Back to Journals » International Medical Case Reports Journal » Volume 14
Takotsubo Cardiomyopathy Associated with High-Grade Atrioventricular Block and Ventricular Fibrillation: A Case Report
Authors de Santana PH, Pedreira FA, Soares PR, Scudeler TL
Received 25 April 2021
Accepted for publication 7 July 2021
Published 9 August 2021 Volume 2021:14 Pages 523—527
DOI https://doi.org/10.2147/IMCRJ.S317445
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ronald Prineas
Supplementary Video of the Case Report paper “Takotsubo cardiomyopathy associated with high-grade atrioventricular block and ventricular fibrillation: a case report” to be published in the open access journal International Medical Case Reports Journal
Views: 520
Pedro Henrique de Santana, Fábio Américo Pedreira, Paulo Rogério Soares, Thiago Luis Scudeler
Emergency Department, Instituto do Coração (InCor), Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil
Correspondence: Thiago Luis Scudeler
Instituto do Coração (InCor), Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, Avenida Doutor Enéas de Carvalho Aguiar 44, AB, Sala 114, Cerqueira César, São Paulo, 05403-000, Brazil
Email [email protected]
Abstract: Takotsubo cardiomyopathy (TCM) is a condition characterized by reversible left ventricular dysfunction. TCM usually has a good prognosis but, in rare situations, it can be associated with life-threatening arrhythmias. We report a case and the management of TCM with a high-grade AV block and QT prolongation followed by ventricular fibrillation.
Keywords: takotsubo cardiomyopathy, high-grade atrioventricular block, ventricular fibrillation, permanent pacemaker
Introduction
Takotsubo cardiomyopathy (TCM) is a form of nonischemic cardiomyopathy characterized by reversible changes in left ventricular function, especially in the mid-apical segments.1 The presence of arrhythmias in patients with TCM is uncommon, and high-grade AV block is very infrequent.2 However, the development of arrhythmias in a patient with TCM is associated with high morbidity and mortality.2 Although TCM usually reverses completely, AV block may persist and require a permanent pacemaker.3 We describe a case of TCM with high-grade AV block and QT prolongation followed by ventricular fibrillation (VF) cardiac arrest.
Case Presentation
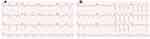
A 56-year-old female with systemic arterial hypertension and grade 2 obesity, regularly using spironolactone 25mg once daily, losartan 50mg twice daily, and amlodipine 5mg twice daily, was admitted to the emergency department with dyspnea and adynamia for 1 day. The patient denied syncope, angina, or palpitations. She reported having experienced an episode of intense emotional stress 2 days before hospital admission. On examination, she had a heart rate of 50 beats per minute, blood pressure of 140/90 mm Hg, arterial oxygen saturation of 97% normal, and absence of clinical signs of heart failure. The electrocardiogram (ECG) on admission (Figure 1A) showed second-degree AV block 2:1, right branch block, left anterior fascicular block, biphasic T wave in DII, DIII, aVF, V1, and V2 and inverted, deep, and asymmetric in DI, aVL, V3, V4, V5, and V6, with QRS duration of 142ms and corrected QT interval of 689ms. Ultrasensitive troponin I was 396 ng/L (normal range, NR<40 ng/L), and BNP was 307 pg/nL (NR<100 pg/mL). Renal parameters, serum electrolytes, and thyroid function tests were within normal limits. Transthoracic echocardiography (Figure 2 and Video) showed a left ventricular ejection fraction (LVEF) of 40%, basal hypercontractility and midventricular and apical ballooning, the most common form of TCM presentation. To expand on the investigation, coronary angiotomography did not show coronary lesions, with a calcium score of zero, and cardiac magnetic resonance (CMR) imaging confirmed the echocardiographic findings and did not show late enhancement (Figure 3). Initially, no transvenous pacemaker was indicated, because the patient was stable, asymptomatic, and had adequate ventricular escape (50 bpm). On the same day, the patient experienced a VF cardiac arrest, and promptly underwent defibrillation with 200 joules and cardiopulmonary resuscitation maneuvers following the Advanced Cardiovascular Life Support protocol. She returned to spontaneous circulation after 3 minutes, with immediate recovery of consciousness. The post-cardiac arrest ECG showed the same pattern as that at the beginning of hospitalization. The patient did not receive tracheal intubation or sedo-analgesic drugs. Laboratory tests after cardiac arrest did not reveal electrolyte abnormalities. The patient underwent temporary pacemaker implantation, maintaining hemodynamic stability, without the need for vasoactive drugs. Because the high-grade AV block did not revert even after 14 days, the patient underwent a dual chamber permanent pacemaker implantation (DDD). On the 18th day, a transthoracic echocardiogram follow-up showed normalization of left ventricular wall motion, with an ejection fraction of 52%; therefore, the patient was discharged from our hospital. ECG at hospital discharge showed complete resolution of T wave inversions and shortening of the QT interval (Figure 1B). At 1-year follow-up, ECG with pacing-off revealed the persistence of high-grade AV block but with a normal corrected QT interval.
Discussion
TCM was first described in 1990 by Sato et al4 and is characterized by transient left ventricular dysfunction, with clinical, electrocardiographic, and laboratory characteristics similar to those of acute coronary syndrome. The syndrome occurs predominantly in postmenopausal women1 after an episode of physical or psychological stress. Its pathophysiology is not yet fully understood, but excess catecholamines have been postulated to be central to the pathogenesis of TCM.5
The diagnosis is based on clinical, echocardiographic, and laboratory data. Although this is not a typical description of the syndrome, the patient’s clinical condition follows the diagnostic criteria proposed by the Mayo Clinic in 2008, which include (1) transient hypokinesis, akinesis, or dyskinesis of the left ventricular mid segments with or without apical involvement; the regional wall-motion abnormalities extend beyond a single epicardial vascular distribution; (2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture; (3) new electrocardiographic abnormalities (either ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin; and (4) absence of all of the following: pheochromocytoma, myocarditis, and hypertrophic cardiomyopathy.6
The clinical suspicion was made based on the changes in segmental mobility detected on the transthoracic echocardiogram. This investigation was further developed with the CMR, which confirmed the changes in segmental mobility and the suspicion of TCM. In this sense, CMR also lends itself to the investigation of differential diagnoses, such as myocarditis or even acute myocardial infarction. According to the description by Eitel et al,7 the observation of late gadolinium enhancement allows such differentiation, because it is absent in TCM, intense in acute myocardial infarction (greater than 5 standard deviations above the mean of the intensity of the myocardial signal), and irregular in myocarditis. In some cases of TCM, it is possible to observe myocardial edema in CMR; however, this finding is considered nonspecific.
We opted for coronary tomography instead of coronary angiography to rule out coronary artery disease (CAD), because the pretest probability of CAD for our patient was low and the clinical and echocardiographic diagnosis of TCM was very likely.
ECG is altered in most patients with TCM (>95%) and usually shows ST segment elevation in the precordial leads (81%), ST segment depression, T-wave inversion (usually deep and diffuse), prolongation of the QT interval, and presence of pathological Q waves.8 Arrhythmias have been described as an uncommon complication of TCM and may include ventricular arrhythmia, atrial fibrillation, torsades de pointes, and AV node dysfunction.9 High-grade AV block is rarely found in patients with TCM and has a prevalence of only 2.9%.9 The exact association between AV block and TCM is not clear, but it can be explained by the continual ischemic status due to microvascular dysfunction.10
Our case shows a rare association between AV block and TCM. Although recovery of left ventricular function occurs in most patients, AV block can persist.11 It is difficult to know whether AV block is the cause of or the result of stress-induced cardiomyopathy. Therefore, the best method for managing high-grade AV block associated with TCM remains uncertain. The electrical changes present in this patient (mainly the prolongation of the QT interval) may have favored the outcome for VF (phenomenon R over T). The dramatic evolution to VF suggests that the implantation of a temporary pacemaker in these patients should not be delayed. An implantable cardioverter defibrillator was not indicated because VF can be managed with a temporary approach until recovery of repolarization time and left ventricular function.10 In our patient, we opted for the implantation of a permanent pacemaker on day 14 due to the persistence of AV block. In patients with TCM, time interval pacemaker implantation is not well established.12 In some cases, AV conduction disorder is transient. However, temporary pacemaker implantation for a long time can be associated with several complications, such as perforation of the right ventricle and infections. Long-term follow-up is necessary to verify the resumption of 1:1 AV conduction and, therefore, unnecessary stimulation should be avoided.
In Box 1 you will find the learning points of this case report.
 |
Box 1 Learning Points |
In conclusion, the recognition of AV conduction defects in patients with TCM is important, because they may not resolve and may need an intervention like pacemaker implantation. Such situations are underrecognized but are potentially fatal and need timely management for patient safety.
Abbreviations
TCM, takotsubo cardiomyopathy; ECG, electrocardiogram; NR, normal range; LVEF, left ventricular ejection fraction; CMR, cardiac magnetic resonance; LV, left ventricular; AV, atrioventricular; VF, ventricular fibrillation.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The research protocol was approved by the Ethics Committee of the Instituto do Coração, Universidade de São Paulo. Written informed consent was obtained from the patient for publication of this case report.
Author Contributions
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest.
References
1. Pilgrim TM, Wyss TR. Takotsubo cardiomyopathy or transient left ventricular apical ballooning syndrome: a systematic review. Int J Cardiol. 2008;124(3):283–292.
2. Patil SP, Gonuguntla K, Rojulpote C, Kumar M, Chen KG. Takotsubo cardiomyopathy related complete heart block: a nationwide cohort analysis. Eur Heart J. 2020;41(2):ehaa946–0697.
3. Benouda L, Roule V, Foucault A, Dahdouh Z, Lebon A, Milliez P. Conduction disturbances in takotsubo cardiomyopathy: a cause or a consequence? Int J Cardiol. 2012;159(1):61–62.
4. Sato H, Tateishi H, Uchida T, et al. Takotsubo type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical Aspect of Myocardial Injury: From Ischemia to Heart Failure. Tokyo: Kagaku Hyoronsha; 1990:56–64.
5. Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539–548.
6. Scantlebury DC, Prasad A. Diagnosis of Takotsubo cardiomyopathy. Circ J. 2014;78(9):2129–2139.
7. Eitel I, von Knobelsdorff-brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306(3):277–286.
8. Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or Takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27(13):1523–1529.
9. Syed FF, Asirvatham SJ, Francis J. Arrhythmia occurrence with Takotsubo cardiomyopathy: a literature review. Europace. 2011;13(6):780–788.
10. Inayat F, Virk HUH, Ullah W, Riaz I. Takotsubo cardiomyopathy-related complete heart block and torsades de pointes. BMJ Case Rep. 2017;2017:bcr2016218017.
11. Kodama S, Miyoshi K, Shiga Y, et al. Takotsubo cardiomyopathy complicated by high-grade atrioventricular block: a report of two cases. Exp Clin Cardiol. 2009;14:e35.
12. Le MT, Grimard C, Varenne O, Jakamy R, Rosencher J. Tako-Tsubo cardiomyopathy and high-degree atrio-ventricular block: do we need to wait left ventricular function recovery to implant a pacemaker? Int J Cardiol. 2014;176(2):e56–e59.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.