Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 16
Survival Rates in Elderly Patients on Continuous Ambulatory Peritoneal Dialysis
Authors Nguyen B, Bui QTH, Tran PQ
Received 1 December 2022
Accepted for publication 29 March 2023
Published 19 April 2023 Volume 2023:16 Pages 131—141
DOI https://doi.org/10.2147/IJNRD.S397555
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Bach Nguyen,1 Quynh Thi Huong Bui,2,3 Phuong Que Tran2
1Department of Nephrology, Thong Nhat Hospital, Ho Chi Minh City, Vietnam; 2Department of Clinical Pharmacy, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam; 3Department of Pharmacy, Thong Nhat Hospital, Ho Chi Minh City, Vietnam
Correspondence: Bach Nguyen, Department of Nephrology, Thong Nhat Hospital, 1 Ly Thuong Kiet Street, Tan Binh District, Ho Chi Minh City, 700000, Vietnam, Tel +84 28 918209808, Fax +84 28 3865 6715, Email [email protected]
Purpose: The present study aimed at evaluating the survival rate, its associated factors, and the causes of death in elderly patients undergoing continuous ambulatory peritoneal dialysis (CAPD) in Vietnam.
Patients and Methods: This is a retrospective, observational study conducted among patients aged ≥ 65 years who underwent CAPD at Thong Nhat Hospital, Ho Chi Minh City, Vietnam, from April 2012 to December 2020. The Kaplan–Meier method was used to calculate the cumulative survival rate, and the Log rank test was used to analyze the factors associated with the survival rate of patients.
Results: This study enrolled a total of 68 patients with a mean age of 71.93 ± 7.44 years at the initiation of CAPD. The most common complication among kidney failure patients was diabetic nephropathy (39.71%). The rate of concomitant cardiovascular diseases was 58.82%. The average survival rate was 45.59 ± 4.01 months. Peritonitis was the most common factor causing death (31.25%), followed by cardiovascular diseases (28.12%) and malnutrition (25%). The factors that impacted the survival rate included concomitant cardiovascular diseases, low serum albumin (< 35 g/dL), and an indication of CAPD due to exhausted vascular access for hemodialysis at baseline. The main factor associated with a shorter survival time was concomitant cardiovascular diseases.
Conclusion: It is necessary to improve the survival time beyond 5 years for elderly patients undergoing CAPD, especially for those with concomitant cardiovascular diseases. Besides the prevention of peritonitis, adequate measures to protect from cardiovascular diseases and malnutrition will reduce the mortality rate in patients on CAPD.
Keywords: CAPD, elderly, Vietnamese, concomitant diseases, cardiovascular diseases
Introduction
Kidney failure is a global burden, and elderly individuals are observed to be the most rapidly expanding population affected by it due to a spike in life expectancies globally.1 In Vietnam, the incidence of kidney failure has been increasing continuously, and nearly 90,000 cases need dialysis.2 Moreover, the hospital systems of Vietnam are overloaded due to the availability of only 400 dialysis facilities and approximately 5000 dialysis machines in the country.3,4 Therefore, many patients choose continuous ambulatory peritoneal dialysis (CAPD). Elderly patients especially prefer CAPD because it has always been perceived to be easier than hemodialysis (HD), with a smaller burden on patients and providing an augmented quality of life (QoL).5 Therefore, the management of elderly patients on CAPD has received increasing attention in recent years because this population has burgeoning numbers and a unique profile of medical and social needs.
There are some specific challenges faced by Vietnamese patients on CAPD, which are different from other countries. Firstly, renal replacement therapies (RRTs) are always delayed in patients from Vietnam.6 There is a tendency to postpone the initiation of dialysis as much as possible. Secondly, HD is still the first choice of RRT for kidney failure patients in Vietnam. The economic situation also plays a role in choosing HD over CAPD.6 The cost of one session of HD is only 20 USD, which allows reusing a dialyzer six times, which is cost-effective compared to CAPD.6 Moreover, physicians are skeptical about the performance of CAPD and concerned about the associated high risk of peritonitis due to inadequate patient training, low living conditions, and environmental pollution. Finally, elderly patients on CAPD always require assistance and care from family members. However, a study by Brown et al7 demonstrated that both elderly and younger patients have similar rates of peritonitis and technique failure. Moreover, no significant difference was observed in the QoL of elderly patients who were maintained on CAPD in comparison to those on HD.7
There is a lack of national data on the survival rate and cause of death in patients on CAPD in Vietnam, especially in elderly patients. Therefore, this study aimed at evaluating the survival rate and identifying the factors influencing the survival rate in elderly patients undergoing CAPD. This retrospective, observational study is designed to provide insight into the clinical outcomes of elderly Vietnamese patients on CAPD.
Patients and Methods
Study Design and Setting
A retrospective, observational study was conducted on patients diagnosed with kidney failure (International Classification of Diseases, Tenth Revision [ICD-10]; code: N18) who were on CAPD at the Thong Nhat Hospital, South Vietnam, from April 2012 to December 2020. The inclusion criteria were as follows: (1) patients aged ≥65 years and who underwent CAPD for more than 3 months at the Thong Nhat Hospital, (2) patients who received the appropriate CAPD prescription and used conventional dialysis fluids (Dianeal® 1.5% and 2.5%, or 4.25% dextrose; Baxter Healthcare) with a Y-set and twin-bag system and 2-L exchanges four times daily, 7 days a week, and (3) patients for whom all data were available. Patients who could have a risk of acute-on-chronic kidney disease or could have withdrawn from CAPD therapy were excluded. The standard criteria for introducing CAPD therapy to patients was a creatinine clearance of <10 mL/min for nondiabetic patients and <15 mL/min for diabetic patients, respectively. Anemia treatment was continued until a target hemoglobin level of ≥10 g/dL was achieved. Patients who had anemia were subcutaneously administered with long-acting erythropoietin agents (methoxy polyethylene glycol-epoetin beta) at a dose of 100 µg per month, adjusted according to the hemoglobin level. Insulin and antihypertensive drugs were used to control the high blood sugar and high blood pressure of patients, respectively. Calcium, vitamin D, and iron supplements were also prescribed to patients when required. In the present study, due to a shortage of peritoneal dialysis (PD) nurses, Kt/V data were not routinely calculated for all patients. However, Kt/V was measured only in some cases that showed signs of inadequate dialysis. Most of the patients were prescribed dialysis fluids (Dianeal® 1.5% and 2.5%, or 4.25% dextrose), 2-L exchanges four times daily, 7 days a week.
The demographic characteristics and medical history of the enrolled patients were collected from the medical records. The demographic characteristics included age at the initiation of CAPD, sex, dry weight, primary causes of kidney failure, concomitant cardiovascular diseases, peritonitis, the indication or selection of CAPD, the initiation of CAPD with acute HD, CAPD exchange with assistance, and survival time (months). The concomitant cardiovascular diseases included history of congestive heart failure, cerebrovascular accident, myocardial infarction (MI), atherosclerosis, thoracic or abdominal artery aneurysm, and cardiac arrhythmia. The criteria for patients diagnosed with peritonitis (ICD-10; code: K65.9) included: (1) clinical features of abdominal pain, fever, nausea, vomiting, and cloudy fluid on drainage, (2) the number of white blood cells (WBCs) found on microscopy alone: either >50 or >100 WBC/mm3 and neutrophil count >50%, and (3) detection of bacteria in the peritoneal effluent by culture or Gram’s stain.8 Data on baseline laboratory variables included measurements of hemoglobin, total cholesterol, fasting glucose, low- and high-density lipoprotein cholesterol, hyperlipidemia, triglyceride, serum albumin, calcium, parathyroid hormone, and phosphate. Hyperlipidemia was defined as the presence of hypercholesterolemia (total cholesterol exceeding 5.2 mmol/L) or hypertriglyceridemia (triglycerides exceeding 1.7 mmol/L), or both.
Causes of Death in Elderly Patients on CAPD
The causes of death were categorized as: (1) peritonitis, (2) cardiovascular diseases (MI, heart failure, stroke), (3) malnutrition, and (4) other causes (malignancy, tuberculosis, unknown). Disease-related mortality was defined as death with active diseases or within 4 weeks of a disease episode or any death during hospitalization for diseases. The standard criteria for diagnosing malnutrition in the study hospital were based on Subjective Global Assessment.9
Statistical Analysis
Data analyses were performed using SPSS version 23.0 (IBM, Armonk, New York). Continuous variables with a normal distribution are presented as mean ± standard deviation, and percentages are reported to describe the categorical variable. The Kaplan–Meier method was used to calculate the cumulative survival rate. The Log rank test was used to analyze the factors that impacted the survival rate. In addition, the Cox proportional hazards model or regression analysis was used to calculate the hazard rate. For univariate analysis, a cross-tabulation was created for one factor/variable and a chi-square test was performed. Any factor that was determined to be significant in the univariate analysis was used in the multivariate analysis. In the two-tailed test, p-values <0.05 were considered statistically significant.
Ethical Approval
The protocol of this study was approved by the Institutional Review Board of Thong Nhat Hospital, Ho Chi Minh City, Vietnam. Informed consent was obtained from the study participants before the study commencement. All the personal information of patients was kept confidential. The ethical standards of the institutional and/or national research committee were followed for all procedures and amendments, which were comparable to the ethical standards of the 1964 Helsinki Declaration.
Results
Demographic and Other Baseline Characteristics
The baseline clinical and laboratory characteristics of the enrolled patients (n=68) are presented in Table 1 and Table 2. The average age at the initiation of CAPD was 71.93 ± 7.44 years, and in 36 patients (52.945%), CAPD was started at the age of ≥70 years. The most common primary disease associated with kidney failure was diabetic nephropathy (39.71%), followed by hypertension (30.88%). The introduction of CAPD with acute HD occurred in 80.88% of patients. The most common coexisting condition was cardiovascular disease, which was reported in 58.82% of patients. The average survival time was 45.59 ± 4.01 months. Low serum albumin (<35 g/dL) and hyperlipidemia at baseline were reported in 49 (72.06%) and 55 (80.88%) patients, respectively.
 |
Table 1 Baseline Clinical Characteristics of Elderly Patients on CAPD (N=68) |
 |
Table 2 Baseline Laboratory Characteristics of Elderly Patients on CAPD (N=68) |
Survival Rates in Elderly Patients on CAPD
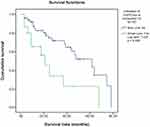
The cumulative survival rate of the enrolled patients is presented in Figure 1. The survival rates of patients at 12, 24, and 60 months were 85%, 75%, and 45%, respectively. The cumulative survival rate using the Kaplan–Meier method was shown for each factor, and the Log rank test was utilized to compare those factors. Initially, patients were compared by dividing them into two groups as per the age at the initiation of CAPD—under 70 and 70 years or older (Table 3). There was no significant decrease in the survival rate for patients aged ≥70 years (Table 3). The nondiabetic patient group showed a higher survival time than the diabetic group; however, there was no statistical significance (Table 3). Moreover, there was a significant difference observed even between patients grouped as with or without concomitant cardiovascular diseases. The average survival time for patients with and without concomitant cardiovascular diseases was 37.55 ± 4.83 and 60.30 ± 6.00 months, respectively (Figure 2). The patient group with the indication of CAPD due to exhausted vascular access for HD had a significantly lower survival time than the patient group without such indication (Figure 3). In addition, there was a major difference seen even with the different baseline levels of serum albumin. Compared to the patient group with high baseline serum albumin (≥35 g/dL), the patient group with low baseline serum albumin (<35 g/dL) had a significantly lower survival time (Figure 4).
 |
Table 3 Factors at Baseline Affecting the Survival Time |
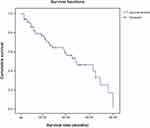 |
Figure 1 Kaplan–Meier survival curves of elderly patients on continuous ambulatory peritoneal dialysis. |
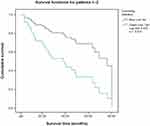 |
Figure 2 Factor (concomitant cardiovascular diseases at baseline) added to Kaplan–Meier and Log rank test. |
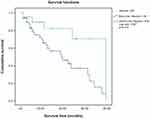 |
Figure 4 Factor (baseline serum albumin) added to Kaplan–Meier and Log rank test. |
Factors Affecting the Survival Rate
In a multivariate analysis using the Cox proportional hazards model, a univariate chi-square test was performed on the three factors (concomitant cardiovascular diseases, indication of CAPD due to exhausted vascular access for HD, and low serum albumin) with a hazard rate of less than 1. There was no significant difference in the group indicated for CAPD due to exhausted vascular access for HD and serum albumin. However, the presence of concomitant cardiovascular diseases significantly impacted the survival time (Table 4).
 |
Table 4 Multivariate Analysis: Cox Proportional Hazards Model Including Factors Predicting Mortality |
Causes of Death in Elderly Patients on CAPD
In the analysis of causes of death, peritonitis was demonstrated to be the most common risk factor (31.25%), followed by cardiovascular diseases (28.12%). Deaths from malnutrition accounted for 25% (Table 5).
 |
Table 5 Causes of Death (N=32) |
Discussion
This retrospective study is the first statistical presentation of the survival rate of patients on CAPD in Vietnam. It was aimed at analyzing the data collected in Thong Nhat Hospital, South Vietnam, from April 2012 to December 2020 to retrospect the clinical outcome of CAPD in elderly patients and the role played by comorbid conditions in the clinical prognosis of these patients. The present study reported the average survival time for the enrolled elderly patients on CAPD to be 45.59 ± 4.01 months. This result is similar to that of another single-center retrospective study conducted in China, where the 1-, 2-, 3-, and 5-year patient survival rates were reported to be 81%, 71%, 59%, and 39%, respectively, in the group aged 65–74 years. The mean survival time of the group aged 65–74 years was 43.1 months.10 Similarly, a study by Steenkamp et al11 conducted in the United Kingdom showed that the average survival time in elderly patients on CAPD (>75 years) was 3 years. In the present study, survival rates of patients were 85%, 75%, and 45% after 12, 24, and 60 months, respectively (Figure 1). The survival rate reached 85% in elderly patients on CAPD after 12 months in the present study, which is similar to that of previously reported studies.11,12 Steenkamp et al11 reported the 1-year survival rate in patients aged ≥60 years to be 88.1% in 2001, which increased to 89.8% in 2010. This study also reported the 1-year survival rate in patients with diabetes to be 82.1% and 84.7% in 2002 and 2010, respectively. Otawa et al12 showed that in patients >80 years of age, the survival rate after 12 months was 83%.
In the present study, the survival rate reported after 2 years was 75%, which is lower than the rate reported by Lo et al13 (84.9% among the enrolled patients [n=320]) in the study conducted in 2003. In the present study, the survival rate after 5 years was only 45%, and this rate is lower than the rates reported by Wei et al14 who enrolled Canadian (n=256) and Chinese (n=240) patients from 2000 to 2004 in their study. The survival rates reported by Wei et al14 after 1, 2, 3, and 5 years in Canadian patients were 90%, 79%, 72%, and 61%, respectively, whereas in Chinese patients, the survival rates were 90%, 79%, 71%, and 64%, respectively. Meanwhile, in Japan, a study by Hiramatsu et al15 reported only a 16.3% (n=27) survival rate at >5 years among the enrolled patients (≥65 years) who underwent CAPD from 1991 to 2006 and had started dialysis at an average age of 66.2 years. A study conducted in China on 148 patients (>65 years) with a mean age of 71.3 ± 4.3 years showed that the survival rates for 1, 2, 3, and 5 years were 79%, 67%, 56%, and 30%, respectively.10
The results of the present study can be compared to those of a few previous studies conducted in different countries for the 1-year and 2-year survival rates, but the 5-year survival rate was lower in the present study. Improvisations should be made for the prognosis of patients undergoing CAPD based on long-term care. It can be hypothesized that due to four main reasons, the enrolled study population demonstrated a lower survival rate in comparison to other studies. Firstly, the population enrolled in the present study had a higher age in comparison to the patients included in other studies. Moreover, patients in the present study had a high age at the onset of CAPD (71.93 ± 7.44), which was comparatively higher than the population enrolled in the studies by Lo et al and Wei et al13,14 Secondly, patients in the present study had many medical comorbidities at baseline, which is a feature of the elderly population. Common diseases affecting patients’ survival time were severe heart failure and severe coronary artery disease. Thirdly, some of the patients had a late indication of CAPD. In Vietnam, in almost all cases, CAPD is conducted in an emergency department. Acute HD introduction was very difficult for elderly patients. Even with a better-planned CAPD initiation, acute HD introduction has been impossible in Vietnam due to poor chronic kidney disease management, patient compliance, and socioeconomic problems. Lastly, the criteria for selecting elderly patients on CAPD in this study were peripheral vascular exhaustion for vascular access surgery for HD (22.06%) and heart failure (17.65%) as presented in Table 1. The study by Hiramatsu et al15 reported that severe cardiovascular disease and peripheral vascular exhaustion for HD accounted for 13% and 8%, respectively; therefore, they demonstrated a low 5-year survival rate. In the present study, the rates of both peripheral exhaustion of vascular access for HD and cardiovascular diseases are higher in comparison to those of the study by Hiramatsu et al,15 thereby suggesting that this might have led to a lower 5-year survival rate among patients.
In the present study, peritonitis is reported to be the major cause of death among elderly Vietnamese patients on CAPD. In the present study, the patients had risk factors for peritonitis due to poor sanitary conditions, diabetes, severe malnutrition, and not strictly adhering to aseptic CAPD exchange. A study in elderly patients on CAPD with peritonitis as a complication reported that gram-negative organisms were primarily responsible for the episodes of peritonitis. Among the gram-negative organisms, Escherichia coli and Klebsiella pneumoniae were overwhelmingly dominant organisms. In the present study, the rates of death due to peritonitis were higher in comparison to the rates of other studies. However, a study by Wu et al16 also showed a high percentage (58.6%) of peritonitis-related deaths in elderly patients aged >65 years, which is even higher than that reported in the present study (31.25%), whereas in another study by Hiramatsu et al,15 death due to peritonitis was accounted to be only 7.6%.To minimize peritonitis episodes, it is important to improve the training for patients on CAPD, extend family support, and provide assistance to at-risk patients, thereby avoiding withdrawal of PD.
Patients undergoing CAPD with coexisting cardiovascular diseases often die at their homes suddenly, and due to a lack of autopsy, the exact cause of death is often not recorded. However, through the medical records and observation of their disease progression, from the present study it could suggested that acute MI and stroke are the crucial underlying risk factors causing death. The results of the present study are similar to those of the study by Hiramatsu et al,15 which reported that the cause of death due to MI was 15.2%. Furthermore, a study by Abraham et al17 in patients on CAPD (n=309) of various ages showed that the main cause of death was cardiovascular disease (59%). It can be noted that another possible cause of death in elderly patients on CAPD was severe physical exhaustion. In the present study, 25% of patients died due to severe malnutrition (Subjective Global Assessment-C). Table 2 shows that 72.06% of patients on CAPD had baseline serum albumin <35 g/dL. Malnutrition is also a frequently encountered complication in elderly patients on CAPD and can lead to a poor prognosis. Steenkamp et al11 investigated the survival rate of patients who were on dialysis in the United Kingdom from 1997 to 2010 and reported that the rate of contribution of treatment withdrawal to cause of death was 18% for prevalent dialysis patients.
Limitations
Firstly, this was an observational study; therefore, it is uncertain whether a causal relationship exists between survival time and independent variables. Secondly, this was a single-center study that enrolled a low number of patients. However, there was little variation in the CAPD technique and prescription, and the therapy regimen followed, thereby increasing the reliability. Finally, there was a lack of longitudinal data focusing on risk factors such as serum lipid, phosphate, calcium, and glucose levels and factors attributing to death, especially in patients who were on dialysis and had died at home. However, to the best of our knowledge, this study is the first statistic focusing on the survival rate of Vietnamese patients on CAPD. Factors were analyzed specifically; therefore, confounding factors were limited. Future studies enrolling a larger number of patients and higher data inputs are required for providing conclusive evidence.
Conclusion
This is the first report presenting the survival rate of elderly patients on CAPD in Vietnam; however, it included data from only one hospital. The survival time results of the present study can be compared to the survival rates usually observed among elderly patients on CAPD. Concomitant cardiovascular diseases reduce the survival rate of elderly patients on CAPD. This study also showed that the leading cause of death in this vulnerable population is peritonitis, followed by severe cardiovascular disease. Future long-term studies can be conducted in Vietnam to overcome the challenges faced by elderly patients on CAPD and to improvise their long-term rate of survival.
Abbreviations
CAPD, Continuous ambulatory peritoneal dialysis; HD, Hemodialysis; QoL, Quality of life; RRT, Renal replacement therapy; WBC, White blood cells.
Acknowledgments
The authors thank BioQuest Solutions for the editorial assistance that was funded by Baxter. The authors also thank Kevin Moses for reviewing and revising the manuscript. We are indebted to the nephrologists and nurses at the Department of Nephrology and Dialysis, Thong Nhat Hospital, for their collaboration in this study.
We are indebted to the nephrologists and nurses at the Department of Nephrology and Dialysis, Thong Nhat Hospital, for their collaboration in this study.
Author Contributions
All the authors made a significant contribution to the work reported, whether in the study conception, design, execution, acquisition of data, analysis and interpretation, or in all of these areas; participated in drafting, revising or critically reviewing the article; provided a final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Stevens LA, Viswanathan G, Weiner DE. Chronic kidney disease and end-stage renal disease in the elderly population: current prevalence, future projections, and clinical significance. Adv Chronic Kidney Dis. 2010;17(4):293–301. doi:10.1053/j.ackd.2010.03.010
2. Hyodo T, Fukagawa M, Hirawa N, et al. Present status of renal replacement therapy in Asian countries as of 2017: Vietnam, Myanmar, and Cambodia. Ren Replace Ther. 2020;6(65). doi:10.1186/s41100-020-00312-w
3. Viet Nam New. Kidney dialysis treatment falling short in Việt Nam. Available from: https://vietnamnews.vn/society/803890/kidney-dialysis-treatment-falling-short-in-viet-nam.html.
4. Van BP, Duc CV. Global dialysis perspective: Vietnam. Am Soc Nephrol. 2020;1(9):974–976.
5. Tran PQ, Nguyen NTY, Nguyen B, Bui QTH. Quality of life assessment in patients on chronic dialysis: comparison between haemodialysis and peritoneal dialysis at a national hospital in Vietnam. Trop Med Int Health. 2022;27(2):199–206. doi:10.1111/tmi.13709
6. Nguyen B, Fukuuchi F. Survival rates and causes of death in Vietnamese chronic hemodialysis patients. Ren Replace Ther. 2017;3:22. doi:10.1186/s41100-017-0099-6
7. Brown EA. Should older patients be offered peritoneal dialysis? Perit Dial Int. 2008;28(5):444–448. doi:10.1177/089686080802800503
8. Cheuk CS, Philip KTL, David JL. Peritonitis and exit-site infection. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of Dialysis.
9. Rosnes KS, Henriksen C, Høidalen A, Paur I. Agreement between the GLIM criteria and PG-SGA in a mixed patient population at a nutrition outpatient clinic. Clin Nutr. 2021;40(8):5030–5037. doi:10.1016/j.clnu.2021.07.019
10. Joshi U, Guo Q, Yi C, et al. Clinical outcomes in elderly patients on chronic peritoneal dialysis: a retrospective study from a single center in China. Perit Dial Int. 2014;34(3):299–307. doi:10.3747/pdi.2012.00209
11. Steenkamp R, Shaw C, Feest T. UK renal registry 15th annual report: chapter 5 survival and causes of death of UK adult patients on renal replacement therapy in 2011: national and centre-specific analyses. Nephron Clin Pract. 2013;123(1):93–123. doi:10.1159/000353324
12. Otawa T, Sakurada T, Nagasawa M, et al. Clinical outcomes in elderly (more than 80 years of age) peritoneal dialysis patients: five years’ experience at two centers. Adv Perit Dial. 2013;29:43–45.
13. Lo WK, Ho YW, Li CS, et al. Effect of Kt/V on survival and clinical outcome in CAPD patients in a randomized prospective study. Kidney Inter. 2003;64(2):649–656. doi:10.1046/j.1523-1755.2003.00098.x
14. Wei F, Jiaqi Q, Aiwu L, et al. Comparison of peritoneal dialysis practice patterns and outcomes between a Canadian and a Chinese centre. Nephrol Dial Transplant. 2008;23:4021–4028. doi:10.1093/ndt/gfn372
15. Hiramatsu M. Japanese Society for Elderly Patients on Peritoneal Dialysis. How to improve survival in geriatric peritoneal dialysis patients. Perit Dial Int. 2007;27(2):S185–S189. doi:10.1177/089686080702702s32
16. Wu H, Ye H, Huang R, et al. Incidence and risk factors of peritoneal dialysis-related peritonitis in elderly patients: a retrospective clinical study. Perit Dial Int. 2020;40(1):26–33. doi:10.1177/0896860819879868
17. Abraham G, Kumar V, Nayak KS, et al. Predictors of long-term survival on peritoneal dialysis in South India: a multicenter study. Perit Dial Int. 2010;30(1):29–34. doi:10.3747/pdi.2008.00028
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.