −52.56, 305.11), P = 0.155).
 |
Figure 2 The influence of the severity of anisometropia on change in stereoacuity. Stereoacuity improved more in participants with severe amblyopia compared to participants with moderate amblyopia. |
Although the mean change in distance and near visual acuity was not our primary outcome, however, they were noted. For the distance visual acuity, there was a significant change from the baseline (0.52±0.06 Log MAR) to post therapy (0.31±0.03 Log MAR) of 0.21±0.015 Log MAR (z = −3.823; p = 0.00014). Therefore, the magnitude of improvement in distance visual acuity in this study was 2.1 lines on the Log MAR chart. For near visual acuity, there was also a significant improvement from baseline (0.54±0.084 Log MAR) to post therapy (0.50±0.0068 Log MAR) of 0.044±0.025 Log MAR (z =−2.641, p = 0.0083).
Discussion
Historically, amblyopia is a common reason for outpatient therapy in children.16 Therefore, early detection and treatment of the causes of amblyopia in childhood is crucial to avoid adult amblyopia.17 Our study found that utilizing a “Tetris” game on a hand-held iPad as a form of home-based dichoptic therapy design can lead to an improvement in stereo-acuity in young adults beyond the childhood years with non-strabismic anisometropic amblyopia. This was achieved by rebalancing input from the amblyopic and fellow eye to induce fusion. This therefore, supports psychophysical studies which reduce suppression of the amblyopic eye by improving binocular functions as in this case's stereo-acuity.
Our study has presented confirmatory and novel findings in agreement with previous work on amblyopia in adults.3,4,17 Studies have shown that in adult amblyopia, monocular functions can improve using clinic-based monocular and binocular therapies.17,18 Consistent with previous studies by Hess et al19 reduced suppression resulted in improvement in stereo-acuity of anisometropic, strabismic and mixed amblyopia, where six out of 10 participants gained improvement in stereo-acuity similar to what was shown in our study. This gain in stereo-acuity is achieved by a constant reduction of the contrast sensitivity of the good eye as participants played the Tetris game and gradually led to a reduction in the suppression of the amblyopic eye by the good eye. The gain in stereo-acuity in this study is comparable to that in previous studies where the Randot test was used on participants aged 6 to 65 years.4,20 It was found that participants in these studies gained improvement in stereo-acuity (200 to 129.90 sec of arc) as compared to our study with stereo-acuity change of 213.42 sec of arc. However, similar findings were not found in other studies that also utilized the Randot test on adult amblyopia (17–69 years),3,5,7,21 where the improvement in stereo-acuity was found to be between 256 and 1000 sec of arc.
The participant profile of our study was restricted to non-strabismic anisometropic amblyopia whilst Hess et al22 included anisometropic, strabismic and mixed amblyopia and noticed a 60% improvement. Our study comprised of only anisometropic amblyopes which may explain the hundred percent (100%) improvement in all adults in the amblyopic group with both severe (0.80 Log MAR or worse) and moderate (0.30 to 0.80 Log MAR) anisometropic amblyopia. In contrast to strabismic and mixed amblyopes, many anisometropic amblyopes retain some stereopsis. Hess et al found that more than 50% of anisometropic amblyopes passed the Randot circles test compared with only 10% of strabismic amblyopes, accounting for the fewer number of participants who gained improvement when compared to our study.19 Weakley showed poorer stereo-acuity was associated with severe anisometropia, this was in contradistinction to our findings that showed more improvement in participants with severe anisometropia.23 However, the smaller representation of this group within the sample may require further studies to confirm this finding.
Similar findings were obtained in a recent study of adults with anisometropic amblyopia and it was discovered that dichoptic-based active vision therapy using “VisuoPrime” software proved effective as a primary modality in adults with anisometropic amblyopia.24
We discovered that just within a short period of three weeks (15 hours) of home-based dichoptic therapy in young adults resulted in a significant improvement in stereo-acuity. This is similar to the study by Hess et al25 where the degree of suppression reduced after two weeks by engaging in one to three hours of game-play per day. These results may indirectly indicate that the adult visual cortex has sufficient plasticity to recover visual function and also provides evidence that the adult amblyopic brain can learn.17,22,26 The findings in this study showed that all 19 participants with anisometropic amblyopia gained improvement to a certain degree and, with this gain in stereo-acuity, implying that binocularity is improving to a certain extent. Thus, showing comparable results for home-based therapy with the clinic-based offering, an option of home-based treatment without clinic-based intervention may be a more convenient treatment option for patients with demanding lives when they may be non-compliant with clinic-based therapy. We quantified compliance as the mean cumulative time spent playing the Tetris game throughout the 8 weeks and 75% and above was regarded as a good compliance. An analysis of the iPad log files allowed for the treatment compliance to be assessed. It was shown that there was an excellent compliance by both groups, this may be due to the fact that all participants reported that the Tetris game was engaging. We expected a higher compliance rate with the amblyopic group compared to the control group due to the anticipated outcome by participants in the amblyopic group. However, both groups had equal compliance rate.
The fundamental basis of dichoptic therapy to explain the observed changes is based on psychophysical studies that information perceived by the amblyopic eye is subject to an inhibitory drive from the fellow eye prior to binocular fusion.26 Dichoptic therapy treatment for amblyopia is designed to reduce suppression of the amblyopic eye by the fellow eye and therefore enhance binocular functions like stereo-acuity.
Significant improvement in stereo-acuity achieved by the amblyopic group in this study further supports the argument that dichoptic therapy is an effective therapy for improving stereo-acuity in young adults with anisometropic amblyopia independent of age and the severity of amblyopia. This improvement in stereo-acuity will translate to a positive impact on activities of daily living and help improve better career options for these adults. The lack of significant changes in visual parameters of the control group further indicates that dichoptic therapy (home-based) is valid for improving stereo-acuity in amblyopic treatment. The degree of stereo-acuity improvement in this study first observed after three weeks of exposure to dichoptic therapy is consistent with previous studies which used the same therapy both at home and in clinic on adults with amblyopia.26,27 Also, the premise from previous studies, demonstrated that greater improvement with perceptual training is achieved in the first eight sessions of treatment.25,27 Nevertheless, eight (8 weeks) after the end of therapy, participants in the amblyopic group were asked to return to the clinic for stereo-acuity testing to note any reversal or further gain in stereo-acuity. It was found that there was no reversal nor further improvement in stereo-acuity. Further to this, the inter-ocular contrast setting used in this therapy was calibrated at the start of each session which may have contributed in optimizing the treatment effect and degree of improvement in stereo-acuity.
The linear regression analysis showed that dichoptic therapy has an equal effect on all degrees of anisometropic amblyopia, which implies that the severity of amblyopia in the amblyopic group did not have an effect on the change in stereo-acuity. Likewise, this analysis demonstrated that age does not influence the level of improvement of stereo-acuity of adults with non-strabismic anisometropic amblyopia.
No adverse effect was reported from the use of home-based dichoptic therapy in this study. However, adaptation difficulty was reported by one participant during the initial phase of optical adaptation.
Limitations
The limitations of this study include some participant’s failure to report to the clinic for follow-up visits at the required time due to work commitments which helps make a case for the study objective of a home-based care for dichoptic therapy. Some participants played the game more than the required 15 minutes per session which affected the ability to keep records of the scores after each session of gameplay, although this did not have an affect on the weekly changes and cumulative time of play at the end of eight weeks which equated to 40 hours. Although participants reported they played the game alone, there was no measure put in place to ascertain the possibility of the game being played by another person as the APP was not password-protected, limiting widespread generalization. However, the use of a home-based approach as examined in this study is an important step forward as it can be monitored through the game “APP”'s daily history and therefore can grant the clinician ease of ability to evaluate the progress of the therapy process. Although the Stereo Fly acuity test gained merit in clinical studies, however, there is a disadvantage of monocular depth cue and the threshold of 40 seconds of arc at 40 cm was a limitation especially for the control group having that the normal human stereo threshold is between 2–10 seconds of arc.28
Recommendations
Home-based dichoptic therapy shows promising results and could be used on a larger scale randomized control trial for the purpose of validating this type of treatment model in adults with anisometropic amblyopia. These results were obtained over eight weeks, but this may occur over a shorter time frame being that the largest improvement occurred after three weeks. Especially if patients choose to do it at home, during lunch at work or even while travelling to work. This encourages convenience and compliance to the therapy. The visual acuity measurements should be done using the visual evoked potential (VEP) as it may provide a more accurate visual acuity representation in comparison to optotypes acuity in amblyopic patients. The VEP reveals the visual acuity in amblyopia irrespective of the error in the amblyopic eye.29
Conclusion
A noteworthy finding of this study was that home-based dichoptic therapy improved stereo-acuity in anisometropic amblyopic adults without strabismus. Home-based dichoptic iPad therapy may represent a feasible treatment option for anisometropic amblyopia in adults. This may better suit the lifestyle of economically active adults who may not be able to comply with clinic-based therapy. It also further promises improvement, considering all participants showed some level of improvement in stereo-acuity. Further clinical trials are needed to confirm these findings to recommend widespread use.
Ethics and Consent
Biomedical Research Ethics Committee (BREC) BREC Ref No: BE704/18.
Affiliation: University of KwaZulu-Natal (UKZN).
A written consent to participate was obtained from all participants of the study.
Acknowledgments
University of KwaZulu-Natal (UKZN), Developing Research Innovation, Localization and Leadership in South Africa (DRILL) fellow. DRILL, is a NIH D43 grant (D43TW010131) awarded to UKZN in 2015 to support a research training and induction programme for early career academics. The content is solely the responsibility of the authors and does not necessarily represent the official views of DRILL and the National Institutes of Health.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
1. Maconachie GDE, Gottlob I. The challenges of amblyopia treatment. Biomed J. 2015;38(6):510–516. doi:10.1016/j.bj.2015.06.001
2. Black JM, Thompson B, Maehara G, Hess RF. A compact clinical instrument for quantifying suppression. Optom Vis Sci. 2011;88(2):334–343. doi:10.1097/OPX.0b013e318205a162
3. Li J, Thompson B, Deng D, Chan LYL, Yu M, Hess RF. Dichoptic training enables the adult amblyopic brain to learn. Curr Biol. 2013;23(8):308–309. doi:10.1016/j.cub.2013.01.059
4. Hess RF, Black J, Thompson B, et al. The iPod binocular home-based treatment for amblyopia in adults: efficacy and compliance. Clin Exp Optom. 2014;97(5):389–398. doi:10.1111/cxo.12192
5. Vedamurthy I, Nahum M, Huang SJ, et al. A dichoptic custom-made action video game as a treatment for adult amblyopia. Vision Res. 2015;114:173–187. doi:10.1016/j.visres.2015.04.008
6. Mansouri B, Thompson B, Hess RF. Measurement of suprathreshold binocular interactions in amblyopia. Vision Res. 2008;48(28):2775–2784. doi:10.1016/j.visres.2008.09.002
7. To L, Thompson B, Blum JR, Maehara G, Hess RF, Cooperstock JR. A game platform for treatment of amblyopia. IEEE Trans Neural Syst Rehabil Eng. 2011;19(3):280–289. doi:10.1109/TNSRE.2011.2115255
8. Katsuki F, Constantinidis C. Bottom-up and top-down attention: different processes and overlapping neural systems. Neuroscientist. 2014;20(5):509–521. doi:10.1177/1073858413514136
9. Hou C, Nicholas SC. Perceptual learning with dichoptic attention tasks improves attentional modulation in V1 and IPS and reduces interocular suppression in human amblyopia. Sci Rep. 2022;12(1):9660. doi:10.1038/s41598-022-13747-4
10. Attebo K, Mitchell P, Cumming R, Smith W, Jolly N, Sparkes R. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105(1):154–159. doi:10.1016/S0161-6420(98
11. Levi DM, Mckee SP, Movshon JA. Visual deficits in anisometropia. Vision Res. 2012;51(1):48–57. doi:10.1016/j.visres.2010.09.029.Visual
12. Hess RF, Thompson B. Amblyopia and the binocular approach to its therapy. Vision Res. 2015;114:4–16. doi:10.1016/j.visres.2015.02.009
13. Jeon ST, Maurer D, Lewis TL. The effect of video game training on the vision of adults with bilateral deprivation amblyopia. Seeing Perceiving. 2012;25(5):493–520. doi:10.1163/18784763-00002391
14. Williams C. Amblyopia. BMJ Clin Evid. 2011;30:709.
15. Hess RF, Thompson B, Black JM, et al. An iPod treatment of amblyopia: an updated binocular approach. Optometry. 2012;83(2):87–94. doi:10.1016/j.optm.2011.08.013
16. Duman R, Atilla H, Çatak E. Characteristics of Anisometropic Patients with and without Strabismus. Turk Oftalmol Derg. 2018;(48):23–26. doi:10.4274/tjo.44342
17. Polat U, Ma-Naim T, Belkin M, Sagi D. Improving vision in adult amblyopia by perceptual learning. Proc Natl Acad Sci. 2004;101(17):6692–6697. doi:10.1073/pnas.0401200101
18. Cleary M, Moody AD, Buchanan A, Stewart H, Dutton GN. Assessment of a computer-based treatment for older amblyopes: the Glasgow pilot study. Eye. 2009;23(1):124–131. doi:10.1038/sj.eye.6702977
19. McKee SP, Levi DM, Movshon JA. The pattern of visual deficits in amblyopia. J Vis. 2003;3(5):380–405. doi:10.1167/3.5.5
20. Travi G, Dehnadi S, Mansouri B. NANOS Amblyopia poster 2018-41x41. In:. 2018. doi:10.13140/RG.2.2.10971.05922
21. Li J, Spiegel DP, Hess RF, et al. Dichoptic training improves contrast sensitivity in adults with amblyopia. Vision Res. 2015;114:161–172. doi:10.1016/j.visres.2015.01.017
22. Li RW, Klein SA, Levi DM. Prolonged perceptual learning of positional acuity in adult amblyopia: perceptual template retuning dynamics. J Neurosci. 2008;28(52):14223–14229. doi:10.1523/JNEUROSCI.4271-08.2008
23. Weakley DR. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108(1):163–171. doi:10.1016/S0161-6420(00)00425-5
24. Murali K, Ramesh A, Murthy S, Goyal A. Binocular therapy as primary intervention in adults with anisometropic amblyopia. Taiwan J Ophthalmol. 2021;12:317. doi:10.4103/tjo.tjo_37_21
25. Li RW, Provost A, Levi DM. Extended perceptual learning results in substantial recovery of positional acuity and visual acuity in juvenile amblyopia. Invest Ophthalmol Vis Sci. 2007;48(11):5046–5051. doi:10.1167/iovs.07-0324
26. Black JM, Hess RF, Cooperstock JR, To L, Thompson B. The measurement and treatment of suppression in amblyopia. J Vis Exp. 2012;14(70):3927. doi:10.3791/3927
27. Levi DM, Li RW. Improving the performance of the amblyopic visual system. Philos Trans R Soc B. 2009;364(1515):399–407. doi:10.1098/rstb.2008.0203
28. Romano PE, Romano JA, Puklin JE. Stereoacuity development in children with normal binocular single vision. Am J Ophthalmol. 1975;79(6):966–971. doi:10.1016/0002-9394(75)90679-0
29. Griffin JR, Grisham JD. Binocular anomalies: diagnosis and vision therapy. Optom Vis Sci. 2005;82(3):135–187.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.