Back to Archived Journals » Smart Homecare Technology and TeleHealth » Volume 9
Teledentistry Approaches for Dental Assessments and Consultation During the COVID-19 Pandemic
Authors Alotaibi S , Alshehri A
Received 31 March 2022
Accepted for publication 8 September 2022
Published 7 October 2022 Volume 2022:9 Pages 11—25
DOI https://doi.org/10.2147/SHTT.S366239
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Aryya Gangopadhyay
Sarah Alotaibi,1 Ahlam Alshehri2
1Dental Center, Prince Sultan Military Medical City, Riyadh, Saudi Arabia; 2General Directorate of National Health Economics and Policies, Saudi Health Council, Riyadh, Saudi Arabia
Correspondence: Sarah Alotaibi, Dental Center, Prince Sultan Military Medical City, Riyadh, Saudi Arabia, Email [email protected]
Introduction: COVID-19 pandemic shows the importance of teledentistry usage to cope with such conditions and to improved the patient access and quality of care. Since dental treatments are highly infectious procedures due to the close proximity to patients required and the extended exposure to aerosols (including water from high- and low-speed handpieces and patients’ saliva and blood). Viruses such as COVID- 19 could be transmitted through these aerosols. As a result dental treatments were limited to emergency only, according to the guidance of the Ministry of Health. This limitation increases the need for means of communication between dental practitioners and patients in order to follow up and provide consultation without direct contact. This could be provided by using telemedicine.
Methods: However, the evidence assessing the effectiveness of this intervention is scars. Therefore, The aim of this study is to conduct mixed method research (quantitative and qualitative) to measure the effectiveness of teledentistry usage during the COVID-19 pandemic. To provide an in-depth understanding of the use of teledentistry in assessing urgent dental cases and providing consultations.
Results: The sample size for the quantitative part of the study (questionnaire) will include Patients that contacts the virtual clinic and attended to their appointments between 28/4/20 and 30/6/20 (the total will be 125 patients), While the sample for the qualitative part will be dentists who used to work in the call center listed in the virtual clinic database.
Conclusion: The outcome of the study is to provide an overview of the use of teledentistry in assessing urgent dental cases and providing consultations and patients satisfaction of the provided service.
Keywords: teledentistry, COVID-19, dental assessment, pandemic, virtual clinic
Background
COVID-19 and Its Impact on Dental Services
Cases of pneumonia with an unknown cause emerged in Wuhan City in China in late December 2019.1 This led the Chinese Centre for Disease Control and Prevention (China CDC) to send a team on December 31, 2019, to help the health authorities in Hubei province and Wuhan city detect the cause of this pneumonia through epidemiologic and etiologic investigations.1 This investigation reported that the cause of pneumonia was a novel coronavirus (SARS-CoV-2) named 2019-nCOV, which differs from MERS-CoV and SARS-CoV and is counted in the family of human coronaviruses.1
Many countries that reported cases of this novel coronavirus subsequently linked them to a history of travel or residency in Wuhan.2 This highly infectious virus was transmitted globally within a very short time; it was announced as a Public Health Emergency of International Concern by the World Health Organization (WHO) on January 30, 2020, after spreading to 18 countries.3 The pneumonia known to be caused by SARS-CoV-2 was renamed “COVID-19” by WHO on February 11, 2020, which is a short name for “coronavirus disease 2019”.2 On March 11, 2020, the WHO declared COVID-19 a pandemic due to the rise in cases to more than 118,000 in 114 countries, with 4000 deaths.4
The first case in Saudi Arabia, detected on March 2, 2020, was a traveler who came from Iran.5 After that, the number of cases steadily rose, consisting mainly of international tourists who had been in direct contact with infected people in their travels. The number of cases continues to rise and, according to the daily updates of the Saudi Centre of Disease Prevention and Control, has reached more than 160,000. The Saudi government was one of the first national governments to apply precautions against the spread of SARS-CoV-2, even before the appearance of the first case, by banning flights coming from China on February 6, 2020.6 Then, on February 27, 2020, international religious tourism was stopped, and the entrances to Makkah and Madinah were subjected to monitoring. The next day, flights were stopped from all countries experiencing a COVID-19 outbreak, thus blocking the entrance of travelers who had visited the affected countries.
One of the most important precautions was limiting dental treatments to emergencies only, according to guidance from the Ministry of Health.7 Dental treatments are highly infectious procedures due to the proximity of dental practitioners and patients and extended exposure to aerosols (including water from high- and low-speed handpieces and patients’ saliva and blood). Viruses such as COVID-19, can be transmitted through these aerosols.8 Both dentistry and other medical practices have generally aimed to restrict patients’ physical attendance as much as possible. This limitation has increased the need for a means of communication between medical and dental practitioners and patients to follow up and provide consultation without direct contact. This has led to the widespread use of telemedicine (TM), a method of delivering healthcare that has been developed using new technologies, such as smartphones, tablets, and laptops.4
Literature Review
An Overview of Teledentistry
Recently, the field of dentistry has seen significant technological innovations. Progress has been made in the development of digital diagnostic imaging services and devices, software for analysis and follow-up, and telecommunication technology.9 Today, the field of dentistry has advanced even further through the use of advanced information technology.10 Improvement to dental practice through the use of new information technology has not only increased the quality of dental patient management but has also made long-distance management possible, offering dental patients partial or complete care even if they live thousands of kilometers away from healthcare centers or qualified dentists.11
The WHO defines telemedicine as
the delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for the diagnosis, treatment and prevention of disease and injuries, research and evaluation and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities.12“(p.10)”
Although telemedicine programs have been developed over a span of 40–50 years, to date, the utilization of this innovation in dentistry has been scarce.13
Teledentistry is a process of networking and sharing digital information in which distant consultations, workup, and analysis are handled by a division of telemedicine concerned with dentistry.11 It involves the consolidation of both dentistry and telecommunications technology to remotely exchange clinical images and information for dental treatment consultation and planning.14 The first use of the term “teledentistry” was in 1997, when Cook defined it as “ … the practice of using video-conferencing technologies to diagnose and provide advice about treatment over a distance”.15
The teledentistry approach was established as a component of the model for dental informatics, which was drafted at a 1989 meeting subsidized by the Westinghouse Electronics Systems Group in Baltimore.16 The focus of the conversation was on how to apply dental informatics in dental practice to improve the delivery of oral health services.16 Teledentistry can be categorized into two forms: real-time consultation and store and forward. Real-time consultation involves the use of telecommunication and a network connection to initiate a remote video or phone call between dental care providers and their patients. Store and forward includes the trading of significant clinical data and static images, such as intraoral and extraoral images and radiographs, which are gathered and saved in a digital form to be shared through the network with other dental practitioners for further consultation and treatment planning.10
Teledentdistry was implemented during the pandemic even by the low income countries in the southeast Asian countries for two key reasons: (1) due to the necessity of lockdown measures at this time that reduced the availability of face-to-face dental practice; and (2) cost effectivity of this method. Although challenges were encountered with the implementation, including internet speeds, technical issues and political clearance, many clinics in Southeast Asian countries started to apply teledentistry in order to provide diagnosis and follow ups for their patients.17
A notable difference between high and low-income countries was that developed nations such as the US had already adopted and applied teledentistry prior to the pandemic. The rationale was to increase accessibility to health care services and provide services to rural and remote areas.18
Teledentistry in Saudi Arabia
A qualitative shift in the healthcare sector is emphasized in Saudi 2030 Vision, which outlines several strategies for the provision of better health services. The plan’s priority is to enhance the quality of healthcare services by improving access to medical services and reducing wait times. In response, all government sectors that provide healthcare are working to implement these goals by applying telemedicine, including teledentistry. [removed for blind peer review]
It is a healthcare facility under the Ministry of Defense that provides healthcare services to numerous Saudi citizens. It was one of the first facilities to apply telemedicine to facilitate access to health services starting in 2004.
The COVID-19 pandemic highlights the importance of using teledentistry to cope with such crises and improving patient access and quality of care. However, the evidence assessing the effectiveness of this intervention remains sparse. Therefore, our research aims to explore a variety of evaluation dimensions in relation to teledentistry services.
Project Objectives
Aims and Objectives
Aim
The aim of this study is to conduct mixed methods research to discover teledentistry approaches used during the COVID-19 pandemic for dental assessments and consultations.
Objectives
The objectives of this study include 1) exploring teledentistry approaches and 2) evaluating its effectiveness during the COVID-19 pandemic for both service users and providers.
Research Design
Search Strategy
Data Collection and Analysis
The data for this study was collected through the following steps and procedures. We started by mapping the available methods of communication with patients using any kind of teledentistry during COVID-19 to formulate an overall picture of the provided services before beginning the study.
This study required a wide range of data collection methods to achieve the required level of depth. Therefore, the mixed methods approach was used. The qualitative methods for the research consisted of interviewing service providers in person (ie, dentists who worked in the call center listed in the virtual clinic database). The interviews were semi-structured since the research was exploratory in nature, with the purpose of identifying the teledentistry approaches used (the interview questions are provided in the Supplementary Materials). To ensure the appropriateness of the questions, we conducted a pilot study on a subsample of three participants.
To evaluate the results, a modified version of the Donabedian framework19 developed by Reeve et al20 was used. This modified framework was based on the work of Wakerman and Humphreys21 and aimed to represent the three key aspects of care (ie, structure, process, and outcomes) according to two categories: the performance of the service and the main requirements that are needed for sustainability and improvement in healthcare outcomes.20
Additionally, the quantitative method of research was applied to measure service users’ (patients who call and attend the dental center) satisfaction, based on data contained in the dental virtual clinic’s database between April 28, 2020, and June 30, 2020. In doing this, an approved tool was used, namely, the Short Questionnaire for Out-of-Hours Care (SQOC), which was originally designed by McKinley et al22 and then adjusted and re-tested by Salisbury to provide greater ease of use.22 The methods of communication were also assessed for potentially necessary enhancements and to determine the impact of using teledentistry to reduce unnecessary visits during the pandemic.
Questionnaire Validation
The questionnaire used in our study has been proven to be reliable and valid for routine service use.22 Before we employed the questionnaire, it was translated, and two bilingual researchers validated the translated version of the questionnaire.
Methods
Methodology
Identifying the Research Question
The research question was the following: What are the teledentistry approaches in performing dental assessments and consultation during the COVID-19 pandemic?
Sample Size and Target Population
The study sample consisted of patients who had contacted the virtual clinic and attended appointments between April 28, 2020, and June 30, 2020 (ie, 125 patients) and dentists who worked in the call center, as listed in the virtual clinic database, who were able to provide an overview of their experience.
Pilot Study
A pilot study with three participants was conducted to validate the qualitative method and ensure that the questions were adequate and measurable.
Inclusion Criteria
The inclusion criteria were as follows:
- Patients who were eligible to receive dental treatment in. [removed for blind peer review] and who provided consent were interviewed.
- Patients who contacted dental call centers in the period April 28, 2020, to June 30, 2020.
- Patients who attended their scheduled appointment (to provide an overview of the whole process).
- Staff that provided any type of teledentistry service.
- Individuals who were 18 years or older.
Exclusion Criteria
The exclusion criteria employed in the study were the following:
- Patients or staff with no experience of teledentistry.
- Patients younger than 18.
- Patients who contacted the call center but did not attend an appointment in the period from April 28, 2020, to June 30, 2020.
Outcomes
The outcomes of the study included providing an overview of the use of teledentistry in terms of assessing the urgency of dental needs, providing consultations, and evaluating patients’ satisfaction with the provided service.
Results
Service Overview
The teledentistry service was created as an initiative to confront the COVID-19 pandemic. There was no budget allocated for it, and only the available resources were used. Four telephone lines were allocated to the public line service of Medical City. Since it was a new service, it was announced to prospective users through a voice message, and recordings were made to educate dental patients about preventive precautions. Relevant statements were made on the patient portal, and phone messages were sent to all dental center patients with all service details, such as the phone number and extension. Moreover, posters and roll-ups were made and distributed at the entrances of the center.
Four assigned dentists answered the telephone, and they had a clear schedule of shifts to cover the need for service. These dentists were trained virtually about the service, including the service delivery plan, such as the assessment and pain scoring system, which was built based on the Ministry of Health guidelines, and a list of on-call dentists’ information for all specialties was shared. The dentists followed up periodically, and forms were manually completed to assess productivity.
According to the evaluation, the patients were categorized as those needing emergency treatment, those needing appointments, and those requiring medical prescriptions. The patients who needed emergency treatment or booked appointments were asked if they had any symptoms of COVID-19 and provided with precautionary measures that they should follow, such as wearing a mask and passing through the visual triage. Furthermore, they were provided the clinic’s number so they could go directly there without needing to wait. If a patient exhibited symptoms of the virus or was a confirmed case, they would be received as an emergency case in a clinic with all the necessary precautions being taken.
Those who needed a prescription had it delivered to them through a team of volunteers or received it from the center through strict precautionary procedures. Three days after using the service, follow-up was provided either at the center or with the patient at home. After the return to regular work and the end of restrictions, the telephone lines designated to serve the dental patients were gradually reduced from four to one, due to the lack of need.
Current Status
The “Hollat” service is a telephone line serving all beneficiaries of the. [removed for blind peer review] medical services throughout the Kingdom of Saudi Arabia. The service is used for booking appointments, including dental center ones. Because the service providers do not know the details of the dental center’s appointments, a ticket is issued for patients’ affairs, who will communicate with the dental center instead of booking the appointment. This shows the need to return to the service of the virtual clinic, and it is activated such that the first appointment for patients is made at the virtual clinic to make the first diagnosis and to direct the patient to a specialist as needed. Patients receive a phone message telling them that the dentist will contact them at a specified time. If the condition is an emergency, they are directed immediately to the emergency clinic and notified of their working hours. If it is the patient’s first visit, a preliminary diagnosis appointment is booked, as a section would have been allocated for patients’ initial diagnosis in the virtual clinic.
Those in charge of the clinic are consultants and have the authority to transfer the patient to the specialist needed after the initial examination. The consultant refers a list of patients’ names for which the specialty is indicated to the specialist’s receptionist. This person, in turn, communicates with the coordinators (there is a list of contact information for the coordinators of all specialties).
To calculate each dentist’s productivity, special codes were developed for the virtual clinic. The virtual attendance and the services provided in the Hospital information system (HIS) were also added for this purpose.
Quantitative Design and the Short Questionnaire for Out-of-Hours Care
Study Population
The patients who contacted the virtual clinic and attended appointments between April 28, 2020, and June 30, 2020, totaled 125. All patients were contacted, and based on the initial conversation, 60 were excluded from the sample for several reasons, including the following: First, 42% (25) of them did not remember the phone conversation; 33% (20) did not use the service; 16% (10) were called to book an appointment with their orthodontist; and 8% (5) did not answer the call (Figure 1).The remaining 65 respondents completed the questionnaire.
 |
Figure 1 Modified PRISMA chart of the sample selection for service users.34 Notes: *42% (25) of them did not remember the phone conversation; 33% (20) did not use the service; 16% (10) were called to book an appointment with their orthodontist; and 8% (5) did not answer the call. |
Variables
The SQOC questionnaire evaluates patient experience of care through multiple-choice questions under titled sections. The first section is about the patients’ call initiation, age, and gender (Table 1). The second section pertains to the services received (Table 2), and the third section is to evaluate the satisfaction of the patients and provide a room for their recommendations to improve service in the future (Table 3).
 |
Table 1 Study Characteristics |
 |
Table 2 Service Provided to the Patient |
 |
Table 3 Evaluation of Patient’s Satisfaction |
About the Patient
- Gender: The distribution of gender was roughly equal, with 51% female and 49% male (Figure 2).
- Age: Most responses (70%) came from those aged 18 or older (Figure 3).
- Call initiator: Over all, 57% of the calls came from the patients themselves, while 43% came from the patients’ parents.
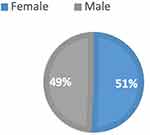 |
Figure 2 Pie chart showing gender distribution of the sample. |
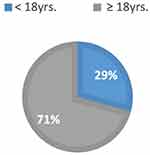 |
Figure 3 Pie chart showing age distribution of the sample. |
About the Service Received
Twelve percent of the respondents claimed that they received advice over the telephone immediately. The majority of the respondents (88%) needed to be seen in the dental clinic. In terms of the way the call was handled, 54% were happy with it, 45% claimed that they preferred to be seen in the clinic, and only 1% complained that they should have been given better advice.
The Respondent’s Satisfaction
The third question in the questionnaire was to assess the respondent’s satisfaction with the service based on a scale (very dissatisfied, dissatisfied, neutral, satisfied, and very satisfied (. Almost half the respondents (49%) were very satisfied with the way they were able to get through on the telephone. However, there was clear dissatisfaction with the way the initial phone call was handled (21%) and with the explanation the doctor or nurse gave them about their problem (35.4%). It is noteworthy that 66% of the responses were neutral regarding the advice or treatment suggested during the call or service. Very satisfied (32.3%) and satisfied (29%) accounted for the bulk of responses regarding the overall satisfaction of the service.
Recommendation to Improve the Service
Most of the comments focused on the need to increase care capacity (ie, availability of the appointments).
Qualitative
The Interview Questions Were Divided into Two Tiers
Service performance and essential requirements for the sustainability and the improvement of the service outcomes. This division was based on the criteria that were used to evaluate the healthcare service based on Donabedian’s (1988) framework and modified by the research team from Fitzroy Valley, who took the same three areas and divided them into the two tiers.
The interviews were semi-structured. Some questions that emerged were related to patients’ privacy. For example, there were video calls and pictures that were sent to the clinician, including concerns about where these data should be stored. In this research, we interviewed 12 clinicians out of the 46 who worked in the service during the first 3 months. This number was found to be enough based on information repetition and data saturation. In the next section, the data is presented according to the questions in the two segments of the questionnaire.
Service Performance
Regarding this section, we asked about three aspects of the service: the clinical aspect, related to the scale used to assess pain; the patient aspect, which is their ability to describe their cases; and the technical aspect of the service. How the three aspects affected service performance was also investigated. In the following, the responses to each question is discussed separately.
First Question
What were the scales used to assess the urgency of the cases? Respondent #1ʹs response was that the patient was asked several questions, and these were enough to assess pain levels. Respondents #3 and #12 mentioned that there was a scale from 0 to 3 (0 = no pain, 1 = mild pain, 2 = moderate pain, and 3 = severe pain, such that the patient cannot sleep). Respondent #4 mentioned that there were three questions. Each question was assigned one point, and if the patient obtained three points, they needed to come to the clinic. The rest of the participants commented that there were questions about the kind of pain, the onset of the pain, and the duration of the pain. Respondent #2 also mentioned that for a better assessment, respondents had access to the DORTAL, an electronic page that allows doctors to access patient files, their medical histories, and their medications. This allowed the doctors to identify if the patient had any allergies and to insert their prescriptions on the same page if antibiotics or analgesics were needed. The main scale in most cases assessed whether the patient was unable to sleep because of the pain. Also, if the patient had finished the prescribed antibiotic or analgesic but was still in pain, they were asked to come to the clinic.
Second Question
To what extent were patients capable of describing their symptoms?
There was not that much difference in the responses to this question. Most participants said that the patients were able to describe their symptoms and that it was therefore easy to identify the ER cases from the others.
Third Question
Describe your experience regarding the technical aspects of the service?
Most of the responses suggested that the technical aspect was good and generally worked well. However, there were a few comments regarding the problematic distribution of calls at the beginning of the service, as well as a technical issue that caused many service users to wait for a long time before the service provider could answer their call. Another comment was related to the need for better technology: Participants suggested that it would be better if there were a system similar to the one used in banks that shows the ID of the caller and accesses their information before answering the call. Another comment suggested having a preliminary automated message informing the service users that they will soon be connected to a doctor and that a virtual assessment session would start.
The next section provides the answers to the questions that occur in the second section.
Essential Requirements for Sustainability and the Improvement of Service Outcomes
First Question
How do you see the future of teledentistry in screening patients and providing an initial diagnosis?
Respondent #1 said that it could be helpful to provide an initial diagnosis, but not in all specialties. For example, in orthodontics, it is hard to diagnose using teledentistry. Respondent #8 also did not think that the service would be beneficial in the case of orthodontic dentistry, in which case, the patient needs to be in the clinic to be able to provide a proper diagnosis. Respondent #5 mentioned that teledentistry could be helpful in follow-up with patients but never in providing an accurate diagnosis. However, Respondents #2 and #11 thought that teledentistry could be helpful in providing an initial diagnosis. Respondents #3, #4, and #6 believed that the service could be very helpful in providing diagnosis, but only if the patient was educated properly before calling. Most of the patients called to make appointments in the clinic, and they were not even aware that they would be talking to a doctor. Even after the service was explained to them, they only wanted to be seen in the clinic. The remaining respondents thought that telecommunication could be very helpful, maybe not for diagnosis, but for differentiating ER patients from those who just wanted a regular appointment. Moreover, it was suggested that teledentistry could ease patients’ communication with doctors when they have questions about treatment, especially if they live in remote areas.
Second Question
How do you find the telecommunication with the patients?
Approximately 80% of the respondents found that telecommunication with patients was quite smooth. Even in situations with elderly patients or those with mental illness, their family members helped in communication. The remaining respondents said that it depended on the patient and that half were cooperative while half were not.
Third Question
Would you prefer using video calls or texts for virtual consultations, and why?
Respondents #2 and #12 said that they did not prefer using video in communication with the patients and that this may not be comfortable for some patients, due to their cultural background. Regarding text communication, they mentioned that they preferred verbal communication. Respondent #10 thought that verbal explanation was enough. The remaining respondents said that it would be better to have video calls and photos of the cases. Respondent #3 mentioned that when a patient reported swelling, it was difficult to know if antibiotics were needed, and having a video call or photo would help in this regard. Respondent #3 thought it was a good idea but preferred sending photos over video calls, indicating that the patients did not use telecommunication in their normal appointments. Respondent #6 also preferred having a photo of the case over video calls. Respondent #7 said that she preferred having video calls or photos because orthodontic cases usually needed a visual diagnosis. Moreover, Respondent #9 mentioned that she already asked some patients to send her a photo of the problematic area to determine if they needed to come to the ER or not.
Fourth Question
What do you recommend for the service in general?
Respondents #2 and #12 mentioned that it was a temporary service for the duration of the pandemic and that it was intended mainly to reassure patients but will not be that useful when the pandemic was over. Respondent #3 said that the service would be great if there were a receptionist available to receive the calls and gather patient information beforehand and to set up appointments when needed with the assessing doctor. She also mentioned that there should be a proper announcement of the service in the hospital. Moreover, she suggested having easier communication with the coordinators of each specialty in case consultations or referrals were needed. Respondent #4 mentioned that patients should be educated about the service and that a specific time should be scheduled beforehand so that both the patient and doctor are prepared for the session. The explanation in every call took time because the patients were calling to ask for appointments and were not prepared for a virtual appointment. Respondent #6 said that the main issue was that the computers sometimes did not work properly, which meant that the doctors did not have access to the patient information, thus complicating the assessment process and the insertion of prescriptions. She would prefer if there were a coordinator to answer the calls and transfer only the calls that need assessments. Respondent #9 said that she would like greater smoothness in the process of prescription entry and medication delivery. The remaining respondents expressed a desire for more video calls or a texting service that would allow sending photos of the cases.
Discussion
The pandemic has brought attention to the importance of teledentistry. However, teledentistry is not a new concept, as it was started by the Westinghouse Electronics Systems Group in Baltimore in 1989.16 However, it initially only involved the linking of dental informatics and dental practice.16 Nevertheless, it was helpful to dental public health professionals and patients in that it reduced the financial expenses of location displacements and minimized wait times in dental care.23 This reduction in wait times also serves to increase access to dental treatment for people who are disadvantaged. Teledentistry approaches can provide better services to these areas by facilitating consultations with doctors from different specialties, who are usually not available in these locations.23 Therefore, a major benefit of this health service is in creating greater equity by reducing wait times and providing better care to underserved people. Moreover, there are several issues that can be addressed by using teledentistry approaches, such as cost, quality of dental care, and efficacy.24
Phone calls became the primary approach for teledentistry during the pandemic when it became difficult to serve patients in clinic. This approach requires less maintenance and encounters fewer technical issues.24 It also does not require staff training to use the tools and can be used by patients of different ages. According to Ben-Omran et al,25 phone calls and text messages are acceptable approaches to use with older adults. However, the service providers reported that there was variation in how the older and younger staff experienced the technology. The older ones thought it was sufficient, while only a few in the younger group agreed; most of them felt it would be better to have a system that gives patients’ information before the call is answered. In addition, there were comments regarding call distribution and how patients were kept waiting for long on the line, although there was a free service provider. Moreover, most of the interviewed service providers mentioned that they would prefer a better approach in providing the assessment or initial diagnosis, whether it was video calls or a system that enables patients to send photos. While phone calls and text messages are simple teledentistry approaches, there are more complicated methods, such as live monitoring devices that take live photos and transfer them, as well as intraoral cameras in televideoconferencing.25 These advanced technologies could improve oral healthcare services, including assessments and initial diagnosis, as well as aid referrals when needed, thus helping to alleviate the problem of limited access to dental services.
In the following section, the results are evaluated using the modified framework that was developed for Fitzroy Valley by Reeve et al.20 The framework consists of two aspects: service performance and essential requirements for the sustainability and the improvement of the service outcomes. To evaluate service performance and sustainability, certain indicators were needed. Therefore, Elmore’s indicators for service performance and sustainability were used in this study.26 Based on Elmore’s framework, the indicators of adequate service performance include accessibility, appropriateness, effectiveness, responsiveness, continuity, and efficiency. The indicators for service sustainability are workforce, linkages, infrastructure, funding governance, management, and leadership.26
Service Performance
The six indicators mentioned above are assessed based on the answers provided in the service users’ questionnaire and the service providers’ interviews.
The first parameter is service accessibility, which is evaluated by the service users’ answers to the question about the ease of getting through on the telephone. In all, 49% of participants were satisfied with the experience and mentioned that there was no long wait time, which provided more access time for the none served in the clinic. Most importantly, the service increased patients’ accessibility during the pandemic when clinics were closed and there was no other access to dental services. Moreover, they needed access to the emergency clinic when needed, since all the participants in this study had appointments after they called the service and went to the clinic based on the service providers’ referrals. Moreover, the accessibility indicator can be measured in terms of the service provided to people who live in remote areas, and this was clearly provided in the teledentistry service. The service also provided easier access for people who wanted to ask their doctors questions or have a simple consultation; they did not have to wait for a formal appointment in the clinic to do so. The main goal of using teledentistry in the 1994 Ministry of Defense’s project (total dental access) in the US Army was to increase access to dental care.23
The second indicator is appropriateness, which can be assessed according to the Elmore criteria that the service should have available female GPs as well as allied health services. Clearly, these were available in this service since 80% of the service providers were females, and there were available health services, such as a pharmacy and prescription delivery. Moreover, there was a proper registry of the patients that used the DORTAL management of cases and referrals when needed.
The third indicator is effectiveness, which mostly concerns coverage for all ages and a wide range of screening. The teledentistry service was provided for all ages and types of patients seeking oral healthcare. In this study, 91% of the service providers said that they found the service beneficial in providing screening and initial diagnosis. Some of them asked for modifications, and some specified specialties where the service could be used for assessment purposes, but the majority agreed that it was useful in providing screening. Furthermore, Alabdullah and Daniel argued that teledentistry is comparable to clinical oral screening, particularly when it is used with people who live in areas with poor access to healthcare, such as in rural areas.27 Moreover, a randomized controlled study used to compare the effectiveness of using teledentistry and traditional examination in detecting early childhood caries (ECC) in preschool low-income children in Rochester, NY, suggested that using teledentistry in screening was similar to traditional examinations. Additionally, the study found that showing printout photos of dental cavities to the parents using the teledentistry service encouraged them to make dental appointments for their children.28
The fourth indicator is responsiveness. The service appears to be responsive to public and cultural needs since the main purpose of teledentistry services is to serve the public during the pandemic without risking exposure to infection. The teledentistry service in general was developed to serve those who did not have access to oral healthcare services for various reasons.29 Regarding the community input into the service planning, the questionnaires helped to identify the patients’ satisfaction and improve the provided service. Moreover, according to results from the service provider interviews, there were technical issues at the beginning of the service that were solved later after they were reported.
The fifth indicator is the continuous nature of the service, which can be measured by using a healthcare needs assessment. This is the main role of the teledentistry service because it provides easier communication between dental healthcare professionals and patients in terms of assessing their needs. Regarding the follow-up appointments for the patients in this study, there were no recall appointments because the service was mainly intended to reassure the patients and filter ER patients. However, according to the majority of the service providers in this study, teledentistry could be used in follow-ups with patients and recall visits, and several studies have advocated the use of teledentistry in recall and follow-up appointments.30,31
The sixth indicator, efficiency, is based on the service availability in the insurance claim system and the electronic recording of the virtual session. Insurance claims are not applicable since the service was implemented in a governmental tertiary hospital where the service is free for hospital affiliates; therefore, no insurance claim was needed. However, regarding the recording, this was provided for all the virtual sessions, and prescriptions were entered through DORTAL using the patients’ medical numbers.
Service Sustainability
There were five indicators in the assessment of service sustainability, which were applied to the results of the research patient questionnaire and the interviews with service providers. First, according to the workforce index when the service started, 46 dentists were assigned to respond to the patients. They had virtual training on the service and received all the needed documents. The dentists had a clear schedule of shifts to cover the needs for the service. They were followed up periodically, and forms were required to be completed to assess productivity.
The second indicator was linkage, which in the dental center experience can be justified according to two points. First, the services guideline was built on the Ministry of Health’s policies and procedures to cope with and conquer the pandemic. Second, the telephone lines allocated to the dental virtual clinic center were linked to the mainstream system, which covers all the outpatient services at. [removed for blind peer review].
The third indicator assessed the service (teledentistry) infrastructure of the dental center in. [removed for blind peer review] of Medical Services. There were four phone lines dedicated to the dental center. A clear work plan was developed for the service in terms of providers, guidelines, lists of doctors on duty for each department, and referral methods. The center was also equipped with all the necessary precautions if patients needed to attend the clinic in emergency cases regarding the patient’s path to reach the clinic without waiting. There was a visual triage at the entrance to ensure that patients were clear of COVID-19 symptoms, preparations to receive a positive or suspected case and provide a particular path, and a negative pressure room. Moreover, in dispensing medicines, a specific approach was determined for patients to follow in receiving their medication. In addition, a team of volunteers delivered medication to some patients to reduce their exposure to infection.
The fourth indicator, assessing, was related to whether there was any funding allocated to a service. There was no additional funding of this service, only redirection or utilization of the available budget at the dental center. Notably, in a published report assessing several study cases of teledentistry programs, the lack of funding was identified as one of the main challenges.32 However, teledentistry might be a cost-effective key in delivering dental care for both providers and patients;32,33 for instance, in lowering the costs spent on the screening sessions.
The fifth indicator assessing service sustainability was governance and leadership. There was complete awareness and response to the pandemic in The Medical City. The authority was given to each department to take the necessary steps to facilitate services and continue providing care in similar circumstances, which was considered as the internal governance of Medical City. Accordingly, a team from the dental center under the guidance of the center leadership performed the necessary work to develop a teledentistry service that provided detailed guides to service providers and worked to educate patients about the new service by placing advertisements at the entrances of the center and through phone messages or the patient portal.
Limitations of the Study
It is difficult to generalize the findings of this study due to its context specificity and the small sample size in its qualitative research segment. Moreover, the Short Questionnaire for Out-of-Hours Care (SQOC) led to some doubts regarding the ability to measure health care quality since it primarily assessed patient satisfaction and not the patients’ experiences.22 However, the use of other patient experience questionnaires is not feasible in this study due to its complexity and length.22
Conclusion
This mixed methods (qualitative and quantitative) research was conducted to evaluate the effectiveness of using teledentistry in the dental center of a tertiary hospital to assess urgent cases and provide consultations during the COVID-19 pandemic. It was intended to provide a thorough understanding of teledentistry service usage at that time.
The data was collected using the mixed methods approach, and from the documentation of the service performance provided by those in charge of the service monitoring, different sources were used to provide an overview of the teledentistry service usage from various perspectives. The Short Questionnaire for Out-of-Hours Care (SQOC) was used to measure the patients’ satisfaction to collect quantitative data, and semi-structured interviews were carried out with 12 staff members to collect qualitative data regarding their perspectives and experiences of service performance.
To enable a proper evaluation, a modified form of the Donabedian framework was used, which was developed by Reeve et al, based on the work of Wakerman and Humphreys.20,21 This framework was divided into two tiers: the performance of the service and the main requirements needed for the sustainability of and improvements to healthcare outcomes. Moreover, to provide a broad analysis of the two tiers of the framework used, specific indicators were required; therefore, Elmore’s indicators were used.
Based on the study’s data analysis, teledentistry usage in assessing urgent cases and providing diagnosis appeared to be effective. However, the approaches used may affect the potential usefulness of the service in terms of whether phone calls or more advanced technology is used.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
2. Kwok KO, Li KK, Chan HH, et al. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. Infect Dis. 2020. doi:10.1101/2020.02.26.20028217
3. Cascella M, Rajnik M, Aleem A, et al. Features, evaluation, and treatment of coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2021.
4. Matusitz J, Breen G-M. Telemedicine: its effects on health communication. Health Commun. 2007;21(1):73–83. doi:10.1080/10410230701283439
5. MOH News. MOH reports first case of coronavirus infection. Moh.gov.sa; 2020. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-03-02-002.aspx.
6. Arab News. Saudi Arabia bars travel to China amid coronavirus; 2020. Available from: https://www.arabnews.com/node/1623851/saudi-arabia.
7. Ministry of Health. MOH dental emergency guidelines for Covid19; 2020. Available from: https://www.moh.gov.sa/Ministry/MediaCenter/Publications/Documents/MOH-Dental-emergency-guidline.pdf.
8. Nejatidanesh F, Khosravi Z, Goroohi H, Badrian H, Savabi O. Risk of contamination of different areas of dentist’s face during dental practices. Int J Prev Med. 2013;4(5):611–615.
9. Clark GT. Teledentistry: what is it now, and what will it be tomorrow? J Calif Dent Assoc. 2000;28:121–127.
10. Bhambal A, Saxena S, Balsaraf SV. Teledentistry: potentials unexplored. Int J Oral Health Dent. 2010;2(3):1–6.
11. Mihailovic B, Miladinovic M, Vujicic B. Advances in telemedicine: applications in various medical disciplines and geographical areas. Chapter 11, Telemedicine in dentistry (Teledentistry); 2011:215–230.
12. World Health Organization. A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics. Geneva: World Health Organization; 1997:39. Report No.: WHO/DGO/98.1.
13. Subbalekshmi T, Anandan V, Apathsakayan R. Use of a teledentistry-based program for screening of early childhood caries in a school setting. Cureus. 2017;9(7):e1416. doi:10.7759/cureus.1416
14. Yoshinaga L. The use of teledentistry for remote learning applications. Pract Proced Aesthet Dent. 2001;13:327–328.
15. Fricton J, Chen H. Using teledentistry to improve access to dental care for the underserved. Dent Clin North Am. 2009;53:537–548. doi:10.1016/j.cden.2009.03.005
16. Chen JW, Hobdell MH, Dunn K, Johnson KA, Zhang J. Teledentistry and its use in dental education. J Am Dent Assoc. 2003;134:342–346. doi:10.14219/jada.archive.2003.0164
17. Marya A, Venugopal A, Karobari M, Messina P, Scardina G, Subramanian A. The exponential rise of teledentistry and patient-oriented protective measures in Southeast Asian dental clinics: concerns, benefits, and challenges. Int J Dent. 2021;2021:1–6. doi:10.1155/2021/9963329
18. Nichols K. Teledentistry overview: United States of America. J Int Soc Telemed eHealth. 2019;7. doi:10.29086/JISfTeH.7.e9
19. Donabedian A. The quality of care: how can it be assessed? JAMA. 1988;260(12):1743–1748. doi:10.1001/jama.1988.03410120089033
20. A comprehensive health service evaluation and monitoring framework. Elsevier Enhanced Reader; 2020. Available from: https://reader.elsevier.com/reader/sd/pii/S0149718915000932?token=D88BFC0D859E06E4723FDA41E8A9BCB8439A2D6142FF9F3F441F0D5215E29CF20C550F62109918DEA97B3A3C77D6BDB0.
21. Wakerman J, Humphreys JS. Sustainable primary health care services in rural and remote areas: innovation and evidence. Aust J Rural Health. 2011;19(3):118–124. doi:10.1111/j.1440-1584.2010.01180.x
22. Salisbury C, Burgess A, Lattimer V, et al. Developing a standard short questionnaire for the assessment of patient satisfaction with out-of-hours primary care. Fam Pract. 2005;22(5):560–569. doi:10.1093/fampra/cmi050
23. da Costa CB, da Peralta FS, Ferreira de Mello ALS. How has teledentistry been applied in public dental health services? An integrative review. Telemed E-Health. 2019;26(7):945–954. doi:10.1089/tmj.2019.0122
24. Bhambal A, Saxena S, Balsaraf SV. Teledentistry: potentials unexplored! J Int Oral Health. 2010;2(3):6.
25. Ben-Omran MO, Livinski AA, Kopycka-Kedzierawski DT, et al. The use of teledentistry in facilitating oral health for older adults: a scoping review. J Am Dent Assoc. 2021;152:998–1011.e17. doi:10.1016/j.adaj.2021.06.005
26. Tham R, Humphreys J, Kinsman L, et al. Evaluating the impact of sustainable comprehensive primary health care on rural health: evaluating rural primary health care. Aust J Rural Health. 2010;18(4):166–172. doi:10.1111/j.1440-1584.2010.01145.x
27. Alabdullah JH, Daniel SJ. A systematic review on the validity of teledentistry. Telemed J E-Health. 2018;24(8):639–648. doi:10.1089/tmj.2017.0132
28. Kopycka-Kedzierawski DT, Billings RJ. Comparative effectiveness study to assess two examination modalities used to detect dental caries in preschool urban children. Telemed J E Health. 2013;19(11):834–840. doi:10.1089/tmj.2013.0012
29. Daniel SJ, Kumar S. Teledentistry: a key component in access to care. J Evid Based Dent Pract. 2014;14:201–208. doi:10.1016/j.jebdp.2014.02.008
30. Watfa MO, Bernfeld NM, Oren D, et al. Rapid implementation of teledentistry during the Covid-19 lockdown. Adv Oral Maxillofac Surg. 2021;2:100031. doi:10.1016/j.adoms.2021.100031
31. Suter N. Teledentistry applications for mitigating risk and balancing the clinical schedule. J Public Health Dent. 2020;80(S2):S126–31. doi:10.1111/jphd.12421
32. Langelier M, Rodat C, Moore J. Case Studies of 6 Teledentistry Programs: Strategies to Increase Access to General and Specialty Dental Services. Rensselaer, NY: Oral Health Workforce Research Center, Center for Health Workforce Studies, School of Public Health, SUNY Albany; 2016.
33. Khau K, Nguyen H. Teledentistry: an innovative workforce model for dental hygienists; 2020. Available from: https://scholarscompass.vcu.edu/denh_student/20/?utm_source=scholarscompass.vcu.edu%2Fdenh_student%2F20&utm_medium=PDF&utm_campaign=PDFCoverPages.
34. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
