Back to Journals » Patient Preference and Adherence » Volume 16
The Association Between the Prevalence, Medication Adherence and Control of Hypertension and the Prevalence of Mild Cognitive Impairment in Rural Northern China: A Cross-Sectional Study
Authors Ma LY, He F, Liu S, Wang XD, Gao Y, Shi Z, Niu J, Ji Y
Received 28 November 2021
Accepted for publication 28 January 2022
Published 22 February 2022 Volume 2022:16 Pages 493—502
DOI https://doi.org/10.2147/PPA.S351588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Ling-Yun Ma,1,* Fangfang He,2,* Shuai Liu,3 Xiao-Dan Wang,3 Yanqin Gao,2 Zhihong Shi,3,4 Jianping Niu,2 Yong Ji1,3,4
1Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Neurology, The Second Affiliated Hospital of Xiamen Medical College, Xiamen, People’s Republic of China; 3Tianjin Key Laboratory of Cerebrovascular and of Neurodegenerative Diseases, Department of Neurology, Tianjin Dementia Institute, Tianjin Huanhu Hospital, Tianjin, People’s Republic of China; 4China National Clinical Research Center for Neurological Diseases, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianping Niu; Yong Ji, Tel +8618059218208 ; +8613612048681, Email [email protected]; [email protected]; [email protected]
Introduction: High blood pressure is one of the main modifiable risk factors for dementia. However, it remains unclear whether lowering the blood pressure effectively prevents cognitive impairment. Our objective was to explore the association between the prevalence, medication adherence and control of hypertension and mild cognitive impairment (MCI) among elderly individuals in northern China.
Methods: A two-stage clustering sampling method was used, and 9036 participants aged ≥ 65 years were included in the analysis. The Mini-Mental State Examination and activities of daily living were used to assess participants’ cognitive function. Demographic characteristics (gender, age, marital status, education level, occupation), history and duration of hypertension, use of antihypertensive medications (AHMs) and its control effect were obtained.
Results: The prevalence of MCI in all participants was 18.1%, and the prevalence of MCI was significantly higher in hypertensive subjects than in normotensive subjects (19.7% vs 16.2%, P < 0.01). Furthermore, in hypertensive patients, the prevalence of MCI was lower in those with good adherence (17.3%) than in those with poor adherence (23.7%, P < 0.01) and lower in those controlled (16.5%) than in those with uncontrolled adherence (20.8%, P < 0.01). In univariate analyses, being female gender, increased age, agriculture occupation, unmarried and widow, less than primary school and middle school were associated with MCI prevalence. The assessment of the hypertensive patients revealed the adjusted OR (95% CI) of having MCI in those with poor adherence to AHMs was 1.32 (1.14– 1.54) compared with those having good adherence.
Conclusion: There is an association between the prevalence of hypertension, adherence to AHMs and MCI, suggesting that hypertensives should be screened for MCI to provide improved diagnoses and optimal therapeutics for cognitive decline prevention, especially in poor AHM adherence.
Keywords: elderly individuals, hypertension, medication adherence, mild cognitive impairment
Introduction
With the expected increase in the elderly population, the prevalence of hypertension is on the rise; this figure may increase to 1.56 billion by 2025. Therefore, both the treatment and control of hypertension are considered important public health issues for the prevention of traditional risk factors such as stroke, cardiovascular events, and other diseases.1,2
Hypertension and mild cognitive impairment (MCI) are two of the most prevalent and devastating diseases associated with aging, affecting millions of people worldwide. The increasing life expectancy of older adults in modern societies poses a major public health problem.3
Accumulating epidemiological and mechanistic evidence has shown that hypertension is a possible risk factor for dementia, Alzheimer’s disease (AD) and mild cognitive impairment (MCI).4–10 Therefore, an increasing number of studies have focused on whether antihypertensive medications (AHMs) and blood pressure control can slow cognitive decline and prevent dementia. Observational studies have shown that individuals with pharmacologically controlled hypertension decline less than people with uncontrolled or untreated hypertension.11 A beneficial effect of antihypertensive medication on cognitive decline and dementia incidence is suggested by several observational studies with short/medium-term follow-ups (ie between 412 years).12 Related studies in China showed that the incidence of MCI was significantly higher in hypertensive patients than in normotensive patients, that there was a correlation between AHMs and MCI, and that the incidence of MCI was significantly higher in hypertensive patients with poor blood pressure control (BP) than in those with good BP control.13,14 But a recent meta-analysis failed to demonstrate that antihypertensive treatment is associated with a reduction in cognitive decline.15 Thus, more research is needed to elucidate the causal link between hypertension and cognition and to better understand the role of medication in the observed associations.
With an aging population, the prevalence of dementia and MCI has been rapidly increasing over the past few decades in China.16,17 Currently, in the elderly population, MCI patients are at higher risk of developing dementia; thus, mild cognitive impairment has become an important public health issue.18,19 Therefore, hypertension, as a major controllable factor, is critical to investigate the current status of MCI. Hypertension and MCI have changed dramatically in the last decade, but there are fewer studies on the effects of hypertension and AHMs on MCI. The current study aims to examine the association between the prevalence, adherence and control of hypertension and the increased risk of mild cognitive impairment in participants over 65 years of age in rural areas in Tianjin, China.
Methods
Participants
The current study is a cross-sectional, population-based survey conducted across 104 communities, aiming to investigate the association of hypertension status and cognitive impairment in Ji County from April to December 2019. The participants were chosen from the database of Health Bureau of Ji County. Every investigation randomly selected 70 villages belonging to the five townships of Ji County. The following inclusion criteria were used: subjects were aged ≥65 years, and were legal residents in Ji County for at least 5 years preceding the survey date who accepted to participate. The detailed data cleaning procedure and quality control is presented in Figure 1. The researchers who participated in the survey had received at least five years of medical education. Training of investigators was centralized to ensure the uniformity in and the quality of field activities. The investigations were aided by the medical staff of the township health center. Prior to conducting this survey, a pilot study surveyed one village to test the epidemiological methods.
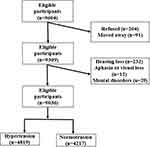 |
Figure 1 Flowchart of subjects recruited into the study. |
Data Collection and Measurement
All data were collected using face-to-face interviews. A standardized questionnaire was designed and developed by the research team based on the relevant literature. On the basis of informed consent, a face-to-face survey was conducted in the home by medical personnel who had received special training and were qualified. The survey contents included the following aspects. Age was divided into three stages: 65–70 years, 71–74 years, 75–79 years, 80–85 years and equal to or greater than 75 years. Education levels included less than primary school, primary school and middle school and above. Marital status was coded as single, married, or widow/divorced; occupational status was coded as agriculture and nonagriculture.
Definitions
The blood pressure (BP) values of the individuals were obtained with three measurements taken after resting for at least 5 min. Participants were advised to avoid smoking, caffeinated drinks, alcohol, and exercise for at least 30 min before measurement. Measurement was taken from the unclothed right arm of the person in a sitting position. Diastolic and systolic blood pressures were measured twice with a resting interval between the two measurements. The average of the two readings was calculated to record the blood pressure value for each participant. If the difference between the two measurements exceeded 10 mm Hg, the participant’s blood pressure was measured a third time, and the average of the three measurements was calculated as the final measurement. A trained observer calculated the average of the three recordings as the final measurement.
Hypertension was defined as systolic BP (SBP) ≥140 mmHg and/or diastolic BP (DBP) ≥90 mmHg or the use of antihypertensive medicine within 2 weeks.20 AHMs adherence was measured using Chinese version of Morisky, Green and Levine (MGL) medication adherence scale, 22 which was widely used and has been demonstrated to be valid. It consisted of four “yes” or “no” questions. A positive answer was graded 1, whereas a negative answer was graded 0. Participants were considered adherent to treatment if they scored 0, and nonadherent if they scored 1 or above.21 For patients who were under 80 years of age, blood pressure <140/90 mmHg was considered controlled, whereas for patients aged 80 years or above, blood pressure <150/90 mmHg was considered controlled. Similarly, for the patients with both hypertension and diabetes mellitus, blood pressure <140/80 mmHg, and for patients with kidney, eye and cerebrovascular damage, blood pressure <130/80 mmHg was considered controlled.22
Trained neurologists evaluated each participant’s cognitive function using the Mini-Mental State Examination (MMSE) and the Diagnostic and Statistical Manual of Mental Disorders (IV Edition) criteria.23 MCI was defined as an MMSE score <17 for illiterate subjects, <20 for subjects with 1–6 years of education and <24 for subjects with ⩾7 years of education, with intact ADL. Impairment and disability were evaluated using the ADL-20. This scale consists of 20 items from four major categories of basic activities of daily living (ADL).24 It has been reported that ADL-20 is useful as a comprehensive measure of ADL in elderly individuals with a variety of handicaps. To assess the parameter “ADL deterioration,” the study physician asked the patient about a decline of independence in the prior two weeks regarding “bathing,” “dressing,” “mobility,” “feeding,” “toilet hygiene,” and “incontinence.” For the parameter “coherence of history,” the study physicians provided a subjective judgment (yes/no), whether they considered the history given by the patient as coherent (no discrepancy to other information, such as health records or histories by proxies).
Statistical Analysis
Sociodemographic data of the respondents were analyzed using descriptive statistics. Continuous variables are expressed as the mean and SD, and categorical variables are expressed as the frequency (%). The t-test and χ2-test were used to assess differences in the continuous and categorical variables, respectively, unless otherwise specified. Logistic regression was used to calculate the unadjusted and adjusted odds ratios (ORs) and the 95% confidence intervals (95% CIs) of the prevalence, adherence and control of hypertension, and the prevalence of MCI. All P values and CIs were estimated in a 2-tailed fashion. Differences were considered statistically significant at P<0.05. Data were analyzed using SPSS version 13.0 (SPSS, Inc., Chicago, IL, USA).
Results
The characteristics of the total participants are shown in Table 1. The study population included 9036 individuals aged 65 years or older. The mean age of the participants was 74.8±7.0 years, with a range from 65 to 98 years. Hypertensive subjects were significantly older (75.1±7.2 vs 74.4±6.5, P < 0.01), compared to non-hypertensive subjects as in Table 1. Overall, the prevalence of MCI and hypertension were 18.1% and 53.3%, respectively.
 |
Table 1 Characteristics of Study Subjects |
As shown in Figure 2, the prevalence of MCI was higher in hypertensive subjects than in normotensive subjects (19.7% vs 16.2%, P < 0.01). In addition, uncontrolled hypertensive subjects had a significantly higher prevalence of MCI than controlled subjects (20.8% vs 16.5%, P <0 0.01). Moreover, the prevalence of MCI revealed significant differences between good adherence to AHMs and poor adherence (17.3% vs 23.7%, P <0.01).
 |
Figure 2 Prevalence of mild cognitive impairment in total hypertensive subjects and those with high and low adherence and controlled blood pressure. *p<0.05; **p<0.01 comparison of MCI prevalence. |
Table 2 shows the univariate analyses of selected demographic variables for MCI. Being female was associated with a higher prevalence than male (P <0.01). The prevalence of MCI increased markedly with increasing age from 12.2 to 41.4% (P <0.01). Agriculture occupation was associated with a higher prevalence than non- agriculture occupation (P <0.05). What is more, the prevalence of MCI was higher in patients with unmarried and widow, less than primary school and middle school and above (P <0.01). No difference was found between different handedness, duration years of hypertension and MCI.
 |
Table 2 Basic Characteristics of Hypertensive Patients Among MCI and Cognitively Normal |
Table 3 shows the unadjusted and adjusted associations between the prevalence, adherence and control of hypertension and the prevalence of MCI. Multivariate logistic analyses were used to explore the association of risk factors with MCI. Overall, For the prevalence of MCI (as a dichotomous variable), after adjusting for gender, age, education level, marital status, occupational status, the OR (95% CI) of having MCI was 1.39 (1.24–1.56) in those with hypertension compared with those normotensive individuals. In the hypertensive patients, the adjusted OR (95% CI) of having MCI in those with poor adherence to AHMs was 1.32 (1.14–1.54) compared with those with good adherence. However, the difference between the uncontrolled hypertensive patients and those controlled hypertensive patients was not significant.
 |
Table 3 Association Between the Prevalence, Adherence and Control of Hypertension and the Prevalence of MCI in Participant |
Discussions
This is a population-based, cross-sectional study aimed at investigating the relationship between the use of AHMs in elderly hypertension and the risk of MCI. The main results showed that the prevalence of MCI was significantly higher in hypertensive subjects than in normotensive subjects and significantly lower in hypertensive subjects with good adherence than in those with poor adherence. In addition, adherence to AHMs, being female gender, increased age, agriculture occupation, unmarried and widow, less than primary school and middle school were associated with MCI prevalence.
Both positive and negative relationships have been reported between hypertension and cognitive decline. However, more findings of the current study are in accordance with previous authors who have reported a positive relationship between hypertension and cognitive decline. Budge et al25 reported that blood pressure was negatively related to the MMSE score in an elderly community. A cross-sectional study by Paran et al26 reported that increasing blood pressure was related to a reduced risk of cognitive impairment in an elderly population aged 70–85 years.
The negative impact of hypertension on cognitive function is best understood in terms of the brain’s need for a continuous blood supply. The brain is a highly vascularized organ, and continuous perfusion is essential to meet its high metabolic demands. Hypertension alters the structural and molecular composition of the cerebral vasculature, disrupting the homeostatic mechanisms that ensure an adequate blood supply to the brain at all times.27,28 Thus, damage to the cerebral vascular system affects the delivery of oxygen and glucose to maintain normal neuronal function, as well as the removal of metabolic waste and toxic proteins. These alterations make the brain more susceptible to ischemic damage, the development of white matter disorders and neurodegenerative diseases.29,30
A recent national cross-sectional study found the prevalence of dementia and mild cognitive impairment in Chinese adults aged 60 years and older, with a clear prevalence of 6.04% for dementia and 15.07 million patients and 15.54% for mild cognitive impairment,17 which is similar to our findings. In the current study, the prevalence of MCI among individuals ≥65 years of age was significantly higher in hypertensive subjects than in normotensive subjects (19.7% vs 16.2%), which were somewhat higher than that Study in urban China (16.5% vs 13.1%).13 In line with our findings was that adherence to AHMs was a critical factor in managing MCI. In addition, we failed to observe differences in the prevalence of MCI between controlled and uncontrolled hypertensives, which is inconsistent with the results of the study conducted in Beijing.
Many factors may clearly influence MCI prevalence in hypertensive patients, such as treatment. Among hypertensive patients in the present study, ORs for the prevalence of MCI in poor adherence hypertensive patients compared with all good adherence hypertensive patients was 1.32. However, the difference between patients with uncontrolled hypertension and those with controlled hypertension was not significant. Taken together, the results suggested that hypertension treatment by itself appears to have a protective effect against mild cognitive impairment. More studies on the protective effect of antihypertensive therapy against cognitive impairment have been reported. In agreement with these data, observational studies31 showed that AHMs may be beneficial in preventing cognitive decline and dementia. Haring32 found that hypertension or antihypertensive adherence was associated with an increased risk of developing cognitive decline. A 4-year follow-up study by Tzourio et al33 found that cognitive decline occurred in a relatively short time period and that the risk was highest in untreated hypertensive patients in individuals with high blood pressure. Then, Tzourio et al34 confirmed the association between active treatment and the reduced risk of both dementia and cognitive decline, and the treatment group showed a 19% reduction in the risk of cognitive decline. Adherence to AHMs was a critical factor in managing blood pressure and preventing related complications. However, onset of overt dementia is typically associated with spontaneous lowering of blood pressure,35 with a potential risk of overtreatment if drug therapy is not adequately modified. It has been hypothesized that, owing to brain hypoperfusion, hypotension due to overtreatment may adversely affect cognitive outcome in dementia.36
We also found an increase in the prevalence of MCI with age. Ageing is accompanied by changes in the brain, including general atrophy particularly in the hippocampus, an imbalance of amyloid-β production and degradation, activation of inflammation, and frailty of neurons in areas related to memory,37 which was also consistent with the reports of Li et al.38 In other study, significant gender differences were found showing a higher prevalence in women than men.39 Increased prevalence in women might be due to a reduction of oestrogen and related hormones after menopause, as well as a difference in brain structure.40 In addition, marital status was also associated with dementia; unmarried or loss of a spouse might result in loneliness and less communication or mutual assistance, which are factors that impair cognition in older adults.41 Dartigues et al42 suggested that occupational status should be taken into consideration when studying brain aging. Consistent with previous studies, our study found that people with physical labour were more likely to have MCI.43 However, control did not seem to serve as a protective factor in this situation. A U-shaped relation was reported from the Kungsholmen project and the East Boston study, in which low SBP was defined as below 130 mm Hg.44,45 Duke population studies of elderly people could replicate this finding only among Caucasians.46 One reason for these inconsistent findings may be the systolic and diastolic blood pressure to analyze the MCI. However, we have not quantified the total number of BPs, which is necessary in future studies.
Limitations
The current study was a population-based cross-sectional study representing a large sample from northern China. In general, there was an excellent response rate and a low percentage of missing data. Notwithstanding, the current study has some limitations. Limitations of the study include the properties of the cross-sectional study and recall bias of the self-report questionnaire. Additionally, detailed information on the type of antihypertensive medication used should have been collected, as this may be an important covariate for the study analysis. We also were not able to collect all risk factors for participants in the survey, and the list of risk factors in MCI survivors did not include many important risk factors (eg, diet, physical activity). The advantages of our study include: (1) very large sample size ensuring sufficient number of rural study participants; (2) an excellent response rate and a low percentage of missing data.
Conclusion
In conclusion, the present study showed a positive relationship between the prevalence of hypertension, poor adherence to AHMs and an increased risk of MCI in rural northern China. Besides, MCI is associated with gender, age, education level and status, and we hoped to have the opportunity to conduct another further in-depth investigation and research about it.
Ethics Approval
This study was conducted in accordance with the Declaration of Helsinki. All procedures performed in studies involving human participants followed the ethical standards of the Ethical Institutional Consideration. The protocol for the current study was reviewed and approved by the ethics committee at Tianjin Huanhu Hospital (2019–40). Informed consent was obtained from each subject either directly or from his or her guardian.
Acknowledgments
We sincerely appreciate the National Key Research and Development Program of China. We would also like to thank the patients for their participation in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation [grant number 8217051007], Science and Technology Project of Tianjin Municipal Health and Health [grant number ZC20121].
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. doi:10.1136/bmj.b1665
2. Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–1518. doi:10.1016/s0140-6736(08)60655-8
3. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi:10.1161/01.cir.0000441139.02102.80
4. Gorelick PB, Scuteri A, Black SE, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2011;42(9):2672–2713. doi:10.1161/STR.0b013e3182299496
5. Okusaga O, Stewart MC, Butcher I, et al. Smoking, hypercholesterolaemia and hypertension as risk factors for cognitive impairment in older adults. Age Ageing. 2013;42(3):306–311. doi:10.1093/ageing/afs193
6. Uiterwijk R, Huijts M, Staals J, et al. Subjective cognitive failures in patients with hypertension are related to cognitive performance and cerebral microbleeds. Hypertension. 2014;64(3):653–657. doi:10.1161/hypertensionaha.114.03621
7. Spinelli C, De Caro MF, Schirosi G, et al. Impaired cognitive executive dysfunction in adult treated hypertensives with a confirmed diagnosis of poorly controlled blood pressure. Int J Med Sci. 2014;11(8):771–778. doi:10.7150/ijms.8147
8. Yamaguchi Y, Wada M, Sato H, et al. Impact of nocturnal heart rate variability on cerebral small-vessel disease progression: a longitudinal study in community-dwelling elderly Japanese. Hypertens Res. 2015;38(8):564–569. doi:10.1038/hr.2015.38
9. Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005;4(8):487–499. doi:10.1016/s1474-4422(05)70141-1
10. Abete P, Della-Morte D, Gargiulo G, et al. Cognitive impairment and cardiovascular diseases in the elderly. A heart-brain continuum hypothesis. Ageing Res Rev. 2014;18:41–52. doi:10.1016/j.arr.2014.07.003
11. Elias MF, Goodell AL, Dore GA. Hypertension and cognitive functioning: a perspective in historical context. Hypertension. 2012;60(2):260–268. doi:10.1161/hypertensionaha.111.186429
12. Köhler S, Baars MAE, Spauwen P, et al. Temporal evolution of cognitive changes in incident hypertension. Hypertension. 2014;63(2):245–251. doi:10.1161/HYPERTENSIONAHA.113.02096
13. Wu L, He Y, Jiang B, et al. The association between the prevalence, treatment and control of hypertension and the risk of mild cognitive impairment in an elderly urban population in China. Hypertens Res. 2016;39(5):367–375. doi:10.1038/hr.2015.146
14. Heizhati M, Wang L, Li N, et al. Prevalence of mild cognitive impairment is higher in hypertensive population: a cross-sectional study in less developed northwest China. Medicine. 2020;99(19):e19891–e19891. doi:10.1097/MD.0000000000019891
15. Chang-Quan H, Hui W, Chao-Min W, et al. The association of antihypertensive medication use with risk of cognitive decline and dementia: a meta-analysis of longitudinal studies. Int J Clin Pract. 2011;65(12):1295–1305. doi:10.1111/j.1742-1241.2011.02810.x
16. Chan KY, Wang W, Wu JJ, et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990–2010: a systematic review and analysis. Lancet. 2013;381(9882):2016–2023. doi:10.1016/s0140-6736(13)60221-4
17. Jia L, Du Y, Chu L, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. 2020;5(12):e661–e671. doi:10.1016/s2468-2667(20)30185-7
18. Lyketsos CG, Lopez O, Jones B, et al. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288(12):1475–1483. doi:10.1001/jama.288.12.1475
19. Parekh AK, Goodman RA, Gordon C, et al. Managing multiple chronic conditions: a strategic framework for improving health outcomes and quality of life. Public Health Rep. 2011;126(4):460–471. doi:10.1177/003335491112600403
20. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi:10.1001/jama.289.19.2560
21. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi:10.1097/00005650-198601000-00007
22. Gu D, Reynolds K, Wu X, et al. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension. 2002;40(6):920–927. doi:10.1161/01.hyp.0000040263.94619.d5
23. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi:10.1016/0022-3956(75)90026-6
24. Eto F, Tanaka M, Chishima M, et al. Comprehensive activities of daily living (ADL) index for the elderly. Nihon Ronen Igakkai zasshi. Jpn J Geriatr. 1992;29(11):841–848. doi:10.3143/geriatrics.29.841
25. Budge MM, de Jager C, Hogervorst E, et al. Total plasma homocysteine, age, systolic blood pressure, and cognitive performance in older people. J Am Geriatr Soc. 2002;50(12):2014–2018. doi:10.1046/j.1532-5415.2002.50614.x
26. Paran E, Anson O, Reuveni H. Blood pressure and cognitive functioning among independent elderly. Am J Hypertens. 2003;16(10):818–826. doi:10.1016/s0895-7061(03)01005-7
27. Pires PW, Dams Ramos CM, Matin N, et al. The effects of hypertension on the cerebral circulation. Am J Physiol Heart Circ Physiol. 2013;304(12):H1598–H1614. doi:10.1152/ajpheart.00490.2012
28. Iadecola C, Park L, Capone C. Threats to the mind: aging, amyloid, and hypertension. Stroke. 2009;40(3 Suppl):S40–S44. doi:10.1161/strokeaha.108.533638
29. Sörös P, Whitehead S, Spence JD, et al. Antihypertensive treatment can prevent stroke and cognitive decline. Nat Rev Neurol. 2013;9(3):174–178. doi:10.1038/nrneurol.2012.255
30. Faraco G, Iadecola C. Hypertension: a harbinger of stroke and dementia. Hypertension. 2013;62(5):810–817. doi:10.1161/hypertensionaha.113.01063
31. Rouch L, Cestac P, Hanon O, et al. Antihypertensive drugs, prevention of cognitive decline and dementia: a systematic review of observational studies, randomized controlled trials and meta-analyses, with discussion of potential mechanisms. CNS Drugs. 2015;29(2):113–130. doi:10.1007/s40263-015-0230-6
32. Haring B, Wu C, Coker LH, et al. Abstract 50: hypertension, antihypertensive treatment, sodium intake and cognitive decline. Circulation. 2015;131(suppl_1):A50–A50. doi:10.1161/circ.131.suppl_1.50
33. Tzourio C, Dufouil C, Ducimetière P, et al. Cognitive decline in individuals with high blood pressure: a longitudinal study in the elderly. EVA Study Group. Epidemiology of Vascular Aging. Neurology. 1999;53(9):1948–1952. doi:10.1212/wnl.53.9.1948
34. Tzourio C, Anderson C, Chapman N, et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med. 2003;163(9):1069–1075. doi:10.1001/archinte.163.9.1069
35. Joas E, Bäckman K, Gustafson D, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 2012;59(4):796–801. doi:10.1161/hypertensionaha.111.182204
36. Di Bari M, Pahor M, Franse LV, et al. Dementia and disability outcomes in large hypertension trials: lessons learned from the systolic hypertension in the elderly program (SHEP) trial. Am J Epidemiol. 2001;153(1):72–78. doi:10.1093/aje/153.1.72
37. Xia X, Jiang Q, McDermott J, et al. Aging and Alzheimer’s disease: comparison and associations from molecular to system level. Aging Cell. 2018;17(5):e12802. doi:10.1111/acel.12802
38. Li JQ, Tan L, Wang HF, et al. Risk factors for predicting progression from mild cognitive impairment to Alzheimer's disease: a systematic review and meta analysis of c ysis of cohort studies. J Neurol Neurosur PS. 2016;87(5):476–484. doi:10.1136/jnnp-2014-310095
39. Guo M, Gao L, Zhang G, et al. Prevalence of dementia and mild cognitive impairment in the elderly living in nursing and veteran care homes in Xi’an, China. J Neurol Sci. 2012;312(1–2):39–44. doi:10.1016/j.jns.2011.08.026
40. Snyder HM, Asthana S, Bain L, et al. Sex biology contributions to vulnerability to Alzheimer’s disease: a think tank convened by the women’s Alzheimer’s research initiative. Alzheimers Dement. 2016;12(11):1186–1196. doi:10.1016/j.jalz.2016.08.004
41. Penninkilampi R, Casey AN, Singh MF, et al. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta-analysis. J Alzheimers Dis. 2018;66(4):1619–1633. doi:10.3233/jad-180439
42. Dartigues JF, Gagnon M, Letenneur L, et al. Principal lifetime occupation and cognitive impairment in a French elderly cohort (paquid). Am J Epidemiol. 1992;135(9):981–988. doi:10.1093/oxfordjournals.aje.a116410
43. Alvarado BE, Zunzunegui MV, Del Ser T, et al. Cognitive decline is related to education and occupation in a Spanish elderly cohort. Aging Clin Exp Res. 2002;14(2):132–142. doi:10.1007/bf03324426
44. Guo Z, Fratiglioni L, Winblad B, et al. Blood pressure and performance on the mini-mental state examination in the very old. Cross-sectional and longitudinal data from the Kungsholmen project. Am J Epidemiol. 1997;145(12):1106–1113. doi:10.1093/oxfordjournals.aje.a009073
45. Glynn RJ, Beckett LA, Hebert LE, et al. Current and remote blood pressure and cognitive decline. JAMA. 1999;281(5):438–445. doi:10.1001/jama.281.5.438
46. Bohannon AD, Fillenbaum GG, Pieper CF, et al. Relationship of race/ethnicity and blood pressure to change in cognitive function. J Am Geriatr Soc. 2002;50(3):424–429. doi:10.1046/j.1532-5415.2002.50104.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
