Back to Journals » International Medical Case Reports Journal » Volume 16
Testicular Tuberculosis: Two Rare Case Report
Authors Mohamed Alı A , Doğan A , Ali MA , Çakmak BS
Received 1 March 2023
Accepted for publication 30 May 2023
Published 5 June 2023 Volume 2023:16 Pages 339—343
DOI https://doi.org/10.2147/IMCRJ.S408874
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Ahmed Mohamed Alı,1 Ahmet Doğan,1 Mukhtar Abdullahi Ali,1 Battal Selçuk Çakmak2
1Department of Infectious Diseases and Clinical Microbiology, Somalia-Mogadishu- Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia; 2Department of Urology, Somalia- Mogadishu- Turkey Recep Tayyip Erdogan Training and Research Hospital, Mogadishu, Somalia
Correspondence: Ahmet Doğan, Tel +9 537 484 5047, Email [email protected]
Abstract: Tuberculosis is especially common in African countries where HIV is common. Although pulmonary tuberculosis is generally seen, testicular tuberculosis can rarely be seen in young men. Especially in African countries, it is not possible to study acid-resistant bacilli, polymerase-chain reaction and culture due to financial impossibility. For this reason, history, physical examination, scrotal ultrasonography and fine needle biopsy help in diagnosis in suspected cases of testicular tuberculosis. Cure is possible with six months of treatment.
Keywords: testicular tuberculosis, rare case, caseifying necrotizing granuloma
Introduction
Globally, 10.6 million cases of tuberculosis (TB) were reported in 2021. 6.4 million males, 3.4 million women, and 1.2 million kids. TB exists in all nations and among all age groups. However, TB can be treated and avoided.1 Although TB most frequently affects the lungs, it can affect any region of the body. TB that affects a bodily component other the lungs is referred to as extrapulmonary TB. Up to 15–25% of cases of TB involve the extrapulmonary organs.2 Genitourinary TB can be seen in both immunocompetent and immunocompromised patients. Male genital TB is uncommon, and it frequently co-occurs with renal TB. The most often involved locations are the prostate and epididymis. Epididymitis is frequently linked to isolated testicular TB, which is uncommon. The issue with these forms of TB is that a precise diagnosis might be challenging to make since clinical symptoms and imaging test results may be ambiguous. It is frequently required to use invasive diagnostic procedures to gather biological samples for diagnosis, such as computerized axial tomography (CAT)-guided fine needle aspiration biopsy (FNAB) or ultrasonography. Although molecular techniques for early mycobacteria DNA detection have become more popular and advanced recently, cultures remain the gold standard for making a reliable microbiological diagnosis.2–7 In this report, we aimed to report two rare cases of testicular TB.
Case 1
In September 10, 2022, an 18-year-old male patient presented with right testicular swelling associated with ulcer, fever, and night sweats. There was no weight loss. There was no history of TB or any other chronic disease. On physical examination, he was conscious and his general condition was good. Vital signs: heart rate: 110 bpm, respiratory rate: 23/mn, blood pressure: 130/80 mmHg and SPO2: 98. In the genital examination, unilateral right testicular swelling, round erythematous, mobile, no discharge, painless scrotal ulcer was present. There was no pathological feature in the other system examination. Examining laboratory tests: Hemogram sedimentation and biochemistry values were normal. Hepatitis serology (HBs Ag, Anti HBs, Anti HCV), syphilis (Treponema Pallidum Hemagglutination Assay) and HIV (Anti HIV test) Eliza were negative. There was no pathology in the posteroanterior chest radiograph. The biopsy specimen was stained with hematoxylin eosin and examined by direct microscopy. Areas of caseification leading to necrosis were seen (Figure 1).
 |
Figure 1 Caseified necrotison granüloma (Hematoxcillin&Eosin stain). |
The patient’s testicular examination revealed a unilateral palpable nodular mass (Figure 2).
 |
Figure 2 Unilateral ulcerated nodule in testis. |
The patient was diagnosed with a definitive diagnosis according to the biopsy result, and four anti-TB treatments were planned (rifampicin 1×600 mg, isoniazid 1x300mg, pyrazinamide 1×1500 mg and ethambutol 1×1000 mg). The patient was followed up.
Case 2
A 26-year-old male patient complained of fever and night sweats in addition to severe right testicular swelling and pain for three days. Due to a small testicular tumor, he visited another hospital before coming to ours. They attempted a biopsy, which made things worse and caused huge testicular edema that grew larger and was hematous. He had anorexic and but his body weight loss was present. He had history of respiratory TB 11 years ago which was treated and he was smoker but non-alcoholic. In vital signs, temperature: 38°C, pulse: 111/mn, blood pressure: 135/81mmHg. Other systemics were unremarkable no other systemic involvement. Right testis were swelled tender firm and fixed to overlying skin. It gradually increased and there was no discharge or sinus. The laboratory tests: White Blood Cells 6.71 x 1000/mm3, Hemoglobin 11.1 g/dL, Platelet 298x1000/mm3, Neutrophıl 4.55x1000/mm3, Lymphocyte 1.33x1000/mm3, C-Reactive Protein 22 mg/l, Aspartate transferase 18 U/L, Alanine Aminotransferase 9 U/L. Chest X-ray was normal. On scrotal ultrasound reveals an irregularly circumscribed mass lesion containing hypoechoic necrotic heterogeneous areas of approximately 20×15 mm was observed in the inferior right testis (TB?). There was a 81x63mm sized hypoechoic heterogeneous lesion in the right hemiscrotum. A collection containing hypoechoic and multiple pseudonodular heterogeneous areas measuring 9×7 cm in size was observed in the right hemiscrotum (Right scrotal hematoma?). An irregularly circumscribed mass lesion containing hypoechoic necrotic heterogeneous areas of approximately 27×17 mm in the right testis inferior without vascularity was observed (Granulomatous TB? Mass?). FNAB was recommended. So we diagnosed caseating granulomatous inflammation and histopathological findings were compatible with TB (Figures 3 and 4). We made testicular exploration and hematoma was evacuated from the sac, and after operation we started anti-TB treatment regimen consisting of rifampicin, isoniazid, pyrazinamide, and ethambutol for the first two months, followed by rifampicin and isoniazid for the following four months, was administered.
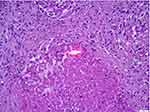 |
Figure 3 Caseified necrotison granuloma (Hematoxcillin&Eosin stain). |
 |
Figure 4 Caseified necrosis in testis. |
Under treatment, patients’ complaints such as fever and night sweats disappeared. Control testicular ultrasound showed a decrease in nodule size. Treatment was completed for six months and stopped.
Discussion
Tuberculosis can affect many organs in the genitourinary region. It affects the testicles at a rate of 0.5% among the genitourinary organs. It is one of the rare forms of extra-pulmonary involvement.8 Since isolated testicular involvement is not a common condition, especially testicular tumor, infarction, and other granulomatous infections should be considered in the differential diagnosis.9 The most important problem that compels the clinician is to perform unnecessary orchiectomies due to difficulties in diagnosis and misdiagnosis.10 Diffuse testicular size, heterogeneous or homogeneous hypoechoic nodular lesions can be observed on ultrasonography.11,12 Testicular biopsy is one of the important methods in the diagnosis. FNAB and cytology can show epithelioid granulomas, and bacilli can be detected by acid-fast staining (ARB). However, ARB positivity is not always. Positivity can be detected in about 60% of tuberculosis cases.13 In addition, testicular USG makes a significant contribution in the diagnosis of TB orchitis. Diffuse, homogeneous / heterogeneous, hypoechoic lesions and nodular enlargements on USG are the features supporting TB. Color Doppler USG contributes to distinguishing testicular TB from other pathologies such as torsion.14,15
ARB could not be examined in our center due to financial insufficiency. In addition, the patient’s history, scrotal USG and FNAB were helpful in the diagnosis, because of TB culture and polymerase-chain reaction (PCR) were not possible. Fever, night sweats in the history, young age of the cases and unilateral testicular involvement suggested testicular TB. In our cases, the caseified necrotizing granuloma stated in the FNAB report was accepted as a definitive diagnosis and treatment was planned. In addition, the improvement of the patient’s symptoms with 6 months of anti-tuberculosis treatment and the disappearance of nodules on Testicular USG strengthened our diagnosis of possible tuberculosis.
Although surgical indication is rarely required in the treatment because of complications, it is possible to effectively treat testicular TB with the quadruple (isoniazid, rifampicin, pyrazinamide and ethambutol). Cure is provided with six months of treatment.16
Conclusion
Without a histological result, the diagnosis of testicular TB may not be possible. In endemic areas where it is not possible to confirm the diagnosis with ARB or culture, the contribution of USG and FNAB is great. Testicular TB should definitely be considered in the presence of unilateral heterogeneous mass, especially in young men with a history of living or traveling in a TB endemic region.
Ethical Approval
Institutional ethical approval was not sought for the publication of the cases.
Consent for Publication
Voluntary consent for publication was obtained from both cases.
Acknowledgments
We thank the urology and pathology teams for their support. Also, microbiologist Dr We would like to thank Serpil DOĞAN for her support.
Funding
No financial support received.
Disclosure
There is no conflict of interest.
References
1. World Health Organization. Tuberculosis; 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
2. Rodriguez-Takeuchi SY, Renjifo ME, Medina FJ. Extrapulmonary tuberculosis: pathophysiology and imaging findings. RadioGraphics. 2019;39(7):2023–2037. doi:10.1148/rg.2019190109
3. Ramírez-Lapausa M, Menéndez-Saldaña A, Noguerado-Asensio A. Tuberculosis extrapulmonar, una revisión [Extrapulmonary tuberculosis]. Rev Esp Sanid Penit. 2015;17(1):3–11. Spanish. doi:10.4321/S1575-06202015000100002
4. World Health Organization. WHO Report 2009. Global Tuberculosis Control: Epidemiología, Strategy, Financing. Geneva: World Health Organization; 2009.
5. Leeds IL, Magee MJ, Kurbatova EV, et al. Site of extrapulmonary tuberculosis is associated with HIV infection. Clin Infect Dis. 2012;55(1):75–81. doi:10.1093/cid/cis303
6. Lakmichi MA, Kamaoui I, Eddafali B, et al. An unusual presentation of primary male genital tuberculosis. Rev Urol. 2011;13(3):176–178.
7. Jacob JT, Nguyen TM, Ray SM. Male genital tuberculosis. Lancet Infect Dis. 2008;8(5):335–342. doi:10.1016/S1473-3099(08)70101-4
8. Al-Hashimi KA, Said UN. Unilateral testicular tuberculosis: an extra-pulmonary manifestation. Cureus. 2021;13(10):e18896. doi:10.7759/cureus.18896
9. Abraham S, Izaguirre Anariba DE, Dua K, Mir M, Ankireddypalli A. A case of testicular tuberculosis mimicking malignancy in a healthy young man. Ther Adv Infect Dis. 2016;3(3–4):110–113. doi:10.1177/2049936116655261
10. Nuwagira E, Yekosani M, Abraham B, Atwine R, Caleb T, Baluku JB. Drug-resistant tuberculosis presenting as a testicular mass: a case report. Int Med Case Rep J. 2021;14:145–149. doi:10.2147/IMCRJ.S300216
11. Turkvatan A, Kelahmet E, Yazgan C, Olcer T. Sonographic findings in tuberculous epididymo-orchitis. J Clin Ultrasound. 2004;32:302–305. doi:10.1002/jcu.20035
12. Jung YY, Kim JK, Cho KS. Genitourinary tuberculosis: comprehensive cross-sectional imaging. Am J Roentgenol. 2005;184:143–150. doi:10.2214/ajr.184.1.01840143
13. Garbyal RS, Sunil K, Kumar S. Diagnosis of isolated tuberculous orchitis by fine-needle aspiration cytology. Diagn Cytopathol. 2006;34:698–700. doi:10.1002/dc.20538
14. Muttarak M, Peh WC, Lojanapiwat B, Chaiwun B. Tuberculous epididymitis and epididymo-orchitis: sonographic appearances. AJR Am J Roentgenol. 2001;176:1459–1466. doi:10.2214/ajr.176.6.1761459
15. Pavlica P, Barozzi L. Imaging of the acute scrotum. Eur Radiol. 2001;11:220–228. doi:10.1007/s003300000604
16. Hadadi A, Pourmand G, Mehdipour-Aghabagher B. Unilateral testicular tuberculosis: case report. Andrologia. 2012;44:70–72. doi:10.1111/j.1439-0272.2010.01097.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
