Back to Journals » Cancer Management and Research » Volume 10
The association between long-term conditions and uptake of population-based screening for colorectal cancer: results from two English cohort studies
Authors Kearns B , Chilcott J , Relton C, Whyte S, Woods HB, Nickerson C, Loban A
Received 5 October 2017
Accepted for publication 25 December 2017
Published 28 March 2018 Volume 2018:10 Pages 637—645
DOI https://doi.org/10.2147/CMAR.S153361
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Kenan Onel
Benjamin Kearns,1 Jim Chilcott,1 Clare Relton,1 Sophie Whyte,1 Helen Buckley Woods,1 Claire Nickerson,2 Amanda Loban1
1School of Health and Related Research, University of Sheffield, Sheffield, UK; 2Cancer Screening Programmes, Public Health England, Sheffield, UK
Introduction: Uptake of screening for colorectal cancer (CRC) can reduce mortality, and population-based screening is offered in England. To date, there is little evidence on the association between having a long-term condition (LTC) and CRC screening uptake. The objective of this study was to examine the association between having an LTC and uptake of CRC screening in England with the guaiac fecal occult blood test, with a particular focus on common mental disorders.
Methods: The study was a preregistered secondary analysis of two cohorts: first, a linked data set between the regional Yorkshire Health Study (YHS) and the National Health Service National Bowel Cancer Screening Program (BCSP, years 2006–2014); second, the national English Longitudinal Study of Ageing (ELSA, years 2014–2015). Individuals eligible for BCSP screening who participated in either the YHS (7,142) or ELSA Wave 7 (4,099) were included. Study registration: ClinicalTrials.gov, number NCT02503969.
Results: In both the cohorts, diabetes was associated with lower uptake (YHS odds ratio [OR] for non-uptake 1.35, 95% CI 1.03–1.78; ELSA 1.33, 1.03–1.72) and osteoarthritis was associated with increased uptake (YHS 0.75, 0.57–0.99; ELSA 0.76, 0.62–0.93). After controlling for broader determinants of health, there was no evidence of significantly different uptake for individuals with common mental disorders.
Conclusion: Two large independent cohorts provided evidence that uptake of CRC screening is lower among individuals with diabetes and higher among individuals with osteoarthritis. Further work should compare barriers and facilitators to screening among individuals with either of these conditions. This study also demonstrates the benefits of data linkage for improving clinical decision-making.
Keywords: colorectal cancer, fecal occult blood test, population screening, uptake, depression, anxiety
Introduction
Colorectal cancer (CRC) is a common form of cancer with over 1 million diagnoses globally every year.1 Deaths from CRC are the second most common cause of cancer-related mortality in a number of countries, including the UK, USA, Japan, Australia, Canada, and Germany,2 with a 5-year survival of <50% in the UK.3 Screening for CRC can reduce mortality via earlier detection and treatment. Within England, guaiac fecal occult blood tests (gFOBTs) are currently used to screen biennially for CRC, as part of the English National Health Service (NHS) National Bowel Cancer Screening Program (BCSP). Initial evidence from the BCSP suggests that the program is set to reduce CRC-related mortality by 16%.4
A number of studies that have examined the factors that affect the uptake and acceptance of screening exist.2,5,6 Gender,7 ethnicity,8 socioeconomic status,9 and literacy levels10 have all been identified as factors. However, there has been little work examining the impact of having a long-term condition (LTC) on CRC screening uptake. Within England, better management of LTCs is a priority.11,12 About 30% of the English population have an LTC,13 and it has been estimated that 70% of all NHS spend is due to LTCs.13 Evidence about the effects of these LTCs on the uptake of CRC screening is required. Hence, the aim of this study was to examine the association between having an LTC and non-uptake of CRC screening, with a particular focus on common mental health problems such as depression and anxiety, as these are known to impact on self-management14 and so may affect the rates of uptake.
Methods
Cohorts and linkage
Two cohorts were used in this study. The first held data on uptake from the BCSP which had been linked to the regional data from the Yorkshire Health Study (YHS) to provide information on participants’ sociodemographics, LTCs, and broader health determinants. The second cohort was from the English Longitudinal Study of Ageing (ELSA). There is a growing awareness of the importance of reproducing results.15 The use of two large independent cohorts represents an ideal opportunity for prospectively validating any observed associations. The two cohorts are discussed in turn.
Linked BCSP–YHS cohort
Roll-out of the BCSP in England began in July 2006; currently eligible people aged between 60 and 74 years are offered biennial gFOBT screening.16 Screening uptake is defined as the percentage of people adequately screened out of those invited for gFOBT screening. An adequate screening occurs if the participants receive a definitive outcome of either negative (normal) or positive (abnormal) gFOBT – this result may be based on multiple gFOBT kits. Historically, uptake has been about 50% for the initial screen and about 90% for repeat screens.17 The BCSP includes information about participants’ age and gender. To obtain data on a broader range of variables, these data were linked to the YHS.
The YHS is a longitudinal observational regional health study, previously known as the South Yorkshire Cohort.18,19 All the YHS data are self-reported; a copy of the questionnaire used is available online.20 Data are available for 12 named LTCs (depression, anxiety, fatigue, pain, insomnia, diabetes, breathing problems, high blood pressure, heart disease, osteoarthritis, stroke, and cancer), along with a free-text “other” LTC. Cancer was not considered in this study as reporting of this is likely to be affected by the uptake of CRC screening. The YHS also includes evidence on participants’ demographics (age when completing questionnaire [which was converted into age at first invitation to screening], sex, and ethnicity) and broader determinants of health (deprivation, education, smoking status, alcohol consumption in the last week, and physical activity levels in the last week for walking, cycling, and physical exercise) along with data on health-related quality of life, as measured using the EQ-5D-3L,21 and health care use in the last 3 months.
Ethnicity categories were based on the 16 categories used in the 2001 UK census, along with an extra category for “Gypsy/traveler.” Deprivation was measured using the 2007 index of multiple deprivation (IMD), which is an area-based measure ranging from 0 to 80 (higher scores indicate higher levels of deprivation). The EQ-5D-3L comprises five domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). The questionnaire asks about health on the day of completing the survey, and there are three possible responses for each domain (no problems, moderate problems, and extreme problems). There were four main categories of health care use: hospital, other healthcarers, other carers, and alternative therapist, along with a free-text “other.”
Because of small numbers, ethnicity was categorized as “White” or “Non-White,” and categories of health care use were reduced from 23 to 11 (accident and emergency, hospital day case, hospital outpatients, hospital in-patients, GP, nurse, physiotherapists, other healthcarers, other carers, alternative therapists, and other health care use). In addition, three categories were derived for smoking status (never, former, and current). Further details on data cleaning are available in the Supplementary materials.
Data from the first wave of the YHS were used, covering the time period from June 2010 to September 2013 inclusive. Participants in the YHS are asked “May we use the information you provide to look at the benefit of health treatments?” and “May we look at your health records?” Those who responded “yes” to both the questions were deemed to be eligible for linkage to the BCSP data. Linkage was based on the NHS number. Data on uptake was obtained from the BCSP and were available for the calendar years 2006–2014. Participants were linked if they had ever been invited to screening, even if this was not in the year that they completed the survey; for example, a YHS participant may have completed the survey early in 2010 at the age of 55 years and been invited to screening late in 2015 (at age 60 years). Details on how age at first invitation to screening was derived are provided in the Supplementary materials. All other data were from the YHS. Data access was de-identified.
ELSA cohort
The ELSA is a nationally representative22 longitudinal survey designed to generate evidence on aging and quality of life among individuals aged ≥50 years.23 There have been seven waves of data collection, with the first wave collected in 2002/2003 and the most recent in 2014/2015. Questions regarding the uptake of CRC screening as part of the BCSP were introduced in Wave 5. The data used for this study are from Wave 7, collected in 2014/2015 and excluding proxy respondents. As part of the data collection, respondents aged between 55 and 75 years (inclusive) were asked “Have you ever completed the NHS bowl cancer screening test using the home test kit?” For those who responded yes, the date of their most recent screen was also recorded.
In addition to details on CRC screening uptake, ELSA also records information on a number of LTCs. For this study, 17 self-reported LTCs were used (Table 1). Also, evidence on participants’ demographics (age, sex, and ethnicity) and broader determinants of health (self-perceived social status, education, smoking status, alcohol consumption in the last week, relationship status, and frequency of sports or exercise) were also used. Cross-sectional weights were used to account for differences in response rates. Further details on the derivation of the variables are available in the Supplementary materials.
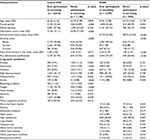  | Table 1 Key characteristics of the two samples Note: Data are n (%) unless otherwise specified. Abbreviations: ELSA, English Longitudinal Study of Ageing; YHS, Yorkshire Health Study. |
Statistical analyses
The protocol for the analysis of the linked BCSP–YHS dataset was preregistered: ClinicalTrials.gov, number NCT02503969. The analysis of ELSA data was designed to reflect the analysis of the BCSP–YHS data as closely as possible.
A descriptive analysis compared the characteristics of participants who participated in CRC screening with those who did not participate. Comparisons were tested for statistical significance, with the caveat that as no specific differences were hypothesized a priori, the resulting p-values should be interpreted with caution. Independent two-sample t-tests were used to compare continuous variables, Fisher’s exact test was used to compare binary variables, and the Kruskal–Wallis test was used to compare ordinal variables. Any p-value <5% was considered to indicate a statistically significant association. The descriptive analysis also included an assessment of the functional form of the association between continuous variables and uptake. This included both a visual assessment and the use of multivariable fractional polynomials.24
To examine the association between having an LTC and the outcome of non-uptake of CRC screening, a series of logistic regression models were constructed. The first model included only LTCs. The second model included LTCs and demographics, with the third (“full” model) including LTCs, demographics, and broader determinants of health. This was designed to highlight the unadjusted association between morbidities and screening uptake and the degree to which these associations are mediated by patient characteristics. A distinction was made between “intrinsic” demographic characteristics (age, gender, and ethnicity) and broader determinants of health. Evidence on health-related quality of life and health care use were treated as descriptive variables and hence not included in the regression models.
Variables for which the proportion of missing data was <5% were imputed using single imputation. Otherwise, multiple imputations were performed. In addition, as part of the pre-registration, power analyses were performed using G*Power 3.1.9.25 These suggested that, with a sample size of 7,500 respondents, there would be an 80% power to detect an odds ratio of ≥1.4 and a 95% power to detect an odds ratio of ≥1.5. With the exception of power analyses, all statistical analyses were performed using STATA version 14. See the Supplementary materials for further details.
Ethics and approval
ELSA data were obtained from the UK Data Service; no approvals were required. Approvals for the linked BCSP–YHS were obtained from the YHS study team, the BCSP research committee, and the Public Health England Office for Data Release. Ethical approval was obtained from the National Research Ethics Service Committee Yorkshire and The Humber – Leeds East (15/YH/0028). Linkage was restricted to participants who provided written informed consent for their data to be re-used in secondary analyses (such as this study).
Review of literature
To aid in placing the results of this study in context, a scoping search was performed to identify published papers that consider the impact of having an LTC on screening uptake, for any type of cancer. Studies were limited to those that involved organized screening and that used statistical modeling to provide an estimate of the impact of having an LTC on screening uptake, adjusted for potential confounders. In order to identify evidence, a number of bibliographic health databases were searched. Free text and thesaurus terms were combined to maximize the sensitivity of the search. Terms for cancer screening and barrier or facilitator terms were combined with terms for comorbidity or chronic disease. No date or language limits were applied to the search. Full details of search terms and sources are available in the Supplementary materials.
Results
A total of 7,330 participants had linked-YHS–BCSP data. Of these, a valid age at first invitation to screening could not be calculated for 181 (2.47%) participants and a further 7 (0.10%) did not have an IMD 2007 score. Data for these participants were dropped from subsequent analyses, resulting in an overall sample of 7,142.
There were 6,105 individuals in the ELSA cohort with valid data on screening uptake. Of those who indicated that they had received a screen, 38 were unable to provide the year of screening, and 17 reported being screened prior to 2006 (when screening began). A further 1,535 individuals were aged <61 years and hence may not have been offered screening. In addition, a further 405 individuals did not have a valid survey weight, one individual had missing ethnicity data, two had missing data on frequency of sports, and eight had missing alcohol data. These individuals were all excluded from further analyses. The resulting sample size for ELSA was 4,099.
Key descriptive data for the two samples are provided in Table 1, broken down by whether or not the individual participated in screening. Participation rates were 84.2% for the linked-YHS and 80.0% for the ELSA. Full descriptive data for the two samples are provided in the Supplementary materials. Results from both the cohorts show that compared to those who did participate in screening, those who did not participate were more likely to be male, have a higher deprivation score (or lower self-perceived social status), more likely to smoke, less likely to report drinking alcohol in the last week, less likely to report having an educational qualification, and less likely to engage in physical activities. Those who did not participate were also less likely to be in a relationship, although this was only measured in the ELSA.
The prevalence of all LTCs was also higher among those who did not participate in screening, with the exceptions of osteoarthritis and the free-text “other” for the linked-YHS, and osteoarthritis, abnormal heart rhythm, other heart disease, and rheumatoid arthritis for the ELSA. Based on the linked-YHS, those who did not participate in screening reported a lower mean EQ-5D score and were more likely to use health care services in the last 3 months, with the exceptions of alternative therapies and the free-text “other.”
Self-report data were available in both the cohorts for the prevalence of six LTCs: anxiety, depression, diabetes, high blood pressure, osteoarthritis, and stroke. The prevalence of osteoarthritis in the ELSA (29.8%) is almost twice that in the linked-YHS (15.2%), whereas the prevalence of anxiety is almost half (5.8% compared with 10.4%). The prevalence estimates for the remaining LTCs were similar in both the cohorts.
Results from the series of regression models are summarized in Table 2 (linked-YHS) and Table 3 (ELSA). Further details of the regression models are provided in the Supplementary materials. From the linked-YHS LTC-only model, an increased odds of non-participation was associated with the occurrence of stroke (odds ratio 1.72), diabetes (1.57), depression (1.43), or breathing problems (1.22), while the occurrence of osteoarthritis or a free-text “other” LTC was associated with increased odds of participation (odds ratios 0.71 and 0.79, respectively). These associations persisted after adjusting for patient demographics. After adjustment for broader determinants, these associations were no longer significant for depression and breathing problems, but they remained for the other LTCs. Other variables associated with non-participation in the full model were male gender (odds ratio 1.29), increasing levels of deprivation (1.01 per unit increase), being a current or former smoker (2.26 and 1.27, respectively, compared to a non-smoker), low levels of walking or physical exercise (odds ratios 1.43–2.10), and no alcohol consumption in the last week (1.36). Of the 17 LTCs in the ELSA, only diabetes and osteoarthritis had a significant association with screening uptake in the LTC-only model (odds ratios 1.69 and 0.79, respectively). In the full model (adjusting for patient demographics and broader determinants), the occurrence of diabetes was associated with increased odds of non-participation (1.33), while the occurrence of osteoarthritis or rheumatoid arthritis was associated with increased odds of participation (0.76 and 0.64, respectively). Other variables associated with non-participation were male gender (1.32), lower levels of self-perceived social status (1.01 per unit decrease), being a current smoker (2.43 compared to a non-smoker), low levels of mild or moderate sports or exercise (odds ratios 1.42–1.58), no alcohol consumption in the last week (1.47), and not being in a relationship (1.41 compared to those who are married).
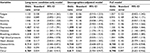  | Table 2 Results from the CRC linked-YHS cohort Notes: Data in bold are statistically significant (p<0.05). The “full model” also includes age, gender, ethnicity, educational qualifications, levels of physical activity (physical exercise, walking, and cycling), smoking status, alcohol use, and deprivation score. The “Demographics-adjusted model” also includes age, gender, and ethnicity. See the Supplementary materials for “full model” results. Abbreviations: CRC, colorectal cancer; YHS, Yorkshire Health Study. |
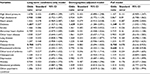  | Table 3 Results from the ELSA cohort Notes: Data in bold are statistically significant (p<0.05). The “full model” also includes age, gender, ethnicity, self-perceived social status, relationship status, smoking status, alcohol use, educational qualifications, and frequency of sports or exercise (vigorous, moderate, or mild). The “Demographics-adjusted model” also includes age, gender, and ethnicity. See the Supplementary materials for “full model” results. Abbreviation: ELSA, English Longitudinal Study of Ageing. |
The literature review identified 14 studies that assessed the impact of having an LTC on the uptake of CRC screening. Of these studies, nine used a count of comorbidities and seven examined specific LTCs (two studies used both the approaches within the same analysis). Seven studies considered the impact of LTCs on the uptake of CRC screening. Five studies used a count of comorbidities; three of these found that individuals with a higher comorbidity count had a higher uptake of CRC screening, while two studies did not find any effect. Two studies examined specific LTCs. In these studies, having an LTC could result in increased or decreased CRC uptake or have no effect at all depending on the condition. Similar results were also observed for the other non-CRC screening tests considered, which suggests that using a simple count of comorbidities may mask the role of individual conditions in increasing or decreasing uptake. Further results, including for the other types of screening identified, are available in the Supplementary materials.
Discussion
Results from both the cohorts were consistent in showing increased uptake of CRC screening among individuals with osteoarthritis and decreased uptake among individuals with diabetes. The common mental health problems of anxiety and depression were self-reported in both the cohorts. In the linked-YHS, individuals with depression (but not anxiety) had lower uptake, after controlling for demographic factors. However, this association disappeared in the full model after controlling for broader determinants of health. In the ELSA, there was no statistically significant association for any of the models considered. Hence, there is some evidence to suggest that individuals with depression have reduced levels of CRC screening uptake and also that this may be due to patterns of broader health determinants among these individuals. Self-reported “emotional problems” and “other psychiatric conditions” were also available in the ELSA. There was no evidence of any statistically significant association with the uptake of CRC screening. However, the prevalence of these conditions was low among the sample (2.1% and 3.1%, respectively). Hence, the lack of an association may have been due to a lack of power, rather than an absence of any effect. Indeed, the odds ratio for emotional problems in the full model (1.41) was greater than that for diabetes (1.35). Of the remaining LTCs, the occurrence of a stroke was associated with lower uptake in the full linked-YHS model (odds ratio 1.59), but not in any of the ELSA models (odds ratio 1.01 in the full model). The reason for these discrepant findings is unclear. The free-text “other” LTC recorded in the linked-YHS was associated with higher uptake, although it is difficult to draw conclusions about this association. In the full ELSA model, individuals with rheumatoid arthritis had higher observed uptake rates. This was not a named LTC in the linked-YHS. It is notable that two types of arthritis (osteoarthritis and rheumatoid arthritis) were associated with increased uptake, although no association was observed for the LTC “other kind of arthritis.”
To the authors’ knowledge, this is the first UK-based study – and the largest study internationally – to assess the association between named LTCs and the uptake of population-based CRC screening. These associations were examined in two independent cohorts, which improved both the external validity of the results and the robustness of the findings. Both the cohorts comprised information on a rich variety of potential confounders, which further strengthens the findings presented.
The results of this study have also shown that most of the existing research considers a simple count of comorbidities and that the presence of an LTC can be associated with either increased or decreased uptake. Hence, use of a simple count may lead to misleading results.
This study created a novel linkage between the NHS BCSP and the YHS. This has a number of strengths; it allowed for analysis of a relatively large sample size, it used an objective definition of CRC uptake (instead of relying on respondents’ self-reported uptake), and it demonstrates the potential for linkage to enhance the possibilities for secondary analysis of health care data sets in order to help improve clinical decision-making. A particular strength of the ELSA cohort is that it is a nationally representative sample of those aged ≥50 years.
There are some limitations in the work. Rates of screening participation were over 80% for both the cohorts. This is higher than that has been previously reported.17 This may be because this study considered participation across any round of screening, as opposed to participation with a single round. For both the cohorts, the LTCs were self-reported, and so may not be as clinically relevant as a doctor-diagnosed LTC. In addition, data were not prospectively collected for this study. This is particularly problematical for age, as it was not possible to derive a precise age at screening. The results presented suggest that those at the start or end of the screening age-range are less likely to have received an adequate screen. This may be an artefact of the screening process if they have received less invitations (screening does not commence until the age of 60 years and the extension of the upper age limit from 70 to 74 years was only fully rolled out in 2015). The lack of an objective measure of uptake is a further limitation with the ELSA data. However, self-report data on FOBT uptake have been shown to have sensitivity and specificity.26 As with any self-reported data, it is important to consider the representativeness of the respondents. The ELSA has been shown to be nationally representative, while the YHS has been shown to slightly overrepresent older White females from areas of low deprivation.19 There are also differences between the two cohorts used. The ELSA relies on self-report for screening uptake (average uptake 80%) while the linked-YHS used data recorded by the NHS BCSP (average uptake 84%). Compared to the ELSA, individuals in the linked-YHS were on average 4 years younger, more likely to be male, had lower reported qualifications, and were more likely to report drinking alcohol in the last week. There were also differences in the prevalence of some LTCs, as previously noted. However, despite this, a number of consistent themes emerged.
Based on the results of the literature review, it has been found that no previous studies have examined the association between CRC screening uptake and having osteoarthritis, while the association with diabetes has only been assessed in one study of 2,225 individuals (prevalence of diabetes 24%),27 which did not find an association (odds ratio for receiving screening 0.90, 95% CI 0.73–1.12). Other variables were considered in both this and the previous study: depression, stoke, and lung disease. None of these variables had a significant association, which supports the findings of this study (with the one exception of stroke in the linked-YHS cohort, which is associated with decreased uptake). The study did find that individuals with hypertension were more likely to receive screening (odds ratio 1.37, 95% CI 1.12–1.66). In contrast, there was no association with high blood pressure in either of the cohorts analyzed in this study. However, it is unclear if the results from this study are generalizable to an English setting, as it was conducted in 1992 among older individuals (mean age 79 years) based in North Carolina.
The findings of this research are important to decision-makers as they suggest that there are potential inequalities in uptake based on the presence of certain LTCs. In particular, higher uptake is observed among individuals with osteoarthritis, and lower uptake among individuals with diabetes. The reasons for these associations are unclear. However, the two data sets comprise evidence on a rich array of factors that may influence uptake, such as sociodemographics and lifestyle factors. Hence, the observed differences in uptake are unlikely to be due to differences in patient-mix. Further research could explore and compare the barriers and facilitators to screening uptake experienced by individuals with diabetes or osteoarthritis. Such work would provide opportunities for shared learning and may help to reduce the potential inequalities in uptake. The results of this study also provide evidence that there are no inequalities in uptake for individuals with self-reported anxiety. For individuals with depression, any differences in uptake may be explained by differences in patterns of broader determinants of health. Further work to detangle the causal effects of these would be useful.
Conclusion
Two large independent cohorts both provided evidence that individuals with diabetes have lower uptake of CRC screening while individuals with osteoarthritis have higher uptake. There was little evidence to suggest that individuals with common mental health problems had different rates of uptake compared to the general population. Our study results have the potential to improve clinical decision-making by providing unique evidence on patient groups who are likely to require further interventions to improve screening uptake or who can provide useful evidence about the facilitators to high levels of uptake.
Data sharing statement
The ELSA data are available from the UK Data Service.
Acknowledgments
We are grateful to all the individuals who have enrolled in the YHS. We also acknowledge the GP practice staff for their contribution in the recruiting process. This publication is the work of the authors and does not necessarily reflect the views of the YHS Management Team or Steering Committee. This paper presents independent research by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for South Yorkshire (NIHR CLAHRC SY) a pilot study which ended in 2013. Further details about the new NIHR CLAHRC Yorkshire and Humber can be found at www.clahrc-yh.nihr.ac.uk. The views and opinions expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
We would like to thank Julietta Patnick for helping with the design of the study, and the NHS BCSP for providing data on screening uptake. We would also like to thank the BCSP, the National Research Ethics Service Committee Yorkshire and The Humber – Leeds East, and Public Health England for providing useful feedback on the protocol of this work. The views expressed in this publication are those of the authors and not necessarily those of the individuals or organizations named above.
ELSA was developed by a team of researchers based at the NatCen Social Research, University College London and the Institute for Fiscal Studies. The data were collected by NatCen Social Research. The funding is provided by the National Institute of Aging in the United States, and a consortium of UK government departments coordinated by the Office for National Statistics. The developers and funders of ELSA and the Archive do not bear any responsibility for the analyses or interpretations presented here.
The abstract for this paper was presented at the 16th Biennial European Conference of the Society for Medical Decision Making, June 12–14, 2016 and at the Health Services Research UK Symposium July 6–7, 2017.
This study presents independent research funded by Public Health England. The views expressed are those of the authors and not necessarily those of Public Health England. The funder of this study had no role in the study design, data collection, data analysis, data interpretation, writing of the report or the decision to submit. The researchers worked independently from the funder.
Author contributions
BK, JC, SW, CR, and AL conceived the study design. BK, CN, and AL were responsible for data linkage. HBW performed the literature searches. BK performed the statistical analysis and wrote the first draft of the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All authors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and registered) have been explained.
Disclosure
The authors report no conflicts of interest in this work.
References
Cunningham D, Atkin WS, Lenz HJ, Minsky B, Nordlinger B, Starling N. Colorectal cancer. Lancet. 2010;375(9719):1030–1047. | ||
Honein-AbouHaidar GN, Kastner M, Vuong V, et al. Benefits and barriers to participation in colorectal cancer screening: a protocol for a systematic review and synthesis of qualitative studies. BMJ Open. 2014;4(2):e004508. | ||
National Cancer Intelligence Network. Colorectal cancer survival by stage. 2013. Available from: http://www.ncin.org.uk/publications/data_briefings/colorectal_cancer_survival_by_stage. Accessed May 8, 2017. | ||
Logan RF, Patnick J, Nickerson C, Coleman L, Rutter MD, von Wagner C. Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first 1 million tests. Gut. 2012;61(10):1439–1446. | ||
Weller DP, Campbell C. Uptake in cancer screening programmes: a priority in cancer control. Br J Cancer. 2009;101:S55–S59. | ||
Beydoun HA, Beydoun MA. Predictors of colorectal cancer screening behaviors among average-risk older adults in the United States. Cancer Causes Control. 2008;19(4):339–359. | ||
Pornet C, Dejardin O, Morlais F, Bouvier VÃ, Launoy G. Socioeconomic determinants for compliance to colorectal cancer screening. A multilevel analysis. J Epidemiol Commun Health. 2010;64(4):318–324. | ||
Robb KA, Power E, Atkin W, Wardle J. Ethnic differences in participation in flexible sigmoidoscopy screening in the UK. J Med Screen. 2008;15(3):130–136. | ||
Von Wagner C, Good A, Wright D, et al. Inequalities in colorectal cancer screening participation in the first round of the national screening programme in England. Br J Cancer. 2009;101:S60–S63. | ||
von Wagner C, Semmler C, Good A, Wardle J. Health literacy and self-efficacy for participating in colorectal cancer screening: the role of information processing. Patient Educ Couns. 2009;75(3):352–357. | ||
Goodwin N, Curry N, Naylor C, Ross S, Duldig W. Managing people with long-term conditions. An inquiry into the quality of general practice in England London, The King’s Fund; 2010. Available from: https://www.kingsfund.org.uk/sites/default/files/field/field_document/managing-people-long-term-conditions-gp-inquiry-research-paper-mar11.pdf. Accessed February 12, 2018. | ||
Department of Health. Raising the Profile of Long Term Conditions Care: A Compendium of Information. 2008. London, DoH. Available from: https://goo.gl/A3BLNu. Accessed May 8, 2017. | ||
Department of Health. Improving the Health and Well-being of People with Long Term Conditions. 2010. London, Department of Health. Available from: https://goo.gl/Eamt58. Accessed May 8, 2017. | ||
Das-Munshi J, Stewart R, Ismail K, Bebbington PE, Jenkins R, Prince MJ. Diabetes, common mental disorders, and disability: findings from the UK National Psychiatric Morbidity Survey. Psychosom Med. 2007;69(6):543–550. | ||
Begley CG, Ioannidis JP. Reproducibility in science. Circ Res. 2015;116(1):116–126. | ||
Kearns B, Whyte S, Seaman HE, et al. Factors associated with completion of bowel cancer screening and the potential effects of simplifying the screening test algorithm. Br J Cancer. 2016;114(3):327–333. | ||
Kearns B, Whyte S, Chilcott J, Patnick J. Guaiac faecal occult blood test performance at initial and repeat screens in the English Bowel Cancer Screening Programme. Br J Cancer. 2014;111(9):1734–1741. | ||
Kearns B, Ara R, Young T, Relton C. Association between body mass index and health-related quality of life, and the impact of self-reported long-term conditions: cross-sectional study from the south Yorkshire cohort dataset. BMC Public Health. 2013;13(1):1. | ||
Green MA, Li J, Relton C, et al. Cohort profile: the Yorkshire health study. Int J Epidemiol. 2016;45(3):707–712. | ||
Relton C, Bissell P, Smith C, et al. South Yorkshire Cohort: a “cohort trials facility” study of health and weight – protocol for the recruitment phase. BMC Public Health. 2011;11(1):1. | ||
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–1108. | ||
Steptoe A, Breeze E, Banks J, Nazroo J. Cohort profile: the English longitudinal study of ageing. Int J Epidemiol. 2013;42(6):1640–1648. | ||
Marmot M, Oldfield Z, Clemens S, et al. English Longitudinal Study of Ageing: Waves 0-7, 1998-2015, [data collection], 26th edition, UK Data Service; November 30, 2016. Available from: http://dx.doi.org/10.5255/UKDA-SN-5050-13. Accessed February 12, 2018. | ||
Royston P, Sauerbrei W. Multivariable Model-Building: A Pragmatic Approach to Regression Analysis Based on Fractional Polynomials for Modelling Continuous Variables. Chichester, England: John Wiley & Sons; 2008. | ||
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. | ||
Vernon SW, Tiro JA, Vojvodic RW, et al. Reliability and validity of a questionnaire to measure colorectal cancer screening behaviors: does mode of survey administration matter? Cancer Epidemiol Biomarkers Prev. 2008;17(4):758. | ||
Heflin MT, Oddone EZ, Pieper CF, Burchett BM, Cohen HJ. The effect of comorbid illness on receipt of cancer screening by older people. J Am Geriatr Soc. 2002;50(10):1651–1658. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
