Back to Journals » Therapeutics and Clinical Risk Management » Volume 14
The effect of diabetes on perioperative complications following spinal surgery: a meta-analysis
Authors Luo W, Sun R, Jiang H, Ma X
Received 24 August 2018
Accepted for publication 13 November 2018
Published 12 December 2018 Volume 2018:14 Pages 2415—2423
DOI https://doi.org/10.2147/TCRM.S185221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Wei Luo,1 Ru-xin Sun,2 Han Jiang,3 Xin-long Ma1
1Department of Orthopedics, Tianjin Hospital, Tianjin 300211, People’s Republic of China; 2Department of Gynaecology and Obstetrics, Tianjin Hongqiao Hospital, Tianjin 300131, People’s Republic of China; 3Department of Orthopedics, Tianjin Third Central Hospital, Tianjin 300170, People’s Republic of China
Background: Degenerative spinal diseases and diabetes mellitus (DM) have increasingly become a social and economic burden. The effect of DM on spinal surgery complications reported by previous studies remains controversial.
Methods: We searched MEDLINE, Cochrane CENTRAL, ScienceDirect, EMBASE, and Google Scholar to identify studies reporting the relationship between DM and spinal surgery complications. Two independent reviewers performed independent data abstraction. The I2 statistic was used to assess heterogeneity. A fixed-effects or random-effects model was used for the meta-analysis.
Results: Twenty-four studies met the inclusion criteria. Surgical site infection and the incidence of deep venous thrombosis after spinal surgery were significantly higher in patients with than in patients without diabetes, and the length of hospital stay was significantly longer in patients with diabetes (P<0.05). No significant differences were observed in the risk of reoperation, blood loss, and operation time between patients with and those without diabetes (P>0.05).
Conclusion: Patients with diabetes have a higher risk when undergoing spinal surgery than patients without diabetes. Diabetes increases the risks of postoperative mortality, surgical site infection, deep venous thrombosis, and a prolonged hospitalization time after spinal surgery.
Keywords: diabetes mellitus, spine, surgery, complication
Introduction
Diabetes mellitus (DM) is a group of metabolic diseases of blood glucose dysregulation that can cause complications and lead to target organ, peripheral vascular, and nerve dysfunction.1 Previous studies showed that DM may affect the typical signs and symptoms of cervical spondylotic myelopathy2 and could be a predisposing factor for the development of lumbar spinal stenosis.3 Several studies have focused on the correlation between diabetes and complications of spinal surgery.4,5 Previous studies have shown that glycemic control could reduce the risk of postoperative mortality, surgical site infection, venous thrombosis, and a prolonged length of hospital stay after spinal surgery in patients with diabetes.6–9 Appaduray and Lo10 demonstrated that hyperglycemia could increase the risk of poor outcomes such as infections and cardiovascular disease following lumbar spinal surgery. A recent study assessed the effect of glycemic control on perioperative complications in patients undergoing lumbar surgery and showed that poor glycemic control in patients with diabetes receiving degenerative lumbar spine surgery could increase the risk of acute complications and poor outcomes.11 However, Arnold et al12 reported that DM would not increase the risk of postoperative complications. Controversies regarding whether diabetes could increase the rate of complications associated with spinal surgery still exist. Moreover, the sample sizes of these studies were relatively small, which could restrict the conclusions. The purpose of the present study was to conduct a meta-analysis to assess the impact of DM on surgical outcomes in patients who receive spinal surgery.
Materials and methods
Search strategy
We conducted the present study in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. A computerized search was performed in the MEDLINE database, the Cochrane CENTRAL database, ScienceDirect, EMBASE, and Google scholar for relevant published studies through May 2018. The following search terms were used to maximize the search specificity and sensitivity: spine, surgery, and diabetes. The search strategy is presented in Figure 1, and included only studies conducted on humans for all published, unpublished, and ongoing trials. In addition, the WHO International Clinical Trials Registry Platform, the UK National Research Register Archive, and Current Controlled Trials were used for a further manual search for articles from Congresses that may have been missed in the database search from their inception to May 2018. The reference lists of all full-text papers were examined to identify any initially omitted studies.
  | Figure 1 Flowchart of the study selection process. |
Selection criteria
The studies that met the following criteria were included in the meta-analysis: 1) the study design was a cohort or case–control study; 2) the study included patients with and those without diabetes who were undergoing spinal surgery; 3) the study reported outcome measures, operation data, clinical function scores, recovery rates, and postoperative complications; and 4) the study may have included any other outcomes.
The exclusion criteria included reviews, letters, case reports, systematic reviews, and studies that were unrelated to our topics.
Study selection
Two authors independently screened the article titles and abstracts based on the eligibility criteria, and intensive reading of the full texts was performed when the studies met the inclusion criteria. When a study could not be excluded immediately, disagreements were resolved by consensus with the senior investigator.
Data extraction
Data extraction was conducted according to the PRISMA statement, and data from eligible peer-reviewed articles were extracted by two independent authors. Any discrepancies between the two reviewers were resolved by discussion and consensus or, if necessary, by third-party adjudication. Authors of the studies were contacted for missing data or further information when necessary. The following outcomes were extracted from the included publications: 1) demographic data on the participants; 2) operation data, clinical function scores, recovery rates, and postoperative complications; and 3) any other outcomes mentioned in the individual studies.
Assessment of methodological quality
We assessed the methodological quality of included studies using the modified Newcastle–Ottawa Scale (NOS). This scale consists of three items for cohort study reports: patient selection, comparability of the intervention/control group, and outcome assessment. The quality scale ranges from 0 to 9 points. Articles were considered to be of high quality if the NOS score was >5 points.
Statistical analysis
We used Review Manager 5.1 software for Windows (RevMan Version 5.1; The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) for data analysis. Dichotomous outcomes are expressed as ORs with 95% CIs; continuous outcomes are expressed as the mean differences (MDs). Before the original data were synthesized, we used Cochran’s Q chi-squared test and the I2 statistic to assess the heterogeneity across studies. P<0.1 or I2 >50% was defined as significant heterogeneity. If substantial heterogeneity existed, a random-effects model (the DerSimonian–Laird method) was used; otherwise, a fixed-effects model (the Mantel–Haenszel method) was preferred to summarize the pooled data. When heterogeneity was present, a sensitivity analysis was conducted to identify the potential sources. Since the number of included studies was <10, an assessment of publication bias was not performed. P<0.05 was considered statistically significant.
Results
Search results
The search strategy identified 738 citations as potentially relevant literature reports. By scanning the titles and abstracts, 712 reports were excluded because of duplication or irrelevancy, because they were case reports or reviews, or because they were not comparative studies. Ultimately, 24 studies6,8–30 were eligible for data extraction and meta-analysis (Table 1). No additional studies were obtained after the reference review. The search process is shown in Figure 1.
  | Table 1 Characteristics of included studies |
Study characteristics
The characteristics of the 24 included studies, which were published between 1993 and 2017, are shown in Table 1. The sample sizes of these studies ranged from 52 to 256,899 patients. Statistically similar baseline characteristics, such as the mean age and gender, were observed between both groups.
Quality assessment and level of evidence
Four of the included studies were prospective controlled studies, and 20 studies were retrospective controlled studies. The NOS scores were 5–8 for the included studies. The methodological quality assessment is presented in Table 1.
Meta-analysis outcomes
Blood loss
Usable data on blood loss were provided in 10 trials.6,14,16,18,19,24,25,27,29,30 No significant heterogeneity was observed, and a fixed-effects model was used (I2=36%, P=0.10). Pooling of the results demonstrated that blood loss in the DM group was not significantly greater than that in the non-DM group (MD=0.55, 95% CI: –8.15 to 9.26, P=0.90; Figure 2).
  | Figure 2 Forest plot showing blood loss. |
Operation time
The operation time was provided in eight trials.6,14,18,19,24,25,27,30 No significant heterogeneity was observed, and a fixed-effects model was used (I2=0%, P=0.47). Pooling of the results demonstrated that the operation time in the DM group was not significantly longer than that in the non-DM group (MD=1.36, 95% CI: −2.22 to 4.94, P=0.46; Figure 3).
  | Figure 3 Forest plot showing operation time. |
Length of hospital stay
Data from five studies were available to examine the length of hospital stay.8,18,24,27,29 Significant heterogeneity was observed, and a random-effects model was used (I2=91%, P<0.001). Pooling of the results demonstrated that the length of hospital stay in the DM group was significantly longer than that in the non-DM group (MD=1.00, 95% CI: 0.29–1.71, P=0.02; Figure 4).
  | Figure 4 Forest plot showing length of hospital stay. |
Mortality
Six studies reported postoperative mortality.8,9,11,18,20,29 No significant heterogeneity was observed (I2=0%, P=0.48); therefore, a fixed-effects model was used. Pooling of the results demonstrated that the incidence of postoperative mortality in the DM group was significantly higher than that in the non-DM group (OR=1.44, 95% CI: 1.33–1.56, P<0.001; Figure 5).
  | Figure 5 Forest plot showing mortality. |
Reoperation
The number of patients who underwent reoperation was provided in six studies.12,16,19,22,27,30 No significant heterogeneity was observed (I2=0%, P=0.56); therefore, a fixed-effects model was used. Pooling of the results demonstrated that the incidence of reoperation in the DM group was not significantly higher than that in the non-DM group (OR=1.18, 95% CI: 0.99–1.40, P=0.07; Figure 6).
  | Figure 6 Forest plot showing reoperation. |
Infection
Seventeen studies reported the postoperative incidence of infection.8–13,15,18–21,24–27,29,30 Significant heterogeneity was observed, and a random-effects model was used (I2=61%, P=0.0005). The meta-analysis revealed that the postoperative incidence of infection was significantly higher than that in the non-DM group (OR=1.88, 95% CI: 1.46–2.42, P<0.001; Figure 7).
  | Figure 7 Forest plot showing infection. |
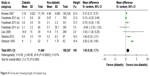
Deep venous thrombosis (DVT)
Five studies reported the postoperative incidence of DVT.8,11,12,19,20 No significant heterogeneity was observed, and a fixed-effects model was used (I2=6%, P=0.37). The meta-analysis revealed that the postoperative incidence of DVT was significantly higher than that in the non-DM group (OR=1.49, 95% CI: 1.40–1.58, P<0.001; Figure 8).
  | Figure 8 Forest plot showing deep venous thrombosis. |
Discussion
The present study indicates that diabetes increases the risks of postoperative mortality, surgical site infection, DVT, and prolonged hospitalization time after spinal surgery. Four prospective controlled studies and 20 retrospective controlled studies were included. Although the NOS scores of the included studies are high (ranging from 5 to 8), the limitations inherent in this methodology weakened the level of evidence and should be considered when interpreting the findings of the present meta-analysis.
In 2010, the number of deaths caused by DM reached approximately 1.3 million worldwide, and the disease burden is several times greater in the elderly.11,31 A large proportion of patients undergoing degenerative spine surgery are elderly, and therefore the impact of DM on surgical outcomes is of great interest. Currently, only a few studies have described the outcomes of spinal surgery in patients with DM. However, previous reports have relatively small sample sizes, which limit the conclusions that can be widely applied to clinical practice.6,7,30
Our meta-analysis demonstrates that patients with diabetes undergoing spinal surgery had increased odds of mortality. However, there is no clear and direct evidence to confirm that DM is an independent risk factor for postoperative mortality. Comorbidities including cardiovascular and cerebrovascular diseases, respiratory diseases, urinary system diseases, and nervous system diseases may have had additional influences on the outcomes for patients following spinal surgery, according to some studies.11,12,18,25 Guzman et al11 and Farrell and Moran32 indicated that people with DM are more likely to have these comorbidities. Furthermore, Hamdan et al33 and Carson et al34 reported that comorbidities could increase inpatient mortality following spinal surgery. Therefore, a significant difference exists between the mortality rate of patients with diabetes undergoing spinal surgery and that of patients without diabetes.
No significant difference was found in the reoperation rate between patients with and without DM following spinal surgery. The reasons for reoperation included dysphagia (following cervical operation), malpositioning of the implant, or a postoperative deformity. Some studies12,19 have shown that reoperation is not closely related to the presence of diabetes.
We also found that the risk of surgical site infection and DVT was higher in patients with DM following spinal surgery than in patients without DM. Many risk factors affect wound healing, including a lack of platelet-derived growth factor, neutropenia, tissue hypoxia, and microvascular disease.35,36 In addition, fibroblasts and collagen deficiency can lead to delayed wound healing.37 Immune dysfunction is caused by the effects of DM increasing the probability of infection of the surgical site. DM is a chronic systemic disease characterized by high concentrations of glucose in the blood. Jones and Mitchell38 also reported that a high concentration of glucose in blood vessels leads to increased vascular endothelial damage, which results in a higher risk of venous thrombosis. Therefore, patients with DM are more likely to develop venous thrombosis than those without DM following spinal surgery.
The results showed no significant difference in the operation time or blood loss between patients with and those without diabetes following spinal surgery, which is consistent with the results of several studies.6,16,18,19,24,27,29,30 However, the length of hospital stay for patients with DM was longer than that for patients without diabetes, which may be related to the treatment of surgical site infections and other complications. Some papers have reported that the prolonged hospitalization time is related to the further regulation of blood glucose.27
There are some limitations in our meta-analysis: 1) no specific type of DM has a greater impact on spinal surgery, and it is not known whether spinal surgery will affect HbA1c; 2) the small sample sizes in the literature may have affected the final results; 3) differences in diabetes duration, treatment, complications, or comorbidities could have affected the findings and, similarly, the definition of diabetes was not standardized across the included studies and therefore it is likely that each study cohort may have affected the findings of the study; 4) this article did not compare the various types of spinal surgeries in detail, and different surgical methods may prolong the operation time and increase blood loss and the probability of surgical site infections, which may have impacted the evaluated results; and 5) most of the studies were performed on patients of the same nationality, and the lack of a regional comparison may affect the generalization of the results.
Conclusion
The effect of spinal surgery in patients with DM is more prominent and serious than that in patients without diabetes, and the mortality rate, surgical site infection rate, risk of venous thrombosis, and length of hospital stay are increased in patients with diabetes. Given this finding, physicians should pay attention to this risk to avoid complications.
Author contributions
WL and RS conducted the literature search and determined studies for exclusion and inclusion. WL and HJ extracted data from the included studies, performed the meta-analysis, and drafted the manuscript. WL, RS, and XM conceived the idea for the study, designed the study, and critically revised the manuscript for important intellectual content. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Engelgau MM, Geiss LS, Saaddine JB, et al. The evolving diabetes burden in the United States. Ann Intern Med. 2004;140(11):945–950. | ||
Houten JK, Lenart C. Diabetes and cervical myelopathy. J Clin Neurosci. 2016;27:99–101. | ||
Asadian L, Haddadi K, Aarabi M, Zare A. Diabetes mellitus, a new risk factor for lumbar spinal stenosis: a case-control study. Clin Med Insights Endocrinol Diabetes. 2016;9:1–5. | ||
Kim KT, Cho DC, Sung JK, Kim CH, Kang H, Kim DH. Changes in HbA1c levels and body mass index after successful decompression surgery in patients with type 2 diabetes mellitus and lumbar spinal stenosis: results of a 2-year follow-up study. Spine J. 2017;17(2):203–210. | ||
Imajo Y, Taguchi T, Neo M, et al. Complications of spinal surgery for elderly patients with lumbar spinal stenosis in a super-aging country: An analysis of 8033 patients. J Orthop Sci. 2017;22(1):10–15. | ||
Kawaguchi Y, Matsui H, Ishihara H, Gejo R, Yasuda T. Surgical outcome of cervical expansive laminoplasty in patients with diabetes mellitus. Spine (Phila Pa 1976). 2000;25(5):551–555. | ||
Satake K, Kanemura T, Matsumoto A, Yamaguchi H, Ishikawa Y. Predisposing factors for surgical site infection of spinal instrumentation surgery for diabetes patients. Eur Spine J. 2013;22(8):1854–1858. | ||
Browne JA, Cook C, Pietrobon R, Bethel MA, Richardson WJ. Diabetes and early postoperative outcomes following lumbar fusion. Spine (Phila Pa 1976). 2007;32(20):2214–2219. | ||
Cook C, Tackett S, Shah A, et al. Diabetes and perioperative outcomes following cervical fusion in patients with myelopathy. Spine (Phila Pa 1976). 2008;33(8):E254–E260. | ||
Appaduray SP, Lo P. Effects of diabetes and smoking on lumbar spinal surgery outcomes. J Clin Neurosci. 2013;20(12):1713–1717. | ||
Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976). 2014;39(19):1596–1604. | ||
Arnold PM, Fehlings MG, Kopjar B, et al. Mild diabetes is not a contraindication for surgical decompression in cervical spondylotic myelopathy: results of the AOSpine North America multicenter prospective study (CSM). Spine J. 2014;14(1):65–72. | ||
Arinzon Z, Adunsky A, Fidelman Z, Gepstein R. Outcomes of decompression surgery for lumbar spinal stenosis in elderly diabetic patients. Eur Spine J. 2004;13(1):32–37. | ||
Armaghani SJ, Archer KR, Rolfe R, Demaio DN, Devin CJ. Diabetes is related to worse patient-reported outcomes at two years following spine surgery. J Bone Joint Surg Am. 2016;98(1):15–22. | ||
Chen S, Anderson MV, Cheng WK, Wongworawat MD. Diabetes associated with increased surgical site infections in spinal arthrodesis. Clin Orthop Relat Res. 2009;467(7):1670–1673. | ||
Cho W, Lenke LG, Bridwell KH, et al. Comparison of spinal deformity surgery in patients with non-insulin-dependent diabetes mellitus (NIDDM) versus controls. Spine (Phila Pa 1976). 2012;37(16):E978–E984. | ||
Dokai T, Nagashima H, Nanjo Y, Tanida A, Teshima R. Surgical outcomes and prognostic factors of cervical spondylotic myelopathy in diabetic patients. Arch Orthop Trauma Surg. 2012;132(5):577–582. | ||
Freedman MK, Hilibrand AS, Blood EA, et al. The impact of diabetes on the outcomes of surgical and nonsurgical treatment of patients in the spine patient outcomes research trial. Spine (Phila Pa 1976). 2011;36(4):290–307. | ||
Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative complications of lumbar instrumentation and fusion in patients with diabetes mellitus. Spine J. 2003;3(6):496–501. | ||
Golinvaux NS, Varthi AG, Bohl DD, Basques BA, Grauer JN. Complication rates following elective lumbar fusion in patients with diabetes: insulin dependence makes the difference. Spine (Phila Pa 1976). 2014;39(21):1809–1816. | ||
Hikata T, Iwanami A, Hosogane N, et al. High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J Orthop Sci. 2014;19(2):223–228. | ||
Kim CH, Chung CK, Shin S, et al. The relationship between diabetes and the reoperation rate after lumbar spinal surgery: a nationwide cohort study. Spine J. 2015;15(5):866–874. | ||
Kim HJ, Moon SH, Kim HS, et al. Diabetes and smoking as prognostic factors after cervical laminoplasty. J Bone Joint Surg Br. 2008;90(11):1468–1472. | ||
Liao JC, Chen WJ, Chen LH, Niu CC. Postoperative wound infection rates after posterior instrumented spinal surgery in diabetic patients. Chang Gung Med J Sep. 2006;29(5):480–485. | ||
Machino M, Yukawa Y, Ito K, et al. Impact of diabetes on the outcomes of cervical laminoplasty: a prospective cohort study of more than 500 patients with cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2014;39(3):220–227. | ||
Maloney PR, Halasz SR, Mallory GW, et al. The effect of diabetes mellitus on 30-day outcomes following single-level open lumbar microdiscectomy: an aged-matched case-control study. J Neurosurg Sci. 2017;61(1):1–7. | ||
Sharma A, Muir R, Johnston R, Carter E, Bowden G, Wilson-Macdonald J. Diabetes is predictive of longer hospital stay and increased rate of complications in spinal surgery in the UK. Ann R Coll Surg Engl. 2013;95(4):275–279. | ||
Silverstein MP, Miller JA, Xiao R, Lubelski D, Benzel EC, Mroz TE. The impact of diabetes upon quality of life outcomes after lumbar decompression. Spine J. 2016;16(6):714–721. | ||
Simpson JM, Silveri CP, Balderston RA, Simeone FA, An HS. The results of operations on the lumbar spine in patients who have diabetes mellitus. J Bone Joint Surg Am. 1993;75(12):1823–1829. | ||
Takahashi S, Suzuki A, Toyoda H, et al. Characteristics of diabetes associated with poor improvements in clinical outcomes after lumbar spine surgery. Spine (Phila Pa 1976). 2013;38(6):516–522. | ||
Bhutani J, Bhutani S. Worldwide burden of diabetes. Indian J Endocrinol Metab. 2014;18(6):868–870. | ||
Farrell C, Moran J. Comparison of comorbidities in patients with pre-diabetes to those with diabetes mellitus type 2. Ir Med J. 2014;107(3):72–74. | ||
Hamdan AD, Saltzberg SS, Sheahan M, et al. Lack of association of diabetes with increased postoperative mortality and cardiac morbidity: results of 6565 major vascular operations. Arch Surg. 2002;137(4):417–421. | ||
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2002;40(3):418–423. | ||
Bagdade JD, Stewart M, Walters E. Impaired granulocyte adherence. A reversible defect in host defense in patients with poorly controlled diabetes. Diabetes. 1978;27(6):677–681. | ||
Goodson WH 3rd, Hung TK. Studies of wound healing in experimental diabetes mellitus. J Surg Res. 1977;22(3):221–227. | ||
Twigg SM, Chen MM, Joly AH, et al. Advanced glycosylation end products up-regulate connective tissue growth factor (insulin-like growth factor-binding protein-related protein 2) in human fibroblasts: a potential mechanism for expansion of extracellular matrix in diabetes mellitus. Endocrinology. 2001;142(5):1760–1769. | ||
Jones EW, Mitchell JR. Venous thrombosis in diabetes mellitus. Diabetologia. 1983;25(6):502–505. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
