Back to Journals » Risk Management and Healthcare Policy » Volume 14
The Association Between Cognitive Medical Errors and Their Contributing Organizational and Individual Factors
Authors Alyahya MS , Hijazi HH, Alolayyan MN , Ajayneh FJ, Khader YS , Al-Sheyab NA
Received 20 November 2020
Accepted for publication 18 January 2021
Published 3 February 2021 Volume 2021:14 Pages 415—430
DOI https://doi.org/10.2147/RMHP.S293110
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Mohammad S Alyahya,1 Heba H Hijazi,1 Main Naser Alolayyan,1 Farah Jehad Ajayneh,1 Yousef S Khader,2 Nihaya A Al-Sheyab3
1Department of Health Management and Policy, Faculty of Medicine, Jordan University of Science and Technology, Irbid, 22110, Jordan; 2Department of Public Health and Community Medicine, Faculty of Medicine, Jordan University of Science & Technology, Irbid, 22110, Jordan; 3Allied Medical Sciences Department, Faculty of Applied Medical Sciences, Department of Maternal and Child Health Nursing, Faculty of Nursing, Jordan University of Science and Technology, Irbid, 22110, Jordan
Correspondence: Mohammad S Alyahya
Department of Health Management and Policy, Faculty of Medicine, Jordan University of Science and Technology, P.O. Box: 3030, Irbid, 22110, Jordan
Tel +962 2-7201000 Ext: 23690
Email [email protected]
Background: Examining cognitive medical errors (MEs) and their contributing factors is vital in health systems research, as it provides baseline data that can be used to develop appropriate interventions to prevent and/or minimize errors. The primary aim of this study was to investigate the association between cognitive MEs and hospitals’ organizational factors and the individual psychological and functional factors.
Methods: This cross-sectional study was conducted in three main hospitals in Northern Jordan. A proportional sampling technique was employed to decide the number of participants from each hospital. Data from physicians and nurses (n=400) were collected using a self-administered questionnaire, which was developed based on pertinent literature review. Exploratory and confirmatory factor analyses were conducted to validate the study instrument. The relationships between the variables were analyzed through structural equation modeling (SEM) using AMOS. Multi-group analysis was also performed to examine the differences in the participants’ perceptions towards the respective variables between the three selected hospitals.
Results: Our results showed a non-significant negative association between MEs and hospital organizational factors. Also, the SEM analysis showed a positive significant correlation between MEs and psychological and functional factors, whereby excessive workload, complexity of tasks, stress, sleep deprivation, and fatigue were found to be predictors of MEs occurrence. In comparison to the results from the university hospital, the multi-group analysis results from the governmental public hospital and the private hospital showed a significant impact of psychological and functional factors on MEs.
Conclusion: To reduce the occurrence of MEs in hospitals, there is a need to enhance organizational safety culture. Efforts should be directed at both organizational and individual levels. Also, it is essential that health decision makers develop strategies to reduce work-related stress and improve healthcare staff well-being, as work stress may cause cognitive impairments among healthcare workers and hence threaten patients’ safety.
Keywords: organizational culture, policies and procedures, mistakes, slips and lapses, workload, stress, fatigue
Introduction
Although attention is being increasingly paid to ensuring patient safety and healthcare quality, medical errors (MEs) and adverse events are still frequent in healthcare providers’ practice and pose a major threat to patients’ safety. MEs are one of the most significant public health problems around the world and are considered one of the major challenges that healthcare systems face in all countries.1,2 Globally, it was estimated that 142,000 people died in 2013 due to adverse effects of clinical treatment, which was a significant increase from 94,000 deaths in 1990.3 However, it was reported that the number of deaths due to MEs in the United States (US) alone in 2013 was 251,454 deaths, suggesting that the global estimation in 2013 may not have been completely accurate. MEs are now the third leading cause of death in the US.4 Similarly, in 2015, a study conducted in England estimated that about 3.6% of the hospital deaths were due to problems in care,5 with the rates of adverse events in hospitals reaching up to 7.5% and 11.7% in Canada and Britain, respectively.6,7
In Jordan, no studies have investigated MEs in general, though some studies have investigated medication errors in particular.8–12 In a study conducted in Jordan, the rate of medication errors using incident reports was 42%.13 Another study reported a medication error rate of 35% (ie 36.4% in ICUs and 33.8% in wards).10 Recently, Alrabadi et al (2020) conducted a study among nurses in three major teaching hospitals in Jordan and found that MEs were underreported, with the reporting rate identified as 28%.14 Similarly, a meta-analysis was conducted to estimate a 1-year prevalence and reporting rate of medication errors among nurses working in Iranian hospitals; the results showed that the overall prevalence of medication errors and their reporting rate were 53% and 36%, respectively.15 Many cases of MEs cannot be estimated because medical records are often underreported, inaccurate, or incomplete.14,16,17 Thus, revealing causes and contributing factors of MEs can inform health policies and practices to reduce their risks and consequences.
Classification or taxonomy of MEs is an important first step and key requirement for the deep understanding of the nature, origins, and causes of human error and the improvement of patient care.18 In their extensive report “To err is human: building a safer health system”, the Institute of Medicine (IOM) classified MEs into diagnostic errors, treatment errors, preventive errors, and other errors (such as failure of communication and equipment failure).19 However, psychological classification (cognitive) of MEs explains events rather than merely describing them, thus, provides a better understanding about the error and its context to be able to prevent similar errors within the same institution. Cognitive MEs are classified into (1) mistakes, (2) slips, and (3) lapses.20,21
Mistakes refer to the correct implementation of an incorrect action sequence. This means that actions may go entirely as planned, but the plan itself deviates from some adequate way towards its intended outcome.20,22 Here, the error lies in the mental processes involved in planning, formulating intentions, judging, and problem-solving (planning of an action).22 This type of error arises when the healthcare providers have incorrect or absent knowledge about the task they are aiming to complete, whereby they may believe that they are doing the right thing, but in fact be doing the wrong thing.23 Slips and lapses are execution failures at the skill-based behavior level. Slips can be defined as an action that was not implemented or performed based on a plan. Such errors occur when the intention is correct, but a failure occurs during the implementation of the task or the action.20,24 Slips occur when a person has the knowledge needed to perform a task, which means the understanding of a situation and the intention are both correct but for some reason, the execution of actions does not go as intended.23,25 Thus, the person uses wrong automatic action to achieve a goal, thereby obtaining the wrong outcome. Lapses are usually failure related to memory functions, which also leads to incomplete or unsuccessful planned task or action. It is an unintended action that might be an omission or commission or an action that did not meet its intended results.26,27 Here, the failure occurs at the internal level and is related to failure of memory. Slips and lapses can occur by highly skilled professionals when carrying out simple tasks that they usually perform without errors. Therefore, predicting such errors may be difficult due to their inherent nature. On the other hand, a mistake may occur by healthcare professionals whose intentions and understanding of situations are not correct. Therefore, mistakes are more detectable and manageable than slips or lapses. Hence, healthcare organizations need to focus on both organizational and individual factors that might cause or lead to MEs.
MEs and Organizational Culture, Policies, and Procedures
In healthcare systems, organizational culture is the primary driver of safety, and the type of culture affects, directly or indirectly, the safety of patients.28–30 Moreover, organizational culture has the potential to shape healthcare providers’ attitudes, direct their behaviors, and encourage or prevent them from speaking up about MEs, depending on the perceived value of safety culture within the organization.31,32 There are two types of organizational culture that influence patient safety and quality improvement: safety culture and blame culture. Positive safety culture plays an important role in guiding healthcare systems to minimize patient harm.17,33–35 Within this culture, MEs are openly discussed, as there is freedom in sharing and reporting MEs.27,32,36 Safety culture provides quick and comprehensive investigations of patient safety incidents and creates an environment that promotes trust in the organization and treats MEs as a learning opportunity rather than a chance to punish or blame.32,34,37–39
In contrast, blame culture is a construct of behavioral norms and attitudes characterized by the inability and unwillingness to take risks or responsibility for errors because of a fear of negative consequences, such as being blamed or punished.40 Changing healthcare providers’ blame culture-related beliefs and attitudes could help in minimizing mistakes and related consequences, ultimately improving patients’ safety.28,40,41
Previous studies have indicated that more than 45% of MEs go unreported because healthcare providers are afraid of negative outcomes and doubt their employer’s ability to be constructive and provide support.42–44 In Jordan, fear of punishment has been reported as being one of the leading causes of the underreporting of errors among nurses, with a 21% rate of non-punitive responses to errors highlighting the presence of a blame and shame culture.45,46 Healthcare systems need to recognize the importance of changing their organizational culture into a safety culture. This transformation can be achieved by promoting trust among healthcare providers, encouraging cooperation among employees, and enhancing awareness regarding the importance of reporting and sharing any information about MEs.17,39,47 In summary, blame culture perceives errors as personal failures, and this may be a barrier for healthcare providers in reporting MEs. Meanwhile, safety culture perceives errors as learning opportunities, whereby healthcare providers can report, share, and discuss MEs without fear of punishment or blame and the same errors can therefore be prevented from occurring in the future.
Policies and procedures also play an essential role in healthcare organizations and represent a cornerstone in the process of making medical decisions. Policies and procedures help healthcare providers understand their roles and responsibilities within the organization and provide standardized practices and activities. Procedures provide instructions and guidance for healthcare providers about appropriate care, hence reducing practice variations and ensuring safe practice. Therefore, complying with policies and procedures is essential for ensuring patient safety and reducing the occurrence of MEs, and hospitals have a duty to inform and communicate with all healthcare providers before developing a new policy or revising an existing one.48,49
Psychological and Functional Factors: Workload and Complexity of Tasks, Stress, and Sleep and Fatigue
The relationship between healthcare providers’ workload and MEs is considered one of the most persistent themes in the field of healthcare, given that the healthcare environment is characterized by uncontrolled and unpredictable workloads. However, workload is a hypothetical construct that represents the effort exerted to achieve a particular level of performance and is an outcome of interrelated factors including the requirements of a task, the conditions under which the task is executed, and the skills and perceptions of workers.50,51 Hence, shift work and long working hours have negative consequences on the health and well-being of healthcareproviders in general and nursing staff in particular, which may negatively impact patient outcomes.52–54 Multitasking may also negatively affect healthcare providers’ memory and attention, as well as potentially distorting their perception of the correct goal of a given task due to its similarity to another task. When healthcare providers do multiple tasks concurrently or sequentially, they may mix up or lose sight of the goals for the different tasks because the goals are too many to be kept in working memory. Consequently, this may adversely impact patient safety and increase the occurrence of MEs.20,55,56 Evidence has shown that fatigue has several negative effects on healthcare providers, which may include degraded performance, overloaded memory, impaired cognitive processes, irritability, lack of learning, and a lack of focus on performing tasks correctly. Also, fatigued providers are more likely to select unsafe alternative behaviors, such as taking shortcuts when performing tasks.57 Similarly, sleep deprivation hinders the provision of high-quality and safe patient care.58,59 It has been found that shift work and extended working hours have adverse impacts on nurses’ sleep patterns.60 Recently, Stimpfel et al (2020) found that nursing staff are sleeping less than the recommended hours before attending work, which may affect their job performance and heath.59 However, due to the nature of healthcare environments, healthcare providers may work despite them being fatigued and sleep-deprived, which may compromise the quality of their provided healthcare and lead them to make more MEs. Stress is a response to an unexpected stressor or fatigue, and globally, work-related stress is considered a risk factor for workers’ health and safety, as it directly influences individuals’ thought processes and shortens their attention spans during task performance.61,62 Workplace stress usually arises when there is a conflict between the job demands and the amount of control an individual has over meeting these demands.63
Despite this intuitive link between cognitive MEs and psychological and functional factors, limited research has been conducted in this area, particularly in low- or middle-income healthcare systems. Moreover, to the best of our knowledge, this is the first study that combines hospitals' organizational factors and psychological and cognitive factors with MEs. Thus, the current study aimed to investigate the association of cognitive MEs with hospitals’ organizational factors and workload, stress, and sleep and fatigue.
Methods
Study Design and Setting
A correlational cross-sectional study design was used in the current study to investigate the relationship between cognitive MEs (mistakes, slips, and lapses) and their contributing factors in Jordan. A self-reported questionnaire was used for data collection, and the study was conducted in three main hospitals in Northern Jordan. The inclusion criteria for selecting these hospitals were: (1) representing different health sectors (including university, public, and private sectors), (2) providing general health services, and (3) being main and large hospitals. The target population of the study was all registered nurses and physicians who were working in the clinical departments of the three selected hospitals. As the number of healthcare staff vary in participating hospitals, a proportional sampling technique was used to recruit participants based on hospital type and size. Based on a 95% confidence interval and margin error of 5%, it was determined that a total of 414 nurses and physicians from the three hospitals were required. The convenience sampling method was used to recruit 441 healthcare providers; however, we managed to recruit only 400 healthcare providers (284 nurses and 76 physicians (residents and specialists) and 40 heads of department.
Survey Instrument
The researchers of this study were unable to find any published validated tool for measuring the association of MEs with workload and hospitals’ organizational culture and therefore developed their own survey based on previous relevant literature and experts’ opinions. The questionnaire, which was developed in English comprised four main sections: demographic data, information about MEs, hospital organizational factors, and psychological and functional factors. In detail, the first section of the questionnaire included questions about the demographic characteristics of the healthcare providers, including gender, age, profession, education, years of experience working in a hospital, and total years of experience. The second section included questions about MEs (mistakes, slips, and lapses), and the third section included questions about hospital organizational culture, policies, and procedures. Finally, the fourth section comprised psychological and functional questions about workload and the complexity of tasks, stress, and sleep and fatigue. All items were scored on a 5-point Likert scale.
Data Collection
Prior to data collection, a pilot study was conducted on 50 nurses and physicians to evaluate their understanding of the questionnaire. In general, the feedback from the participants was excellent, and they indicated that this topic had not previously been studied in Jordan. The internal consistency of the questionnaire was tested using Cronbach’s alpha, and values ranged from 0.602 to 0.900 (Table 1). The content validity of the questionnaire was assessed by three experts in quality and patient safety, and according to the experts’ comments, some items were altered and some domains modified. Before distributing the questionnaire, the researchers obtained permission from the heads of the department at the selected hospitals. Data collection took place during different times of the day (day, evening, and night) to ensure that the sample was representative and that participants working different shifts were included. The required completion time for the questionnaire was approximately 20 minutes. Data were collected between July and October 2020.
 |
Table 1 Results of the Pilot Study (N=50) |
Data Analysis
The current study used exploratory factor analysis (EFA), which is a statistical technique used to detect the underlying components or groupings of items measuring the particular construct and to discover the structure of factors through the factor loading of every measurement.64,65 EFA was carried out to assess the usefulness of each item through factor loading and the dimensionality of the items through the components. Cronbach’s alpha was used to measure the internal reliability. In addition, confirmatory factor analysis (CFA) was employed to determine the reliability and different types of validity of the latent constructs, which is required for performing structural equation modeling (SEM).
The purpose of CFA is also to assess and validate the measurement model. The relationships between the variables were analyzed through SEM using AMOS, which is used to explain the relationships between independent and dependent variables. This approach includes using factor analysis, structural models, and path analysis. The proposed conceptual framework included several relationships between the study constructs. Therefore, AMOS was used, as it allows for the evaluation of the whole study model by conforming to different connected dependence relationships, which gives a greater-level standpoint of analysis. Multi-group analysis was also used in the current study to examine the differences in the participants’ perceptions towards the respective variables between the three selected hospitals.66
Ethical Considerations
Ethical approval was obtained from the Institutional Review Board (IRB) committee at Jordan University of Science and Technology, the Jordanian Ministry of Health (MOH), and the administrators of the selected hospitals. Permission to distribute the questionnaire was obtained from the heads of department at the three selected hospitals. Prior to data collection, informed consent was obtained from the participants, who were made fully aware of the study significance and purposes.
Results
Demographic Characteristics
Table 2 shows the demographic profile of the respondents (N=400). Almost half of the participants (52.5%) were female, and 49% of the participants were aged 31–40 years. As with regards to profession, 71.0% of the respondents were nurses and 19.1% were physicians. The majority of the respondents were undergraduate degree holders (70.8%), while 13.3% held postgraduate degrees. Around one-third of the participants (30.5%) had between 6 and 10 years of work experience in the healthcare sector.
 |
Table 2 Demographic Profile of the Respondents |
Exploratory Factor Analysis and Cronbach’s Alpha
Factor analysis was conducted for all of the three main variables, namely MEs (ME), hospitals’ organizational factors, and psychological and functional factors. Hospitals’ organizational factors had the two sub-variables organizational culture (blame or safety culture) and policies and procedures, while psychological and functional factors had the three sub-variables complexity of tasks, stress, and sleep and fatigue. Varimax and principal component analysis (PCA) using the Statistical Package for the Social Sciences (SPSS) version 21 were used for all indicators or items for each of these variables.
Table 3 presents the results of the factor loadings analysis of all variables. The Kaiser–Meyer–Olkin (KMO) values for all of the variables were within the acceptable range.67 Since the KMO values for all the variables met the recommended value of 0.668 and Bartlett’s Test of Sphericity was statistically significant (p<0.01), the data were deemed appropriate for factor analysis. In the factor analysis, only items that achieved a factor loading value of 0.50 or above were retained and included in further analysis, while factor loadings of below 0.50 were excluded from further analysis.
 |
Table 3 Exploratory Factor Analysis and Cronbach’s Alpha |
A cutoff value of 0.7 for internal reliability is recommended.69 However, due to the nature of the study instrument, the internal reliability values for the blame culture and stress factors in the current study are considered acceptable despite them being lower than 0.70. Most factors in the current study showed good reliability, which enabled further analysis.
Measurement Model Assessment
In order to validate the study constructs, CFA was initially conducted for each construct to complete checking for convergent and discriminant validation for each scale. Fitness indices also needed to be checked to assess construct validity. Furthermore, average variance extracted (AVE), which is usually used to assess convergent validity, was used in the present study. Composite reliability (CR) is considered the most suitable measure for assessing construct reliability.70 Three fit indices, namely parsimonious fit, incremental fit, and absolute fit, were used to measure the standard values and validity of the constructs. The fitness indices and their greater thresholds are presented in Table 4. Only one fitness index from each group is needed.
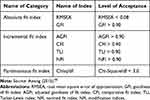 |
Table 4 Categories of Model Fit and Their Cutoff Values |
CFA of the Hospital Organizational Factors Construct
This study aimed to address its main research questions and objectives by analyzing the respondents’ perceptions towards MEs and their contributing factors, which would help the researchers draw up a conceptual model that could then be refined through future research. The first exogenous construct, namely hospital organizational factors, is a second-order construct with three sub-constructs (ie blame culture, safety culture and policies and procedures) measured by various respective items.
In the present study, the first run of the model showed poor results with unacceptable convergent validity measurements and poor factor loading. After screening the model, it was decided to merge the two dimensions (safety culture and blame culture) into one dimension, namely organizational culture. To improve the model, it was also decided to delete the items related to blame culture in the organizational culture dimension, after which fit results were obtained. For the absolute fit category, the root-mean-square error of approximation (RMSEA) value was 0.045, which was below the limit of 0.08. For the incremental fit category, the comparative fit index (CFI) value was 0.97, which was above the threshold of 0.90. As for the parsimonious fit category, the Chisq/df ratio value was 1.814, which was below the limit of 3.0.71 Therefore, the measurement model of the hospital organizational factors construct met the construct validity requirements.
As with regards to assessing convergent validity, it was necessary to calculate two important values, namely average variance extracted (AVE) and composite reliability (CR). A construct is considered to have convergent validity if the AVE and CR values exceed the minimum values of 0.5 and 0.6, respectively.72 The AVE and CR values for the hospital organizational factors construct and its associated sub-constructs were calculated using Microsoft Excel simple equations and are provided in Table 5.
 |
Table 5 AVE and CR Values for the Hospital Organizational Factors Construct |
CFA of the Psychological and Functional Construct
The second exogenous construct, the psychological and functional construct, is a second-order construct with three sub-constructs (ie workload and complexity of task, stress, and sleep and fatigue) measured by various respective items. Initially, the first run of the model showed unacceptable convergent validity measurements with poor factor loading. After screening the model, it was decided to delete the items of Stress 1 and Stress 2, and the results obtained were fit. The RMSEA value was 0.079, which was below the limit of 0.08, and the CFI value 0.94, which was above the threshold of 0.90. However, the Chisq/df ratio value was 3.466, which was above the limit of 3.0. However, one index does not affect the whole model if the other indices are good.71 Therefore, the measurement model for the workload construct met the construct validity requirements. As with regards to assessing convergent validity, it was necessary to calculate the AVE and CR values for the construct. The AVE and CR values for the psychological and functional construct and its associated sub-constructs were calculated using Microsoft Excel simple equations and are provided in Table 6.
 |
Table 6 AVE and CR Values for the Psychological and Functional Construct |
CFA of the MEs Construct
The third construct, MEs, is a second-order endogenous construct with three sub-constructs (mistakes, slips, and lapses) measured by various respective items. The RMSEA value for this construct was 0.152, which was above the limit of 0.080. However, based on the categories provided in Table 7, only one index from each category is required for evaluating the model fitness. Therefore, we adopted the goodness fit index (GFI), as an acceptable value of 0.98 was obtained. The CFI value was 0.95, which was above the threshold of 0.90; however, the Chisq/df ratio value was 10.213, which was above the limit of 3.0.71 Therefore, the measurement model for the MEs construct met most of the requirements of construct validity. The AVE and CR values were calculated in order to assess convergent validity. The AVE and CR values for the MEs construct and its associated sub-constructs were calculated using Microsoft Excel simple equations and are provided in Table 7.
 |
Table 7 AVE and CR Values for the MEs Construct |
Structural Equation Modeling (SEM) Analysis
Structural equation modeling (SEM) was used to analyze the relationships between the respective variables and answer the study questions. The current study aimed to examine cognitive MEs and identify the contributing factors that need to be considered in order to reduce the occurrence of MEs. Few studies in the literature have explored the cognitive classification of MEs, and no such study has been carried out in Jordan. A structural model was developed to answer the proposed questions. The results of the SEM text output are presented in Table 8. The computed probability value (P-value) obtained from the maximum likelihood estimators (MLE) procedure was 0.326, thus indicating that the effect of the exogenous construct hospitals’ organizational factors on the endogenous construct MEs was insignificant (P>0.05). Thus, the suggested correlation was not empirically confirmed. However, the path coefficient showed a negative association between the respective constructs and indicated that improving hospitals’ organizational factors would reduce the occurrence of MEs.
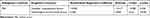 |
Table 8 The Standardized Regression Weights and Its Significance for Each Path |
The obtained probability value indicated that the effect of the exogenous construct psychological and functional on the endogenous construct MEs was also insignificant. Therefore, it can be concluded that psychological and functional factors have a positive significant association with MEs. Also, the path coefficient showed a positive effect, which indicates a positive association between the respective constructs and suggests that increasing workload task complexity, stress, and sleep and fatigue lead to an increase in MEs. Based on the obtained results, the suggested conceptual model can be finalized as shown in Figure 1, which summarizes the factors that may contribute to the occurrence of MEs in the selected hospitals and the dimensions of each factor.
 |
Figure 1 Suggested conceptual model of ME factors. |
Multi-Group Analysis
Multi-group analysis (MGA) was conducted using AMOS to examine the differences, if any, in the participants’ perceptions towards the respective variables. The dataset was divided into three different independent subsets to show the agreement among the participants. Table 9 shows that, in comparison with respondents from the other hospitals, the respondents from the university hospital did not perceive MEs to be impacted by the organizational characteristics’ factor and its dimensions or the psychological and functional factors and their dimensions. Meanwhile, the results from the governmental public hospital and the private hospital showed that the participants perceived workload to have a significant impact on MEs.
 |
Table 9 Independent Variables Influencing MEs |
Discussion
This study developed and tested a model that investigated the association between cognitive MEs and their organizational factors and work-related psychological and functional factors. To the best of our knowledge, this is the first study that combines hospitals’ organizational culture, policies, and procedures with cognitive and psychological factors including workload, stress, sleep and fatigue in order to investigate cognitive MEs.
Hospital Organizational Factors and MEs
Our findings indicated a non-significant negative association between MEs and hospital organizational factors. Hence, enhancing organizational culture would encourage safety and no-blame culture, both of which would ultimately reduce the occurrence of MEs. This non-significant relationship may be attributed to several reasons and challenges related to the process of data collection and the participants’ attitudes and perceptions. For instance, many respondents may have provided inaccurate responses in an attempt to show that their hospital had better organizational culture than other hospitals. Others may have feared being punished if they responded in a way which showed their hospital culture to be a blame culture. Despite the existence of reverse questions, most of the participants answered with “neutral” or “agree” with regards to questions related to their hospitals’ organizational culture, which may be because they believed that all culture-related questions should be answered positively. Additionally, hospital organizational culture is considered a sensitive topic for healthcare providers, and views about this topic may differ from country to country or even from person to person. Therefore, it is not surprising that our findings are not completely congruent with the findings of previous studies.
Several previous studies from different countries have evidenced that the type of organizational culture (safety or blame culture) influences the occurrence of MEs. Previous studies in the US and the United Kingdom (UK) found that the dominant culture within an organization is a main factor that influences healthcare providers’ decisions to speak up about MEs, and that blame culture negatively affects healthcare professionals’ attitudes towards being open about and reporting MEs.32,73 Similarly, studies from Iran and Lebanon found that the main reasons for healthcare professionals to not report MEs were fear of punishment and lack of knowledge, both of which are related to blame culture.1,17 In contrast, positive safety culture is associated with fewer adverse events and hospital complications; safety culture allows employees to learn from their errors and feel confident enough to report the errors they have made or witnessed.38,74,75 Developing policies and procedures on disclosing and reporting critical incidents and MEs could encourage patient safety culture and eliminate inconsistencies among healthcare settings and providers. Updated formal policies and procedures can reduce practice variation and reliance on individual’s memory, which, when overloaded, has been shown to be a main cause of cognitive MEs.16,48,76 Nonetheless, organizational culture varies across different hospitals and over time. However, our multi-group analysis using AMOS revealed no differences between governmental, educational, or private hospitals.
Psychological and Functional Factors and MEs
Our findings suggest a significant positive correlation between healthcare professionals’ psychological and functional status and the occurrence of MEs, whereby excessive workload, fatigue, stress, sleep deprivation, and complexity of tasks may be predictors of the occurrence of MEs. These findings are consistent with the findings of previous studies conducted in Canada, Turkey, Iran, and Australia, which have indicated that heavy workloads, fatigue, lack of sleep, and staff shortages are all factors causally related to the occurrence of MEs.77–80 For example, Zarea et al (2018) found that high patient-to-nurse ratio (57.3%), heavy workload (51.1%), and nurses’ fatigue due to being overworked (40.4%) were associated with an increase in the occurrence of medication errors.81 In Iran, it was reported that a heavy workload and work shift type were the main causes of medication errors by nurses, and workload was the most important reason for underreporting errors.82
All of these factors which contribute to MEs are due to deficiencies in cognitive performance, overload in memory, and impaired thought processes among healthcare professionals. For instance, several previous studies have argued that fatigue and sleep deprivation affect several cognitive processes and usually lead to changes in brain function that are likely to impair healthcare professionals’ simple decision-making performance. Sleep deprivation and subsequent fatigue can also increase rigid thinking and weaken memory when carrying out complex tasks.83,84 Given that healthcare providers work under stressful conditions that cause a variety of disorders and cognitive impairments, they may find it difficult to concentrate and organize their thoughts logically during the provision of healthcare services.85,86 In turn, this may increase the likelihood of the occurrence of cognitive MEs, hence impacting patients’ safety.
In the current study, multi-group analysis using AMOS was conducted to examine perceptions towards psychological and functional status among the healthcare providers from the three hospitals. Interestingly, the results showed that the participants from the government hospital and the private hospital perceived psychological and functional status to have a significant impact on MEs, while the participants from the university hospital did not. Likewise, a review of over 50 research articles on working conditions in public hospitals found that shortages of staff, long working hours, poor infrastructure, and budgetary constraints were the most important factors related to poor working conditions.87 Recently, it was found that staff shortage was the primary cause of MEs as perceived by Jordanian nurses and nursing students.88 The governmental public hospital included in the present study is overcrowded, as it is considered one of the main public hospitals in Northern Jordan. Therefore, the healthcare professionals working at this hospital deal with excessive workloads. According to the latest annual report published by the Jordanian Ministry of Health in 2019, the bed occupancy rate at this hospital was 93.5%, while the bed turnover rate was 96.6%.89 These figures indicate high demand for health services at this hospital, especially from patients who have public medical insurance. Additionally, the hospital’s infrastructure is not suitable for accommodating such a large number of patients, which may make the hospital overcrowded and lead the healthcare providers working at the hospital to feel overworked. On the other hand, the private hospital included in this study is considered one of the main private hospitals in the Irbid Governorate. The annual report conducted by the hospital in 2019 indicated a bed occupancy rate of 74.5%. Additionally, given the relatively high workload and the increasing number of admissions and demand for other healthcare services, the hospital management team made the decision to expand the building and include more specialty clinics. However, the hospital’s vision and mission focus on satisfying customers’ needs, exceeding customers’ expectations, and gaining a good reputation, which places extra pressure on healthcare providers to ensure the provision of high-quality health services and amenities. All of the abovementioned reasons may explain our findings regarding the heavy workloads at these two hospitals. Similar findings were reported in a study that was conducted in five governmental hospitals in Kuwait, which indicated that the major causes of adverse events were related to inadequate help available to lift or move patients (86%), inadequate time to document care (80%), verbal abuse by patients or visitors (77%), concerns about the quality of care (71%), being rushed while giving medications (64%), and physical exhaustion (62%).90
Limitations
This study used a convenience sample, which may not be representative of all healthcare providers in Jordan. Further, the majority of the respondents were nurses. The difficulty in reaching and communicating with physicians during the data collection period was one of the main barriers to the recruitment of a proportional sample of both nurses and physicians. However, as the number of clinicians (physicians and nurses) vary based on hospital type and size, a proportional sampling approach was used to increase the representativeness of the findings and thus generalizability of findings. The use of a self-administrated questionnaire is another limitation, as the participants’ responses may have been influenced by recall bias, underreporting of information, and subjective discrepancies. Despite these limitations, no prior studies have considered such a range of dimensions linked to cognitive MEs and the factors that contribute to the occurrence of such errors. Finally, this study is the first study in Jordan to compare between governmental, university, and private hospitals with regards to the occurrence of cognitive MEs.
Conclusion
In conclusion, hospitals need to enhance their organizational culture in order to encourage safety and no-blame culture and hence reduce MEs. Thus, the focus should be placed on both organizational and individual levels. Our findings indicate a significant association between healthcare professionals’ psychological and functional status and the occurrence of cognitive MEs. Excessive workload, fatigue, stress, sleep deprivation, and complexity of tasks among healthcare providers are factors which may directly impact the occurrence of MEs and which therefore need to be considered by decision-makers in healthcare settings. Moreover, healthcare providers work under stressful conditions, which may cause cognitive impairments leading to cognitive MEs and hence impacting patients’ safety. One step towards reducing the occurrence of MEs is to decrease the nurse/doctor to patient ratio. Further, healthcare providers need to be made aware of the importance of complying with policies and procedures, as they provide healthcare professionals with up-to-date instructions related to the appropriate provision of care without the need to rely on memory. This ensures consistency of practice and leads to a reduction in MEs, particularly errors that occur as a result of overload in memory. To this end, future research can adopt our newly developed instrument to investigate the impact of the individual and organizational factors on cognitive MEs at different settings in different countries. Future research should also focus on the magnitude of the cognitive MEs and their real impact on healthcare providers and patient safety, as well as strategies and interventions that could reduce human errors in healthcare organizations.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Institutional Review Board (IRB) committee at Jordan University of Science and Technology, the Jordanian Ministry of Health (MOH), and the administrators of the selected hospitals. Permission to distribute the questionnaire was obtained from the heads of department at the three selected hospitals. Prior to data collection, informed consent was obtained from the participants, who were made fully aware of the study significance and purposes.
Funding
This study was funded by the Deanship of Research/Jordan University of Science and Technology.
Disclosure
The authors report that they have no competing interests in this work.
References
1. Safarpour H, Tofighi M, Malekyan L, Bazyar J, Varasteh S, Anvary R. Patient safety attitudes, skills, knowledge and barriers related to reporting medical errors by nursing students. Int J Clin Med. 2017;8:1–11. doi:10.4236/ijcm.2017.81001
2. Flotta D, Rizza P, Bianco A, Pileggi C, Pavia M. Patient safety and medical errors: knowledge, attitudes and behavior among Italian hospital physicians. Int J Qual Health Care. 2012;24(3):258–265. doi:10.1093/intqhc/mzs014
3. GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age–sex specifi c all-cause and cause-specifi c mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi:10.1016/S0140-6736(14)61682-2.
4. Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139. doi:10.1136/bmj.i21395
5. Hogan H, Zipfel R, Neuburger J, Hutchings A, Darzi A, Black N. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ. 2015;351:h3239. doi:10.1136/bmj.h3239
6. Baker GR, Norton PG, Flintoft V, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–1686. doi:10.1503/cmaj.1040498
7. Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ. 2001;322(7285):517–519. doi:10.1136/bmj.322.7285.517
8. Abdel-Qader DH, Al Meslamani AZ, El-Shara’ AA, et al. Investigating prescribing errors in the emergency department of a large governmental hospital in Jordan. J Pharm Health Serv Res. 2020;11(4):375–382. doi:10.1111/jphs.12376
9. Abdel-Qader DH, Saadi Ismael N, Al Meslamani AZ, et al. The role of clinical pharmacy in preventing prescribing errors in the emergency department of a governmental hospital in Jordan: a pre-post study. Hosp Pharm. 2020;2020. doi:10.1177/0018578720942231
10. Mrayyan MT. Reported incidence, causes, and reporting of medication errors in teaching hospitals in Jordan: a comparative study. Contemp Nurse. 2012;41(2):216–232. doi:10.5172/conu.2012.41.2.216
11. Mrayyan MT, Al-Atiyyat N. Medication errors in university-affiliated teaching hospitals as compared to non-university-affiliated teaching hospitals in Jordan. Nurs Forum. 2011;46(4):206–217. doi:10.1111/j.1744-6198.2011.00241.x
12. Ali L, Saifan A, Alrimawi I, Atout M. Nurses’ perceptions toward factors that cause medication errors in Jordan: a qualitative study. Perspect Psychiatr Care. 2020. doi:10.1111/ppc.12707
13. Mrayyan MT, Shishani K, Al-Faouri I. Rate, causes and reporting of medication errors in Jordan: nurses’ perspectives. J Nurs Manag. 2007;15(6):659–670. doi:10.1111/j.1365-2834.2007.00724.x
14. Alrabadi N, Haddad R, Haddad R, et al. Medication errors among registered nurses in Jordan. J Pharm Health Serv Res. 2020;11(3):237–243. doi:10.1111/jphs.12348
15. Matin BK, Hajizadeh M, Nouri B, Rezaeian S, Mohammadi M, Rezaei S. Period prevalence and reporting rate of medication errors among nurses in Iran: a systematic review and meta-analysis. J Nurs Manag. 2018;26(5):498–508. doi:10.1111/jonm.12579
16. Kalra J, Kalra N, Baniak N. Medical error, disclosure and patient safety: a global view of quality care. Clin Biochem. 2013;46(13–14):1161–1169. doi:10.1016/j.clinbiochem.2013.03.025
17. El-Jardali F, Jaafar M, Dimassi H, Jamal D, Hamdan R. The current state of patient safety culture in Lebanese hospitals: a study at baseline. Int J Qual Health Care. 2010;22(5):386–395. doi:10.1093/intqhc/mzq047
18. Elder NC, Dovey SM. Classification of medical errors and preventable adverse events in primary care: a synthesis of the literature. J Fam Pract. 2002;51(11):927–932.
19. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. In: Kohn LT, Corrigan JM, Donaldson MS, eds. Washington (DC): National Academies Press (US); 2000.
20. Zhang J, Patel VL, Johnson TR, Shortliffe EH. A cognitive taxonomy of medical errors. J Biomed Inform. 2004;37(3):193–204. doi:10.1016/j.jbi.2004.04.004
21. Ferner RE, Aronson J. Clarification of terminology in medication errors. Drug Safety. 2006;29(11):1011–1022. doi:10.2165/00002018-200629110-00001
22. Reason J. Safety in the operating theatre - Part 2: human error and organisational failure. Qual Saf Health Care. 2005;14(1):56–60.
23. Wiseman S, Cairns P, Cox A A taxonomy of number entry error.
24. Embrey D. Understanding human behaviour and error. Human Reliability Assoc. 2005;1:1–10.
25. Lin CJ, Yenn T-C, Yang C-W. Optimizing human–system interface automation design based on a skill-rule-knowledge framework. Nuclear Eng Design. 2010;240(7):1897–1905. doi:10.1016/j.nucengdes.2010.03.026
26. McDowell SE, Ferner HS, Ferner RE. The pathophysiology of medication errors: how and where they arise. Br J Clin Pharmacol. 2009;67(6):605–613. doi:10.1111/j.1365-2125.2009.03416.x
27. Sirota RL. Error and error reduction in pathology. Arch Pathol Lab Med. 2005;129(10):1228–1233. doi:10.1043/1543-2165(2005)129[1228:EAERIP]2.0.CO;2
28. Stock GN, McFadden KL, Gowen CR. Organizational culture, critical success factors, and the reduction of hospital errors. Int J Prod Econ. 2007;106(2):368–392. doi:10.1016/j.ijpe.2006.07.005
29. Chen I-C, Ng H-F, Li -H-H. A multilevel model of patient safety culture: cross-level relationship between organizational culture and patient safety behavior in Taiwan’s hospitals. Int J Health Plann Manage. 2012;27(1):e65–e82. doi:10.1002/hpm.1095
30. Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ. 2018;363:k4907. doi:10.1136/bmj.k4907
31. Ismail Ababaneh R. The role of organizational culture on practising quality improvement in Jordanian public hospitals. Leadersh Health Serv. 2010;23(3):244–259. doi:10.1108/17511871011061064
32. Levine KJ, Carmody M, Silk KJ. The influence of organizational culture, climate and commitment on speaking up about medical errors. J Nurs Manag. 2020;28(1):130–138. doi:10.1111/jonm.12906
33. Hartmann CW, Meterko M, Rosen AK, et al. Relationship of hospital organizational culture to patient safety climate in the veterans health administration. Med Care Res Rev. 2009;66(3):320–338. doi:10.1177/1077558709331812
34. Singer S, Lin S, Falwell A, Gaba D, Baker L. Relationship of safety climate and safety performance in hospitals. Health Serv Res. 2009;44:399–421. doi:10.1111/j.1475-6773.2008.00918.x
35. Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM. Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:369–374. doi:10.7326/0003-4819-158-5-201303051-00002
36. Palatnik AM. Speak up for patient safety. Nurs Crit Care. 2016;11(6):4. doi:10.1097/01.Ccn.0000503425.05594.02
37. Jafree SR, Zakar R, Zakar MZ, Fischer F. Nurse perceptions of organizational culture and its association with the culture of error reporting: a case of public sector hospitals in Pakistan. BMC Health Serv Res. 2016;16:3. doi:10.1186/s12913-015-1252-y
38. Karsh B-T, Escoto KH, Beasley JW, Holden RJ. Toward a theoretical approach to medical error reporting system research and design. Appl Ergon. 2006;37(3):283–295. doi:10.1016/j.apergo.2005.07.003
39. Mohsin SU, Ibrahim Y, Levine D. Teaching medical students to recognise and report errors. BMJ Open Qual. 2019;8(2):e000558.
40. Khatri N, Brown GD, Hicks LL. From a blame culture to a just culture in health care. Health Care Manage Rev. 2009;34(4):312–322. doi:10.1097/HMR.0b013e3181a3b709
41. Gorini A, Miglioretti M, Pravettoni G. A new perspective on blame culture: an experimental study. J Eval Clin Pract. 2012;18:671–675. doi:10.1111/j.1365-2753.2012.01831.x
42. Campbell EG, Regan S, Gruen RL, et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147(11):795–802. doi:10.7326/0003-4819-147-11-200712040-00012
43. Kaldjian LC, Jones EW, Wu BJ, Forman-Hoffman VL, Levi BH, Rosenthal GE. Reporting medical errors to improve patient safety: a survey of physicians in teaching hospitals. Arch Intern Med. 2008;168(1):40–46. doi:10.1001/archinternmed.2007.12
44. Rashid Z, Khan HT, Rehman F, Ahmad S, Niazi S, Sarwar MZ. Attitudes and practice of surgeons in reporting medical errors at 3 a tertiary care hospital 4. J Pak Med Assoc. 2020;1–10. doi:10.5455/JPMA.19325
45. Bayazidi S, Zarezadeh Y, Zamanzadeh V, Parvan K. Medication error reporting rate and its barriers and facilitators among nurses. J Caring Sci. 2012;1(4):231–236. doi:10.5681/jcs.2012.032
46. Khater WA, Akhu-Zaheya LM, Al-Mahasneh SI, Khater R. Nurses’ perceptions of patient safety culture in Jordanian hospitals. Int Nurs Rev. 2015;62(1):82–91. doi:10.1111/inr.12155
47. Nieva VF, Sorra J. Safety culture assessment: a tool for improving patient safety in healthcare organizations. Qual Saf Health Care. 2003;12(suppl 2):ii17. doi:10.1136/qhc.12.suppl_2.ii17
48. Irving A. Policies and procedures for healthcare organizations: a risk management perspective. PSQH. 2014.
49. Vaishnavi V, Suresh M, Dutta P. A study on the influence of factors associated with organizational readiness for change in healthcare organizations using TISM. Benchmarking. 2019;26(4):1290–1313. doi:10.1108/BIJ-06-2018-0161
50. Hart SG, Staveland LE. Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. Adv Psychol. 1988;139–183. doi:10.1016/S01664115(08)62386-9
51. Haga S, Shinoda H, Kokubun M. Effects of task difficulty and time‐on‐task on mental workload. Jpn Psychol Res. 2002;44(3):134–143. doi:10.1111/1468-5884.00016
52. Griffiths P, Dall’Ora C, Simon M, et al. Nurses’ shift length and overtime working in 12 European countries: the association with perceived quality of care and patient safety. Med Care. 2014;52(11):975–981. doi:10.1097/MLR.0000000000000233
53. Magalhães A, Dall’Agnol CM, Marck PB. Nursing workload and patient safety-a mixed method study with an ecological restorative approach. Rev Lat Am Enfermagem. 2013;21(SPE):146–154. doi:10.1590/S0104-11692013000700019
54. Caruso CC. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014;39(1):16–25. doi:10.1002/rnj.107
55. Källberg AS, Göransson KE, Florin J, Östergren J, Brixey JJ, Ehrenberg A. Contributing factors to errors in Swedish emergency departments. Int Emerg Nurs. 2015;23(2):156–161. doi:10.1016/j.ienj.2014.10.002
56. Kalisch BJ, Aebersold M. Interruptions and multitasking in nursing care. Joint Commis J Qual Patient Saf. 2010;36(3):126–132. doi:10.1016/S1553-7250(10)36021
57. Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487. doi:10.1371/journal.pmed.0030487
58. Patterson PD, Weaver MD, Frank RC, et al. Association between poor sleep, fatigue, and safety outcomes in emergency medical services providers. Prehosp Emerg Care. 2012;16(1):86–97. doi:10.3109/10903127.2011.616261
59. Stimpfel AW, Fatehi F, Kovner C. Nurses’ sleep, work hours, and patient care quality, and safety. Sleep Health. 2020;6(3):314–320. doi:10.1016/j.sleh.2019.11.001
60. Rhéaume A, Mullen J. The impact of long work hours and shift work on cognitive errors in nurses. J Nurs Manag. 2018;26(1):26–32. doi:10.1111/jonm.12513
61. Khanade K, Sasangohar F. Stress, fatigue, and workload in intensive care nursing: a scoping literature review. Proc Human Factors Ergon Soc Ann Meeting. 2017;61(1):686–690. doi:10.1177/1541931213601658
62. O’Connor DB, Thayer JF, Vedhara K. Stress and health: a review of psychobiological processes. Annu Rev Psychol. 2021;72:663–688. doi:10.1146/annurev-psych-062520-122331
63. Karasek RAJA. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;24(2):285–308. doi:10.2307/2392498
64. Williams B, Onsman A, Brown T. Exploratory factor analysis: a five-step guide for novices. Australas J Paramed. 2010;8(3). doi:10.33151/ajp.8.3.93
65. Watkins MW. Exploratory factor analysis: a guide to best practice. J Black Psychol. 2018;44(3):219–246. doi:10.1177/0095798418771807
66. Awang Z. Validating the Measurement Model: CFA. A Handbook on SEM.
67. Hutcheson GD, Sofroniou N. The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models. SAGE; 1999.
68. Tabachnick B, Fidell L. Using Multivariate Statistics.
69. Henseler J. Bridging design and behavioral research with variance-based structural equation modeling. J Advert. 2017;46(1):178–192. doi:10.1080/00913367.2017.1281780
70. Baistaman J, Awang Z, Afthanorhan A, Rahim M. Developing and validating the measurement model for financial literacy construct using confirmatory factor analysis. Human Soc Sci Rev. 2020;8:413–422. doi:10.18510/hssr.2020.8247
71. Ahmad S, Zulkurnain NNA, Khairushalimi FI. Assessing the validity and reliability of a measurement model in structural equation modeling (SEM). J Adv Math Comp Sci. 2016;15(3):1–8. doi:10.9734/BJMCS/2016/25183
72. Valentini F, Damasio BF. Average variance extracted and composite reliability: reliability coefficients/variancia media extraida e confiabilidade composta: indicadores de Precisao. Psicologia: Teoria e Pesquisa. 2016;32.
73. Waring JJ. Beyond blame: cultural barriers to medical incident reporting. Soc Sci Med. 2005;60(9):1927–1935. doi:10.1016/j.socscimed.2004.08.055
74. Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6(4):226–232. doi:10.1097/PTS.0b013e3181fd1a00
75. Smith SA, Yount N, Sorra J. Exploring relationships between hospital patient safety culture and consumer reports safety scores. BMC Health Serv Res. 2017;17(1):143. doi:10.1186/s12913-017-2078-6
76. Liang BA. A system of medical error disclosure. Qual Saf Health Care. 2002;11(1):64–68. doi:10.1136/qhc.11.1.64
77. Vogel L. Canadian medical residents report pervasive harassment, crushing workloads. CMAJ. 2018;190(46):E1371–E1371.
78. Jacobs S, O’Beirne M, Derfiingher L, Vlach L, Rosser W, Drummond N. Errors and adverse events in family medicine developing and validating a Canadian taxonomy of errors. Can Fam Physician. 2007;53(2):270.
79. Kahriman İ, Öztürk H. Evaluating medical errors made by nurses during their diagnosis, treatment and care practices. J Clin Nurs. 2016;25(19–20):2884–2894. doi:10.1111/jocn.13341
80. Bolandianbafghi S, Salimi T, Rassouli M, Faraji R, Sarebanhassanabadi M. Correlation between medication errors with job satisfaction and fatigue of nurses. Electron Physician. 2017;9(8):5142–5148. doi:10.19082/5142
81. Zarea K, Mohammadi A, Beiranvand S, Hassani F, Baraz S. Iranian nurses’ medication errors: a survey of the types, the causes, and the related factors. Int J Afr Nurs Sci. 2018;8:112–116.
82. Fathi A, Hajizadeh M, Moradi K, et al. Medication errors among nurses in teaching hospitals in the west of Iran: what we need to know about prevalence, types, and barriers to reporting. Epidemiol Health. 2017;39:e2017022–e2017022. doi:10.4178/epih.e2017022
83. Alhola P, Polo-Kantola P. Sleep deprivation: impact on cognitive performance. Neuropsychiatr Dis Treat. 2007;3(5):553–567.
84. Harrison Y, Horne JA. One night of sleep loss impairs innovative thinking and flexible decision making. Organ Behav Hum Decis Process. 1999;78(2):128–145. doi:10.1006/obhd.1999.2827
85. Gelsema TI, Van Der Doef M, Maes S, Janssen M, Akerboom S, Verhoeven C. A longitudinal study of job stress in the nursing profession: causes and consequences. J Nurs Manag. 2006;14(4):289–299. doi:10.1111/j.1365-2934.2006.00635.x
86. Donovan O, Doody O, Lyons R. The effect of stress on health and its implications for nursing. Br J Nurs. 2013;22(16):969–973. doi:10.12968/bjon.2013.22.16.969
87. Manyisa ZM, van Aswegen EJ. Factors affecting working conditions in public hospitals: a literature review. Int J Afr Nurs Sci. 2017;6:28–38. doi:10.1016/j.ijans.2017.02.002
88. Ta’an W, Suliman MM, Al-Hammouri MM, Ta’an A. Prevalence of medical errors and barriers to report among nurses and nursing students in Jordan: a cross-sectional study. Nurs Forum. 2020. doi:10.1111/nuf.12542
89. Ministry of Health. Annual Statistical Book; 2019. Amman-Jordan: Department of Studies and Information. Available from: https://www.moh.gov.jo/Echobusv3.0/SystemAssets/c3c6fc8e-9e95-4772-b143-5fac9c900279.pdf.
90. Al-Kandari F, Thomas D. Adverse nurse outcomes: correlation to nurses’ workload, staffing, and shift rotation in Kuwaiti hospitals. Appl Nurs Res. 2008;21(3):139–146. doi:10.1016/j.apnr.2006.10.008
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
