Back to Journals » International Journal of Women's Health » Volume 11
Swiss gynecologists’ opinions and perceptions concerning the use of intrauterine devices by nulliparous and multiparous women: an online survey study
Authors Zimmermann Y, Viviano M, Yaron M
Received 28 September 2018
Accepted for publication 5 January 2019
Published 6 March 2019 Volume 2019:11 Pages 153—159
DOI https://doi.org/10.2147/IJWH.S189051
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Yaël Zimmermann,1 Manuela Viviano,2 Michal Yaron2
1Faculty of Medicine, University of Geneva, Geneva, Switzerland; 2Department of Obstetrics and Gynecology, Geneva University Hospitals, Geneva, Switzerland
Objective: The aim of this study was to 1) evaluate the Swiss physicians’ attitudes and beliefs on intrauterine device (IUD) use in multiparous and nulliparous women and 2) determine whether the woman’s parity was a factor influencing the gynecologists’ IUD practice.
Material and methods: The Global Survey questionnaire investigating IUD use was modified and adapted to the Swiss guidelines. A link to the online questionnaire was sent to gynecologists practicing in the French- and German-speaking parts of Switzerland. We defined IUD use as frequent whenever it was prescribed by gynecologists for 25% or more out of all women consulting for contraception.
Results: A total of 299/1,696 gynecologists completed the online questionnaire (17.6%). Frequent IUD prescription was found in 72.9% of multiparous and in 11.8% of nulliparous women. The most frequently reported barriers to IUD use in nulliparous women were as follows: concern over a painful insertion, difficulty of insertion, higher risk of perforation, pelvic inflammatory disease, changes in bleeding pattern, high cost, and risk of extrauterine pregnancy. The presence of such perceived obstacles was associated with less frequent IUD insertion in nulliparous women.
Conclusion: The results of this study provide a valuable insight into the attitudes and opinions of Switzerland’s gynecologists on the use of IUDs in nulliparous and multiparous women, showing that the women’s parity is a factor influencing the physicians’ attitudes and opinions. Further health education might help minimize the physicians’ attitude discrepancies in IUD prescription to nulliparous and multiparous women.
Keywords: intrauterine device, IUD, nulliparous, multiparous, gynecologists, LARC, contraception
Introduction
As a growing number of women are postponing their childbearing projects into their later years of life, an increasingly greater part of the worldwide population demands an effective, long-acting method of contraception. Recent studies have demonstrated that long-acting contraceptive methods, such as intrauterine devices (IUDs), are acceptable and more reliable than others, such as the pill or the patch, which require a daily or weekly intake and the efficacy of which heavily relies on the user’s compliance.1
Despite their known efficacy, recent studies have found that only 12% of women using contraception and 4.8% of nulliparous women use either IUDs or the implant as a means of contraception.2 The use of IUDs among nulliparous women, in particular, has since long been questioned due to aspects such as younger age, lack of experience with gynecological examination, and seemingly increased pain perception.3 Moreover, a recent study conducted in Egypt found that physicians were more reluctant to offer IUDs to nulliparous women, as well as to women aged <20 years old.4
The 2013 “Global Survey of healthcare practitioners’ beliefs and practices around intrauterine contraceptive method use in nulliparous women” evaluated the attitude of health practitioners coming from 15 countries (UK, France, Australia, USA, Mexico, Russia, Turkey, Canada, Germany, the Netherlands, Sweden, Brazil, Ireland, Colombia, and Argentina) and concluded that the main concerns about IUD use in nulliparous women were difficulty of insertion and subsequent pelvic inflammatory disease (PID).1 Moreover, the physicians’ knowledge of the WHO Medical Eligibility Criteria (MEC) recommendations, which have recently stated that the advantages of IUD use in nulliparous women generally outweigh theoretical and proven risks (MEC category 2) for both copper and hormonal Levonorgestrel 20 mg IUDs, was globally lacking.5
Switzerland has been vaunting one of the lowest voluntary abortion rates in the world for the past several decades.6 According to previous studies, such abortion rates are strongly influenced by the “family planning culture”, the available contraceptive methods, and the quality of sexual education.7 To date, however, there is no available data on the physicians’ beliefs and practices on IUD use in nulliparous women in Switzerland, as the country was not included in the previously mentioned 2013 survey.
The aims of this study were to 1) collect and analyze data on the Swiss physicians’ attitudes and beliefs on IUD use in multiparous and nulliparous women and 2) evaluate whether the women’s parity was a factor influencing the gynecologists’ IUD practice, in the view of breaking up the barriers that may restrain the use of such long-acting mean of contraception in nulliparous women.
Material and methods
Study procedure
The Global Survey questionnaire investigating physicians’ attitudes toward IUDs was modified and adapted to Switzerland.1 Prior to its online publication, the questionnaire was pre-tested in order to ensure its validity and reliability. An informed consent form and an anonymous online link to a MonkeySurvey® questionnaire, both of which had been translated into either French or German, were sent to a total of 1,696 gynecologists, of which 750 worked in the French and 946 in the German-speaking part of Switzerland, in either private and/or public clinics. The survey and the informed consent form were emailed by the secretary of the Groupement Romand de la Société Suisse de Gynécologie et Obstétrique to the society’s members, which include health care professionals coming from both the French- and the German-speaking part of the country. No distinction was made between copper and hormonal IUDs, and the brand name of the IUD was not reported in the questionnaire.
Participants’ characteristics
The reported sociodemographic characteristics of the physicians who took part in the study included their age, gender, Swiss region of residence, country of medical diploma and of the gynecology specialty degree attainment (coded as either a Swiss or a foreign diploma for all other countries), and type of health care center in which they practiced (university hospital, private hospital, private clinic, private practice, and their respective combinations). The gynecologists’ experience was defined according to their number of working years (<5, 5–10, >10 years). Their attitude towards IUDs was defined according to two categories: 1) the gynecologist informed the woman about IUDs but addressed her to another colleague for the insertion; 2) the gynecologist inserted and/or taught the IUD insertion technique to another colleague.
The proportion of IUD insertion among women consulting for contraception was reported only among the subset of gynecologists inserting and/or teaching insertion, with a frequency reported as either <15%, 15%–25%, 25%–50%, 50%–75%, and >75% of women. For those gynecologists addressing women to a colleague for IUD insertion, the monthly frequency of women addressed to other colleagues for IUD fitting was reported using the previously stated frequencies. IUD insertion was globally considered as “frequent” when the physician inserted IUDs in 25% or more of his/her patients and “rare” when the participant inserted IUDs in <25% of his/her patients.
IUD benefits
Out of a list of 12 possible benefits deriving from IUD use, the gynecologists were asked to report the degree of importance for each one of them. Such benefits were as follows: 1) effectiveness, 2) freedom, 3) high continuation rate, 4) cost-effectiveness, 5) lighter bleeding, 6) appreciation by women, 7) emergency contraception, 8) uterine cancer risk reduction, 9) quick return to fertility, 10) long term contraception, 11) minimal contraindications, and 12) little medication interaction. The importance degree was dichotomized as either important or very important vs all others, which were therefore encoded as not important. In the group of gynecologists using and/or teaching IUD insertion, benefits considered as important were analyzed as predictors of frequent vs rare IUD use in all patients with no distinction between multiparous and nulliparous women.
Barriers to IUD insertion
Barriers to the gynecologists’ IUD insertion were reported in a list of 17 items, which included lack of efficacy, pelvic infection, infertility, insertion difficulty, pain during insertion, extrauterine pregnancy, not appreciated by the women, expulsion, the woman’s age, lack of information, religious/ethic, changes in bleeding pattern, high cost, the woman’s sexual behavior, and risk of uterine perforation. Barriers were reported specifically for nulliparous women, as either present or absent for each one of the items.
Comparison of IUD insertion in nulliparous and multiparous women
Six questions were added in order to further compare the gynecologists’ attitude toward IUD insertion in nulliparous vs multiparous women. The questions were about IUD efficacy, risk of genital infection, uterine perforation, and expulsion, ease of insertion, and pain during insertion.
Statistical analyses
Statistical analyses were carried out by a qualified bio-statistician using SAS 9.2 (SAS Institute Inc., Cary, NC, USA). Results were presented as proportions (%). All hypotheses were two sided at the 0.05 significance level.
The chi-squared test and Fischer’s exact test were used, where appropriate, to assess the relationship between the participant’s characteristics according to the two Swiss regions (French and German) as well as frequency of IUD use according to women’s parity (bivariate analysis).
Ethics approval and informed consent
As specified by the local ethics committee (Comité cantonale d’éthique de la recherche), as the present study was focused on the physicians’ opinions and attitudes rather than their individual patients, no ethics approval was required for the present study.
Results
Response rate
A total of 156/750 (21%) and 143/946 (15%) French and German gynecologists, respectively, completed the online questionnaire. The combined response rate for the two Swiss regions was 299/1,696 (17.6%). When comparing the characteristics of gynecologists in the French- and German-speaking part of Switzerland, we found similar percentages of female gynecologists, of country of medical and specialty diploma obtention. Because of the little discrepancies in the participants’ characteristics and for the purpose of keeping the sample size as large as possible in order to fulfill the study’s primary objective, all analyses in this paper were carried out by grouping the two Swiss regions together.
Participants’ characteristics
Table 1 reports the baseline characteristics of the participants. Overall, 228/299 (88.6%) respondents had obtained their specialty title in Switzerland. A total of 185/299 (61.9%) of the gynecologists were females. The participants’ mean age was 50 years, and 156/299 (52.2%) of them worked exclusively in private clinics. A total of 284/299 participants (95.0%) offered IUDs to their patients and/or trained other gynecologists to insert them.
  | Table 1 Participants’ sociodemographic characteristics |
IUD fitting
Table 2 reports the frequency of IUD insertion among women consulting for contraception for the subset of gynecologists either only inserting (n=64) or both practicing and teaching IUD insertion (n=220) on nulliparous and multiparous women. Among gynecologists fitting IUDs and/or teaching IUD fitting, 204/284 (72.9%) and 33/284 (11.8%) of them prescribed IUDs frequently to multiparous and nulliparous women, respectively (P<0.0001).
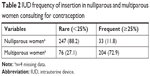  | Table 2 IUD frequency of insertion in nulliparous and multiparous women consulting for contraception |
Association between women’s parity and IUD fitting
In the group of gynecologists frequently fitting IUDs in multiparous women (n=204/299, 72.9%), only 30/204 of them (14.7%) were also frequently fitting IUDs in nulliparous women. Among (n=33, 11.8%) gynecologists frequently fitting IUDs in nulliparous women, the majority of them (30/33, 90.9%) also frequently fit IUDs in multiparous ones.
Moreover, we found that female gynecologists were more likely than their male counterparts to frequently fit IUDs (OR 1.7, 95% CI: 1.0–2.9) on all women, regardless of their parity.
IUD perceived benefits
The main perceived benefits of IUD insertion for the physicians’ patients were as follows: effectiveness (96.6%), long-term contraception (95.8%), high compliance (95.0%), and appreciation (92.7%). Benefits considered as either important or very important were associated with a significant increase in the probability of frequent IUD insertion. The benefits of IUD insertion according to the study participants are reported in Figure 1.
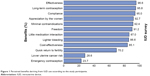  | Figure 1 Perceived benefits deriving from IUD use according to the study participants. |
Barriers to IUD use in nulliparous women
The most frequently reported obstacles to IUD prescription to nulliparous women were concern over painful insertion (57.9%), difficulty of insertion (46.2%), higher risk of perforation (30.5%), PID (26.4%), changes in bleeding pattern (18.4%), high cost (16.1%), and extrauterine pregnancy (15.7%). All other barriers were mentioned by <15% of the gynecologists. Figure 2 illustrates the main barriers to IUD prescription for nulliparous women.
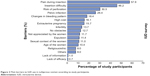  | Figure 2 Main barriers to IUD use in nulliparous women according to study participants. |
Increasing confidence in IUD use in nulliparous women
When asked about what could increase their confidence in IUD use in nulliparous women, 44.6% of gynecologists stated already feeling confident enough to prescribe IUDs to nulliparous women. The remaining respondents suggested that, to increase their knowledge and confidence on the subject, they mostly wished to have more information relative to pain during insertion (23.1%), risk of infection (22.1%), and expulsion rate (19.7%). They also wished to assist to more congress presentations on the theme (22.4%) and to have more precise national guidelines to rely on (20.1%). The factors potentially capable of increasing the gynecologists’ trust in IUD use in nulliparous women are illustrated in Figure 3. Finally, 4.5% of the participants said that nothing could increase their confidence in IUD insertion in nulliparous women.
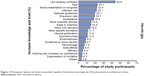  | Figure 3 Participants’ opinion on factors potentially capable of increasing knowledge on IUD prescription to nulliparous women. |
A total of 37.3% of the participants had full knowledge of the MEC 2 category recommendations.
Discussion
With only a minority (11.8%) of the participants frequently inserting IUDs in nulliparous women, we found that the main barriers to IUD insertion in this part of the population were concern over painful insertion, difficulty of insertion, higher risk of perforation, PID, changes in bleeding patterns, high cost, and extrauterine pregnancy. Similarly, a study conducted in Australia found that, while most general physicians were confident about IUD insertion in multiparous women, only 46% of them felt confident about IUD insertion in nulliparous patients.8 Another study conducted in the United States found that only 66% and 43% of the American College of Obstetricians and Gynecologists’ members considered IUDs to be an appropriate means of contraception for nulliparous and adolescent women, respectively.9 Our results are in line with those of the 2013 Global Survey, according to which the main barriers to IUD insertion in nulliparous women were as follows: fear of PID, difficulty of insertion, painful fitting, and concern over infertility. Moreover, according to both the results of our study and those of the Global Survey, insertion was perceived to be more difficult and more painful in nulliparous women by the majority of the physicians.1
Concerning knowledge of the most recent MEC criteria, we found that only 37.3% of our study participants, of which 76.7% and 48.5% came from the French- and German-speaking part of Switzerland, respectively, felt confident about their knowledge of the recommendations in regard to IUDs, while the results of the 2013 Global Survey show that 53.1% of gynecologists coming from different worldwide countries correctly recognized MEC 2 category for IUD use in nulliparous women.1 Such result is in line with the small proportion of gynecologists frequently inserting IUDs in nulliparous women found in our study and further underlines the importance of spreading knowledge and raising awareness of the latest recommendations on the subject as a means to boost the physicians’ confidence in IUD prescription to nulliparous women. Moreover, we found that those practitioners who considered nulliparous and adolescent women as appropriate IUD candidates were those who also recalled reading a college clinical publication on the subject, as well as those who strongly agreed that unintended pregnancy was a serious problem in their practice. Similarly, a study conducted in Egypt found that, while only 22% of the physicians would recommend IUDs to nulliparous women, continuous education and in-service training on the updated MEC criteria may lower the medical restrictions to IUD use.4 Such results underline the importance of continuous education and training in order to boost the gynecologists’ confidence in the subject and to allow them to further increase the practice of IUD fitting among both multiparous and nulliparous women.
While concerns over painful insertion, difficulty of insertion, risk of perforation, PID, changes in bleeding pattern, high cost, and extrauterine pregnancy, were among the gynecologists’ most reported barriers for IUD fitting, it is essential to realize that the patients’ reluctance to IUD use might be due to additional and/or different reasons than those of their physicians. A recently published literature review on the subject concluded that, although nulliparity is seemingly associated with higher pain and difficulty at IUD insertion, most IUD insertions are well tolerated and successful in this group of women.10 Previously reported, additional patient concerns include infertility, weight gain, acne, and discomfort deriving from a foreign body.11 Moreover, according to the findings of the European TANCO study, despite the high levels of satisfaction with the available contraceptive methods, women wish to be more thoroughly informed about such methods by their physicians.12
To the best of our knowledge, this is the first study to explore the Swiss practitioners’ attitudes toward IUD insertion in nulliparous and multiparous women, thus providing an insight into the measures needed to improve the everyday practice of family planning in the country.
Limitations
First of all, the study did not include the Italian-speaking part of Switzerland. However, the “Office Fédéral de la Statistique” latest report found that the Italian-speaking population represents only 6.5% of the entire Swiss population.13 A selection bias may have also have occurred, as only those gynecologists who are part of the mailing list of the “Groupement Romand de la Société Suisse de Gynécologie et Obstétrique” had the possibility of taking part in the study. Finally, the main criticism raised by the participants was the lack of distinction between copper and hormonal IUD, as some answers would have been different depending on the type of IUD considered.
Conclusion
This survey provides a valuable insight into the attitudes and opinions of Switzerland’s gynecologists on the use of IUDs in nulliparous and multiparous women, showing that the women’s parity is a factor influencing the physicians’ attitudes and opinion while also revealing a knowledge gap of the international recommendations for IUD use for nulliparous women. Additional, evidence-based education and training on the subject may help minimize attitude discrepancies in prescribing IUDs to nulliparous and multiparous women. Further studies should focus on the women’s own perceptions and expectations over IUD use, in the view of helping them make a more informed contraceptive choice by improving the discussions with health care providers.
Acknowledgments
The authors would like to thank all the Swiss gynecologists who took some of their time to complete our questionnaire, and a particular thank you to Prof Merki Gabriele and Sabine Gisler for collaborating with us and making this survey possible. This study was supported by the Geneva University Hospitals.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Black KI, Lotke P, Lira J, Peers T, Zite NB. Global survey of healthcare practitioners’ beliefs and practices around intrauterine contraceptive method use in nulliparous women. Contraception. 2013;88(5):650–656. | ||
Evans ML, Espey E, Ogburn T, Zite NB. Use of long-acting reversible contraception by obstetrics and gynecology residents: an examination of access for all women. Obstet Gynecol. 2018;131(3):538–541. | ||
Akers AY, Harding J, Perriera LK, et al. Satisfaction with the intrauterine device insertion procedure among adolescent and young adult women. Obstet Gynecol. 2018;131(6):1130–1136. | ||
Aziz M, Ahmed S, Ahmed B. Attitudes of physicians providing family planning services in Egypt about recommending intrauterine device for family planning clients. Sex Reprod Healthc. 2017;14:64–68. | ||
Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep. 2016;65(3):1–103. | ||
Stamm H, Gloor PA, Dondénaz M, et al. [Interruption of pregnancy in Switzerland 1982–1986]. Schweiz Rundsch Med Prax. 1990;79(9):229–234. German. | ||
Ketting E. Conference of Dr. Evert Ketting. Berne: 1998. Available from: http://www.svss-uspda.ch/fr/facts/prevenir.htm. Accessed April 30, 2018. | ||
Stewart M, Digiusto E, Bateson D, South R, Black KI. Outcomes of intrauterine device insertion training for doctors working in primary care. Aust Fam Physician. 2016;45(11):837–841. | ||
Luchowski AT, Anderson BL, Power ML, et al. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89(6):572–577. | ||
Lohr PA, Lyus R, Prager S. Use of intrauterine devices in nulliparous women. Contraception. 2017;95(6):529–537. | ||
Hardeman J, Weiss BD. Intrauterine devices: an update. Am Fam Physician. 2014;89(6):445–450. | ||
Merki-Feld GS, Caetano C, Porz TC, Bitzer J. Are there unmet needs in contraceptive counselling and choice? Findings of the European TANCO study. Eur J Contracept Reprod Health Care. 2018;23(3):183–193. | ||
Atlas Graphique et Statistique de la Suisse 1914–2014. Office fédéral de la statistique. Neuchâtel 2015. Numéro OFS 1469-1400. 2015. Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/statistique-regions/atlas/atlas-graphique-statistique-suisse-1914-2014.html. Accessed April 30, 2018. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
