Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
The appropriate troponin T level associated with coronary occlusions in chronic kidney disease patients
Authors Sitthichanbuncha Y, Sricharoen P, Tangkulpanich P , Sawanyawisuth K
Received 29 March 2015
Accepted for publication 17 June 2015
Published 4 August 2015 Volume 2015:11 Pages 1143—1147
DOI https://doi.org/10.2147/TCRM.S85671
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Yuwares Sittichanbuncha,1 Pungkava Sricharoen,1 Panvilai Tangkulpanich,1 Kittisak Sawanyawisuth2,3
1Department of Emergency Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, 2Department of Medicine, Faculty of Medicine, 3Research Center in Back, Neck, Other Joint Pain and Human Performance (BNOJPH), Khon Kaen University, Khon Kaen, Thailand
Background: High-sensitivity troponin T (HS Trop T) plays an important role as a diagnostic marker for acute coronary syndrome. It is also related to cardiovascular outcomes. HS Trop T levels may be varied in individuals with renal dysfunction. This study aimed to find the appropriate HS Trop T cutoff points in chronic kidney disease (CKD) patients who had coronary artery occlusion.
Patients and methods: The study was conducted at the Emergency Department, Ramathibodi Hospital, Mahidol University, Thailand. CKD patients stage 3–5 who had HS Trop T levels after 2 hours of chest pain and had coronary angiographic results were enrolled. Patients were divided into two groups: those who had significant occlusion of more than 70% of a coronary artery as the coronary artery disease (CAD) group and the non-CAD group.
Results: In total, 210 patients met the study criteria. There were 132 patients (62.86%) who had significant stenosis of coronary arteries by coronary angiograms. The average age (standard deviation) of all patients was 71.02 (9.49) years. HS Trop T levels were significantly higher in all CKD patients with CAD than the non-CAD group (0.4973 versus 0.0384 ng/mL). Sex and HS Trop T levels were significantly associated with CAD by multivariate logistic regression analysis. The HS Trop T level of 0.041 ng/mL gave sensitivity and specificity of 65.91% and 75.65%, respectively, for CAD.
Conclusion: The HS Trop T level of 0.041 ng/mL provided diagnostic properties for established coronary artery occlusion in CKD patients.
Keywords: high-sensitivity troponin T, acute coronary syndrome, coronary artery occlusion, chronic kidney disease, sensitivity, specificity, coronary angiogram
Introduction
Acute coronary syndrome (ACS) is a common disease at emergency departments, and has high morbidity and mortality.1 Cardiac biomarkers are a useful diagnostic tool for ACS.2–4 High-sensitivity troponin T (HS Trop T) is very specific to myocardial tissue, and a level of more than 0.014 ng/mL has specificity to acute myocardial infarction in normal renal function patients.5
Chronic kidney disease (CKD) is a common disease in clinical practice and increases risk for ACS. Serum Trop T levels of renal dysfunction patients may be higher than the normal population, resulting in higher cutoff points.6 The cutoff point of HS Trop T for ACS with renal dysfunction may be higher than normal population.7,8 The diagnosis of ACS may need to be confirmed by coronary angiogram, but some studies have used clinical diagnosis of ACS.7,8 This study aimed to find the appropriate HS Trop T cutoff points in CKD patients who presented with ACS and had coronary artery occlusion by coronary angiogram. Factors associated with coronary occlusion in CKD patients who are suspected to have ACS were also studied.
Patients and methods
The study was conducted at the Department of Emergency, Ramathibodi Hospital, Mahidol University, Thailand. CKD patients stages 3–5 who had HS Trop T levels (Hoffman-La Roche Ltd, Basel, Switzerland) after 2 hours of chest pain and had coronary angiographic results were enrolled. Patients who had received hemodialysis therapy or who had been diagnosed with non-coronary artery disease (non-CAD) by coronary angiogram were excluded. The study period was between June 1, 2010 and June 30, 2013.
Eligible patients were identified by using International Classification of Diseases 9 code 88.5 (clinical medication procedure code). Charts of eligible patients were retrospectively reviewed. Baseline characteristics, comorbid diseases, medications, history of smoking, HS Trop T levels, serum creatinine, and coronary angiographic results were recorded. CKD was classified by estimated glomerular filtration rate (eGFR) as stages 3–5 with eGFR of 31–60, 15–30, and <5 mL/min/1.73 m2. eGFR was calculated by the Chronic Kidney Disease Epidemiology Collaboration formula. Serum creatinine on the date of the emergency room visit was used to calculate eGFR.
ACS was diagnosed by clinical findings of chest pain, HS Trop T, and ECG.3 The thrombolysis in myocardial infarction (TIMI) risk score was calculated.9 Significant CAD was defined by the presence of coronary artery occlusion of more than 70% of the culprit coronary artery or arteries.
Statistical analyses
Patients were divided into two groups by significant occlusion of more than 70% of a coronary artery as CAD and non-CAD. Baseline and clinical characteristics of patients in both groups were compared using descriptive statistics. Univariate logistic regression analyses were applied to calculate the crude odds ratios (ORs) of individual variables for CAD. All clinically important variables or results of univariate analyses with a P-value less than 0.10 were included in subsequent multivariate logistic regression analyses. Analytical results were presented as adjusted ORs and 95% confidence intervals. Various cutoff points of HS Trop T were calculated by using receiver operating characteristic (ROC) analysis. The areas under ROC curves, sensitivity, specificity, and predictive values of all cutoff points were also executed. The association of HS Trop T levels and various factors were also calculated by multivariate logistic regression analyses. All data analyses were performed with Stata software (StataCorp LP, College Station, TX, USA). The study protocol was approved by the Ethics Committee in Human Research, Mahidol University.
Results
There were 1,550 patients who had HS Trop T results and coronary angiographic results. Of those, 282 patients met the study criteria. We excluded 72 patients due to hemodialysis (42 patients), inappropriate time of HS Trop T level (22 patients), stress-induced cardiomyopathy (five patients), and pulmonary embolism (three patients). In total, 210 patients were included in the analysis. There were 132 patients (62.86%) who had significant coronary artery stenosis by coronary angiogram. Triple-vessel disease was the most common CAD (83 patients); double-vessel disease and single-vessel disease were found in 26 and 23 patients, respectively.
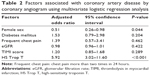
The average age (standard deviation) of all patients was 71.02 (9.49) years. Being of male sex, having diabetes mellitus, and significantly higher TIMI risk scores were found in the CAD group (Table 1). The mean eGFR of CAD was significantly lower in the CAD group than the non-CAD group: 38.91 versus 42.81 mL/min/1.73 m2 (P=0.031). HS Trop T levels were significantly higher in all CKD patients with CAD than in the non-CAD group (0.4973 versus 0.0384 ng/mL, P=0.008), and when classified by stage in CKD 3 but not in 5 (Table 1). Two factors were significantly associated with CAD by multivariate logistic regression analysis (Table 2). Female sex and HS Trop T levels had adjusted ORs (95% confidence interval) of 0.51 (0.26–0.98) and 5.92 (3.02–11.60).
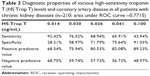
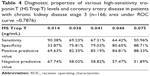
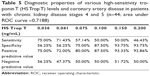
For all CKD patients, the cutoff points for HS Trop T and CAD are shown in Table 3 and Figure 1. The area under the ROC curve was 77.15%, giving sensitivity and specificity of 65.91% and 75.65%, respectively, for the cutoff point of 0.041 ng/mL. The cutoff point of HS Trop T at 0.041 gave sensitivity and specificity of 67.31% and 79.03% (CKD stage 3; Table 4 and Figure 2) and 71.43% and 56.25% (CKD stages 4 and 5; Table 5 and Figure 3), respectively.
  | Figure 1 Receiver operating characteristic (ROC) curve of high-sensitivity troponin T levels and coronary artery disease in all patients (n=210). |
  | Figure 2 Receiver operating characteristic (ROC) curve of high-sensitivity troponin T levels and coronary artery disease in chronic kidney disease stage 3 (n=166). |
  | Figure 3 Receiver operating characteristic (ROC) curve of high-sensitivity troponin T levels and coronary artery disease in chronic kidney disease stages 4 and 5 (n=44). |
Discussion
Third-generation Trop T has been shown to be a predictor of future CAD and associated with mortality in CKD patients.10,11 This study added the correlation of HS Trop T and significant coronary occlusion with an adjusted OR of 5.92 in CKD patients (Table 2). Sex is another significant factor (Table 2). As in previous reports, males were at higher risk for CAD than females. After adjustment by multivariate logistic regression analysis, TIMI score and GFR became non-significant factors for coronary occlusion (Tables 1 and 2). These results may indicate that sex and HS Trop T levels were the only two independent factors associated with significant coronary occlusion, but not GFR level or disease severity.
A study from France suggested using an HS Trop T cutoff point at 0.0358 ng/mL for acute myocardial infarction in patients with CKD. Its sensitivity and specificity were 94% and 86%, respectively.12 Another study conducted in the US compared HS Trop T levels in 51 CKD patients with 112 normal renal function patients who had ACS.7 The sensitivity of ACS diagnosis increased from 63% to 87% if the cutoff point of HS Trop T increased from 0.1 to 0.5 ng/mL. For a Thai population, the Trop T level of 0.1 ng/mL gave sensitivity of 90.90% and specificity of 84.50% in CKD patients with suspected ACS compared with CKD patients without ACS symptoms.13 Other studies also showed that the cutoff point for HS Trop T to diagnose acute myocardial infarction needs to be adjusted by the GFR.14–16
In this study, the cutoff point of HS Trop T at 0.041 ng/mL gave sensitivities from 65.91% to 71.45% and specificities of 71.43% and 79.03% overall and CKD stage 3, respectively. Specificity dropped to 56.25% in CKD stage 4 and 5 (Table 4 and 5). The decreasing of sensitivities by GFR may explain by the high baseline HS Trop T level in low GFR.14–16 Note that these diagnostic properties were indications of coronary occlusion by coronary angiogram, not for diagnosis of acute myocardial infarction as in previous studies.12–16
The strength of this study is that all subjects had coronary angiograms performed to confirm the CAD. There are some limitations in this study, including small sample size, retrospective data collection, and generation of HS Trop T. The results therefore may not be applicable for the newer generations of Trop T or another cardiac marker (troponin I). The study population was limited, due to the use of newer-generation HS Trop T in this hospital. Finally, due to the retrospective study design, the study population in the CAD and non-CAD groups may not have been equally distributed. The numbers of patients with high TIMI score, CKD stage 4, and CKD stage 5 were higher in the CAD group than the non-CAD group (12.88% versus 6.41%; 15.91% versus 20.51%; 5.30% versus 0%), as shown in Table 1. However, after controlling of these factors by using multivariate logistic regression analysis, both TIMI score and CKD stage were not an independent factor for having CAD.
Conclusion
The HS Trop T level of 0.041 ng/mL provided diagnostic properties for established coronary artery occlusion in chronic kidney disease patients.
Acknowledgment
We would like to thank Professor James A Will (University of Wisconsin) for his kind review of the paper.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Cardiovascular Diseases (CVDs): Fact Sheet 317. 2015. Available from: http://www.who.int/mediacentre/factsheets/fs317/en. Accessed July 6, 2015. | ||
O’Connor RE, Brady W, Brooks SC, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S787–S817. | ||
Hamm CW, Bassand JP, Agewall S, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054. | ||
Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. 2007;116:2634–2653. | ||
Christenson RH, Phillips D. Sensitive and high sensitivity next generation cardiac troponin assays: more than just a name. Pathology. 2011;43:213–219. | ||
Hamm CW, Giannitsis E, Katus HA. Cardiac troponin elevations in patients without acute coronary syndrome. Circulation. 2002;106:2871–2872. | ||
Van Lente F, McErlean ES, DeLuca SA, Peacock F, Rao JS, Nissen SE. Ability of troponin to predict adverse outcomes in patients with renal insufficiency and suspected acute coronary syndromes: a case-matched study. J Am Coll Cardiol. 1999;33:471–478. | ||
Chotivanawan T, Krittayaphong R. Normal range of serum highly-sensitive troponin-T in patients with chronic kidney disease stage 3–5. J Med Assoc Thai. 2012;95 Suppl 2:S127–S132. | ||
Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. | ||
Apple FS, Murakami MM, Pearce LA, Herzog CA. Predictive value of cardiac troponin I and T subsequent death in end-stage renal disease. Circulation. 2002;106:2941–2945. | ||
Aviles RJ, Askari AT, Lindahl B, et al. Troponin T levels in patients with acute coronary syndromes, with or without renal dysfunction. N Engl J Med. 2002;346:2047–2052. | ||
Chenevier-Gobeaux C, Meune C, Freund Y, et al. Influence of age and renal function on high-sensitivity cardiac troponin T diagnostic accuracy for the diagnosis of acute myocardial infarction. Am J Cardiol. 2013;111:1701–1707. | ||
Sukonthasarn A, Ponglopisit S. Diagnostic level of cardiac troponin T in patients with chronic renal dysfunction, a pilot study. J Med Assoc Thai. 2007;90:1749–1758. | ||
Parikh RH, Seliger SL, deFilippi CR. Use and interpretation of high sensitivity cardiac troponins in patients with chronic kidney disease with and without acute myocardial infarction. Clin Biochem. 2015;48:247–253. | ||
Dubin RF, Li Y, He J, et al. Predictors of high sensitivity cardiac troponin T in chronic kidney disease patients: a cross-sectional study in the chronic renal insufficiency cohort (CRIC). BMC Nephrol. 2013;14:229. | ||
Pfortmueller CA, Funk GC, Marti G, et al. Diagnostic performance of high-sensitive troponin T in patients with renal insufficiency. Am J Cardiol. 2013;112:1968–1972. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.