Back to Journals » Clinical Ophthalmology » Volume 14
Surgical Options for Optic Disc Pit Maculopathy: Perspectives and Controversies
Authors Pastor-Idoate S , García-Arumí Fusté C , García-Onrubia L, Copete S, García-Arumí J
Received 23 February 2020
Accepted for publication 16 April 2020
Published 16 June 2020 Volume 2020:14 Pages 1601—1608
DOI https://doi.org/10.2147/OPTH.S250921
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Salvador Pastor-Idoate,1– 3 Claudia García-Arumí Fusté,4,5 Luis García-Onrubia,1 Sergio Copete,6 José García-Arumí3– 5,7,8
1IOBA Eye Institute, University of Valladolid, Valladolid, Spain; 2Clinical University Hospital of Valladolid, Valladolid, Spain; 3Red Temática de Investigación Cooperativa en Salud (RETICS), Oftared, Instituto de Salud Carlos III, Madrid, Spain; 4Vall d´Hebron University Hospital, Barcelona, Spain; 5Ophthalmology Research, Vall d´Hebron Research Institute (VHIR), Barcelona, Spain; 6Complex University Hospital, Albacete, Spain; 7Ocular Microsurgery Institute (IMO), Barcelona, Spain; 8Department of Ophthalmology, Autonomous University of Barcelona, Barcelona, Spain
Correspondence: José García-Arumí
Vall d´Hebron University Hospital, Passeig De La Vall D’hebron, 119-129, Barcelona 08035, Spain
Tel +34 934 893 000
Fax +34 932 746 185
Email [email protected]
Abstract: Optic disc pit (ODP) is a rare congenital optic nerve head abnormality, which can be complicated by intraretinal and subretinal fluid at the macula (ODP-maculopathy) with progressive visual loss. The source of this fluid remains unclear and the most dominant hypotheses have pointed to vitreous cavity or cerebrospinal fluid. Although spontaneous resolution has been reported, the majority of untreated cases of ODP-maculopathy result in final visual acuity less than 20/200 or worse. A wide array of interventions, either individually or in combination with adjuvant treatments, have been tried with varying degrees of success. Recently, different surgical procedures to fill the ODP by self-sealing materials in combination with pars plana vitrectomy have been reported as an effective adjuvant treatment. However, given the relative rarity of this condition, the majority of reports describe a small retrospective case series, making it difficult to compare among different treatments options and create a consensus regarding the optimal treatment for ODP-maculopathy. In this situation, a mini-review about surgical treatment modalities and their results can be a useful approach to identify the most effective surgical option in the management of ODP-maculopathy.
Keywords: optic disc pit, optic disc pit maculopathy, optic disc pit maculopathy treatments, optic nerve stuffing, post-operative outcomes, pars plana vitrectomy
Introduction
Optic disc pit (ODP) is considered to be part of the spectrum of rare congenital cavitary abnormalities of the optic disc, occurring in the majority of the cases on the temporal side of the optic disc.1 It is usually unilateral, sporadic in occurrence and can occur equally in men and women with an estimated prevalence of 1 out of 10,000 people.2
In the absence of other sequelae, many of the patients may remain asymptomatic and it may be found incidentally. Sometimes, the symptoms are generally limited to arcuate scotomas or enlargement of the blind spot in visual field tests.2–4 However, when ODP is complicated by maculopathy (ODP-M), it may cause significant visual deterioration. ODP-M is the term used to describe the existence of intraretinal and subretinal fluid at the macula as well as retinal pigment changes. It can occur in up to 25–75% of all cases.2–5 Regarding the pathophysiology of ODP-M and the origin of fluid, the exact mechanism remains unclear. It has been proposed that either vitreous or cerebrospinal fluid (CSF) may be responsible for macular detachment in eyes with OPD.6–8
When ODP-M is present, visual acuity (VA) is usually affected to 20/70 or worse,2,5,9–13 but in the untreated and long-standing cases, which can be associated with cystoid changes, lamellar or full-thickness macular holes, and retinal pigment epithelium (RPE) atrophy, the visual impairment is usually irreversible, leading to a reduced VA to 20/200 or worse in the affected eye.2,5,9-13 Therefore, interventions are valuable, as they may prevent significant visual loss in these patients. However, despite the improved insight into this unusual pathology, currently, there is no consensus regarding its optimal treatment. Maybe because the nature and the origin of the fluid causing the macular detachment are still controversial with no known triggers.2,5,9-13 The purpose of this mini-review is to discuss the possible surgical treatments options and the postoperative outcomes data of this challenging entity.
Conservative Management
In the management of ODP-M, especially in pediatric cases, a spontaneous resolution with an improvement of visual acuity is possible.14,15 Therefore, a more conservative approach with 3–6 months of follow-up before any surgical procedure could be appropriate. However, it must be kept in mind that the number of pediatric cases is small, relapses are frequent, and the prognosis remains poor in approximately 25% to 75% of the patients.2–5
Since patients with ODP may remain asymptomatic with normal visual acuity until 2nd to 4th decades of life2–5 an individualized approach should be considered in each case assessing the visual symptoms with the clinical and imaging findings, but currently, in the presence of progression of fluid accumulation and/or visual loss, observation is deemed unjustified.5,13
Surgical Treatment Options
Currently, there is no optimal accepted treatment for ODP-M because the pathogenesis of the disease is not yet fully understood. However, since vitreous traction, specifically the vitreopapillary traction,2,5,16–18 has been suggested to play an important role in the pathogenesis of ODP-M, pars plana vitrectomy (PPV) with the induction of posterior vitreous detachment (PVD) remains the most widely accepted treatment of choice for this entity.9–13,19–22 Tight vitreous attachment over the optic nerve has been reported in previous studies preoperatively by OCT and intraoperatively by iOCT in ODP-M patients.16,17,23 Therefore, inducing a PVD by PPV can relieve the traction exerted by the vitreous on either the macula or the ODP, facilitating the absorption of subretinal fluid. Most of the published literature on ODP-M is focused on PPV techniques which have evolved along with the breakthroughs.2,5,9-13 A summary of some published series of PPV and adjuncts treatments for ODP-M is given in Table 1.
 |
Table 1 Main Recent Series Describing Treatment for Optic Disc Pits with Maculopathy |
A wide array of adjuvant treatments, including injection of gas,20,21,24,25 air17 or silicone tamponade,26 juxtapapillary laser,20,24,27 retinal fenestration,28 glial tissue removal29 and macular internal limiting membrane (ILM) peeling,25,27,30 in combination with PPV have been tried with varying degrees of success.
The majority of these studies reported high anatomical success rates (50% to 95%) and similar functional results, with VA improvement in >50% of cases in routine cases.9–13,17,20,24–27,31,32 However, these adjuvant interventions are not exempt from risks and complications whilst successfully long-term anatomical results have been achieved with just PPV alone.19–22
In cases where a vitreous substitute is necessary, the use of gas would be a reasonable approach to prevent the migration into the brain or subretinal space.26,33–36 Thus, avoiding the use of perfluorocarbon liquid or silicone oil because of their lower surface tension and easier migration. Also, migration of gas is much less problematic and easy to manage than silicone oil or heavy liquid migration.
Temporal endolaser photocoagulation has been proposed as a treatment for ODP-M,20,24,27 with the reasoning that laser scars will act as a “permanent” barrier to prevent fluid from leaking into the macula. However, this method of treatment can cause significant visual field defects because of the damage over the maculopapular bundle.24,30,37 Furthermore, it has been reported that laser treatment does not aid in anatomical success.19,27,38 Peeling the ILM in these cases may result in a high incidence of macular hole creation, as well as anatomical changes of the macula including dimpling or damage to the inner retina.39 In addition, there are numerous surgical series showing excellent results without ILM peeling.23–25,40,41 Thus, this maneuver seems to be questionable and probably not essential in the treatment of most cases of ODP-M. Creation of an inner retinal fenestration28 or glial tissue removal,29 procedures that involve risk of optic nerve injury, fall short of providing adequate evidence to be recommended for ODP-M, as they did not show an increment in the surgical success rate.
Therefore, if the vitreous cavity is the source of the fluid in ODP-M, then the role of PPV + induction of PVD would be the most reasonable and effective treatment, as the adjuvant procedures may not confer any tangible added benefit over PPV alone.19–22
However, this vitreous traction hypothesis has some limitations as it cannot explain the recurrent cases of macular detachment after PPV + induction of PVD or even after the removal of tight vitreous adhesion at the ODP.28 Neither it can explain the ODP-M cases developed in patients with total PVD.
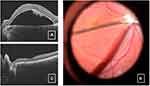
But if the source of the fluid is the CSF, then further explanation regarding the efficacy of PPV is needed.42 Maybe in those cases, the key point for obtaining a successful surgery could be the emergence of recent adjuvant treatments that are principally focused on sealing the pit. The justification for sealing the ODP with different materials such as ILM flap (Figure 1),14,41–46 fibrin glues47,48 or autologous fibrin,49 homologous scleral tissue50 or even silicone lacrimal plug,51 is based on the recent hypothesis postulated by Jain and Johnson,7 in which different pressure ranges between the eye and intracranial pressure can lead to migration of fluid from the vitreous cavity or CSF to intraretinal or subretinal space due to a defect either in the lamina cribrosa or the juxtapapillary area.7 Therefore, from a theoretical point of view, a procedure to create a “broad plug” along the “involved” disc margin could prevent the translaminar difference of pressure or block the outflow of fluids to the retinal layers or subretinal space.
However, even though reports describe successful anatomical and functional results that have been maintained long term in some cases, the restricted number of cases and low level of evidence limit the use of these methods.9–14,41–51
Our experience using the ILM flap technique in nine consecutive patients suggested a moderate rate of anatomical success, as 44% of our patients remained with unattached macula even 6 months after the surgery.14 However, published studies44,45 using the same technique have reported quick improvements and promising functional outcomes. Such differences might be related to the reduced function of the retinal pigment epithelium-Bruch’s membrane complex, as well as by degeneration within the retinal layers in chronic and/or refractory macular detachment patients.30,50
In some of these patients, we have observed a relapse. However, in those refractory cases, we have considered preferable to apply for another novel technique initially described by Travassos et al50 in which autologous scleral graft is used for sealing the pit with good initial outcomes (Figure 2).
The concept of these techniques would consist of covering the optic disc, including the ODP, creating a barrier to the fluid passage from the pit to the macular region. Although both techniques have demonstrated favorable long-term results, the use of ILM or scleral flap may be beneficial only in selected cases of optic pit maculopathy. However, the evidence remains low and more studies are warranted.
One of the main concerns that should be addressed in the future is the potential damage to the optic nerve and neurosensory retina caused by surgical trauma and/or the cytotoxicity of introducing different sealing materials into the ODP, as the majority of results are presented without visual field tests or macular sensitivity tests.14
Other Techniques
Pneumatic tamponade with or without laser photocoagulation is another therapeutic option for ODP-M.52 Theoretically, this dual treatment could ensure the induction of PVD, alleviating the vitreous tractions and facilitating the reattachment of the macula, and the formation of a barrage to seal the passage between the ODP and the macula.53 However, this technique has only reported retinal reattachment in approximately 50% of cases. Additionally, significant visual field defects and no improvement in VA have been reported after peripapillary barrier with photocoagulation.2,5,7
Macular buckling (MB) is another alternative for ODP-M and it has been reported a success rate of about 85% with long-term visual improvement and low rates of complications or recurrences.42,54–56 The macular buckle pushes the macular surface toward the vitreous cavity, preventing the entrance of fluid and alleviating vitreous tractions. It is worthy to note that MB seems to provide favorable results independently of the origin of the fluid in ODP-M. However, MB is considered a difficult and demanding technique and, for this reason, is not widely applied nowadays.9–13
Conclusions
ODP is a rare disease, and most of them are diagnosed incidentally.1,2,9-13 In patients with ODP-M, the prognosis is relatively poor, leading to visual loss in the untreated cases.2,9-13 In addition, the origin of the macular fluid and its triggers have yet to be understood. This lack of clarity has spawned a diversity of pathophysiology theories and treatment approaches with variable efficacy.9–13
Compared to other indications for vitreoretinal surgery, there is no established guideline for the treatment of OPD-M, neither is there a consensus on the most effective surgical technique.9–13 Additionally, the majority of the proposed adjuvant surgical techniques are challenging to perform. Convenience and comfort zones may affect the choice of treatment. Table 1 depicts the main treatment modalities for ODP-maculopathy.
Most of the reports about adjuvant treatments for ODP-M describe successful anatomical and functional results that have been maintained long term with a very low rate of recurrence and with very few postoperative complications in routine cases.9–13 However, limited experience exits for these alternative interventions and further studies are required to confirm these preliminary outcomes.
However, there is still a paucity of literature on the management of chronic and/or refractory cases, in which their outcomes may be limited by reduced function of RPE-Bruch´s membrane complex, photoreceptor apoptosis or by retinal layers’ degeneration. Most of the reports document the visual and anatomical improvements during the first two postoperative years. This is very important to the appropriate setting of patients’ expectations prior to surgery.
Certainly, the best clinical evidence to determine which treatment is superior in ODP-M patients should be obtained through a randomized clinical trial of different adjuvants surgical techniques to PPV. However, it is unlikely that such a trial can be performed as this is a very rare clinical entity.9–13
Nowadays, the gold standard for the treatment of ODP-M is still the PPV and PVD induction.9–13,19–22 Adjuvant procedures in combination with PPV are several and varied but they would probably be pertinent when the primary surgery fails.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gowdar JP, Rajesh B, Giridhar A, Gopalakrishnan M, Hussain R, Thachil T. An insight into the pathogenesis of Optic disc pit-associated maculopathy with enhanced depth imaging. JAMA Ophthalmol. 2015;133(4):466–469. doi:10.1001/jamaophthalmol.2014.6093
2. Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefe’s Arch Clin Exp Ophthalmol. 2011;249(8):1113–1122. doi:10.1007/s00417-011-1698-5
3. Brodsky M, Baker R, Hamed L. Pediatric Neuro-Ophthalmology.
4. Tawara A, Miyamoto R, Tou N, Ishibashi S, Kondo H. A classic temporal optic disc pit showing progression in the corresponding optic nerve fiber and visual field defects. Jpn J Ophthalmol. 2013;57(3):263–267. doi:10.1007/s10384-012-0225-5
5. Shah SD, Yee KK, Fortun JA, Albini T. Optic disc pit maculopathy: a review and update on imaging and treatment. Int Ophthalmol Clin. 2014;54(2):61–78. doi:10.1097/IIO.0000000000000025
6. Irvine AR, Crawford JB, Sullivan JH. The pathogenesis of retinal detachment with morning glory disc and optic pit. Retina. 1986;6(3):146–150. doi:10.1097/00006982-198600630-00002
7. Jain N, Johnson MW. Pathogenesis and treatment of maculopathy associated with cavitary optic disc anomalies. Am J Ophthalmol. 2014;158(3):423–435. doi:10.1016/j.ajo.2014.06.001
8. Sugar HS. An explanation. For the acquired macular pathology associated with congenital pits of the optic disc. Am J Ophthalmol. 1964;57(5):833–835. doi:10.1016/0002-9394(64)92235-4
9. Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology. 1990;97(11):1539–1542. doi:10.1016/S0161-6420(90)32380-1
10. Uzel MM, Karacorlu M. Optic disk pits and optic disk pit maculopathy: a review. Surv Ophthalmol. 2019;64(5):595–607. doi:10.1016/j.survophthal.2019.02.006
11. Chatziralli I, Theodossiadis P, Theodossiadis GP. Optic disk pit maculopathy: current management strategies. Clin Ophthalmol. 2018;12:1417–1422. doi:10.2147/OPTH.S153711
12. Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. Int J Retina Vitreous. 2015;1(1):1–9. doi:10.1186/s40942-015-0013-8
13. Kalogeropoulos D, Ch’ng SW, Lee R, et al. Optic disc pit maculopathy: a review. Asia Pac J Ophthalmol. 2019;8(3):247–255. doi:10.22608/APO.2018473
14. Yuen CHW, Kaye SB. Spontaneous resolution of serous maculopathy associated with optic disc pit in a child: a case report. J AAPOS. 2002;6(5):330–331. doi:10.1067/mpa.2002.127921
15. Bayar SA, Sezenöz AS, Pınarcı EY, Yılmaz G. Spontaneous regression of optic disc pit maculopathy in a six-year-old child. Turk Oftalmoloiji Derg. 2017;47(1):56–58. doi:10.4274/tjo.57614
16. Pastor-Idoate S, Gómez-Resa M, Karam S, et al. Efficacy of internal limiting membrane flap techniques with vitrectomy for macular detachment associated with an optic disc pit. Ophthalmologica. 2019;242(1):38–48. doi:10.1159/000495621
17. Pastor-Idoate S, Gil-Martinez M, yau K, Biswas S, Lloyd IC, Stanga PE. Pars plana vitrectomy with air tamponade for optic disc pit maculopathy: swept-source optical coherence tomography imaging findings and surgical approach: a clinical case. J Clin Exp Ophthalmol. 2015;06(01):2–6. doi:10.4172/2155-9570.1000397
18. Pinarci EY, Karacal H, Oncel B, Bayar SA, Karakaya M. The inner diameter of the optic disc pit decreases with pars plana vitrectomy. Int Ophthalmol. 2013;33(2):199–201. doi:10.1007/s10792-012-9656-8
19. Hirakata A, Inoue M, Hiraoka T, McCuen BW. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012;119(4):810–818. doi:10.1016/j.ophtha.2011.09.026
20. Teke MY, Citirik M. 23 gauge vitrectomy, endolaser, and gas tamponade versus vitrectomy alone for serous macular detachment associated with optic disc pit. Am J Ophthalmol. 2015;160(4):779–785.e2. doi:10.1016/j.ajo.2015.07.019
21. Bottoni F, Cereda M, Secondi R, Bochicchio S, Staurenghi G. Vitrectomy for optic disc pit maculopathy: a long-term follow-up study. Graefe’s Arch Clin Exp Ophthalmol. 2018;256(4):675–682. doi:10.1007/s00417-018-3925-9
22. Zheng A, Singh RP, Lavine JA. Surgical options and outcomes in the treatment of optic pit maculopathy: a meta-analysis and systematic review. Ophthalmol Retina. 2020;4(3):289–299. doi:10.1016/j.oret.2019.10.011
23. Gregory-Roberts EM, Mateo C, Corcóstegui B, et al. Optic disk pit morphology and retinal detachment: optical coherence tomography with intraoperative correlation. Retina. 2013;33(2):363–370. doi:10.1097/IAE.0b013e318263d0a6
24. Avci R, Yilmaz S, Inan UU, et al. Long-term outcomes of pars plana vitrectomy without internal limiting membrane peeling for optic disc pit maculopathy. Eye. 2013;27(12):1359–1367. doi:10.1038/eye.2013.172
25. Avci R, Kapran Z, Ozdek S, et al. Multicenter study of pars plana vitrectomy for optic disc pit maculopathy: MACPIT study. Eye. 2017;31(9):1266–1273. doi:10.1038/eye.2017.142
26. Kuhn F, Kover F, Szabo I, Mester V. Intracranial migration of silicone oil from an eye with optic pit. Graefe’s Arch Clin Exp Ophthalmol. 2006;244(10):1360–1362. doi:10.1007/s00417-006-0267-9
27. Abouammoh MA, Alsulaiman SM, Gupta VS, et al. Pars plana vitrectomy with juxtapapillary laser photocoagulation versus vitrectomy without juxtapapillary laser photocoagulation for the treatment of optic disc pit maculopathy: the results of the KKESH International Collaborative Retina Study Group. Br J Ophthalmol. 2016;100(4):478 LP- 483. doi:10.1136/bjophthalmol-2015-307128
28. Ooto S, Mittra RA, Ridley ME, Spaide RF. Vitrectomy with inner retinal fenestration for optic disc pit maculopathy. Ophthalmology. 2014;121(9):1727–1733. doi:10.1016/j.ophtha.2014.04.006
29. Inoue M, Shinoda K, Ishida S. Vitrectomy combined with glial tissue removal at the optic pit in a patient with optic disc pit maculopathy: a case report. J Med Case Rep. 2008;2:1–4. doi:10.1186/1752-1947-2-103
30. Rayat JS, Rudnisky CJ, Waite C, et al. Long-term outcomes for optic disk pit maculopathy after vitrectomy. Retina. 2015;35(10):2011–2017. doi:10.1097/IAE.0000000000000576
31. Kiang L, Johnson MW. Formation of an Intraretinal fluid barrier in cavitary optic disc maculopathy. Am J Ophthalmol. 2017;173:34–44. doi:10.1016/j.ajo.2016.09.025
32. Ghosh YK, Banerjee S, Konstantinidis A, Athanasiadis I, Kirkby GR, Tyagi AK. Surgical management of optic disc pit associated maculopathy. Eur J Ophthalmol. 2008;18(1):142–146. doi:10.1177/112067210801800126
33. Johnson TM, Johnson MW. Pathogenic implications of subretinal gas migration through pits and atypical colobomas of the optic nerve. Arch Ophthalmol. 2004;122(12):1793–1800. doi:10.1001/archopht.122.12.1793
34. Coll GE, Chang S, Flynn TE, Brown GC, Brown GC. Communication between the subretinal space and the vitreous cavity in the morning glory syndrome. Graefe’s Arch Clin Exp Ophthalmol. 1995;233(7):441–443. doi:10.1007/BF00180949
35. Salam AK-LD, Luff AJ. Superior retinal detachment in an oil-filled eye with a colobomatous optic disc. Retin Cases Brief Rep. 2008;2(2):124–125. doi:10.1097/ICB.0b013e3180338f0f
36. Dithmar S, Schuett F, Voelcker HE, Holz FG. Delayed sequential occurrence of perfluorodecalin and silicone oil in the subretinal space following retinal detachment surgery in the presence of an optic disc pit. Arch Ophthalmol. 2004;122(3):409–411. doi:10.1001/archopht.122.3.409
37. García-Arumí J, Corcóstegui Guraya B, Boixadera Espax A, Martínez Castillo V, Sararols Ramsay L, Motta RM. Optical coherence tomography in optic pit maculopathy managed with vitrectomy-laser-gas. Graefe’s Arch Clin Exp Ophthalmol. 2004;242(10):819–826. doi:10.1007/s00417-004-0897-8
38. Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology. 2005;112(8):1430–1435. doi:10.1016/j.ophtha.2005.02.013
39. Shukla D, Kalliath J, Tandon M, Vijayakumar B. Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina. 2012;32(7):1337–1342. doi:10.1097/IAE.0b013e318235d8fc
40. Chang S, Gregory-Roberts E, Chen R. Retinal detachment associated with optic disc colobomas and morning glory syndrome. Eye. 2012;26(4):494–500. doi:10.1038/eye.2011.354
41. Ravani R, Kumar A, Karthikeya R, et al. Comparison of inverted ILM-stuffing technique and ILM peeling alone for optic disc pit-associated maculopathy: long-term results. Ophthalmic Surg Lasers Imaging Retina. 2018;49(12):e226–e232. doi:10.3928/23258160-20181203-12
42. Theodossiadis GP, Chatziralli IP, Theodossiadis PG. Macular buckling in optic disc pit maculopathy in association with the origin of macular elevation: 13-year mean postoperative results. Eur J Ophthalmol. 2015;25(3):241–248. doi:10.5301/ejo.5000553
43. Mohammed OA, Pai A. Inverted autologous internal limiting membrane for management of optic disc pit with macular detachment. Middle East Afr J Ophthalmol. 2013;20(4):357–359. doi:10.4103/0974-9233.120008
44. D’Souza P, Babu U, Narendran V. Autologous free internal limiting membrane flap for optic nerve head pit with maculopathy. Ophthalmic Surg Lasers Imaging Retina. 2017;48(4):350–353. doi:10.3928/23258160-20170329-11
45. Nawrocki J, Bonińska K, Michalewska Z. Managing optic pit. the right stuff! Retina. 2016;36(12):2430–2432. doi:10.1097/IAE.0000000000001218
46. Caporossi T, Finocchio L, Barca F, Franco F, Tartaro R, Rizzo S. 27-gauge via pars plana vitrectomy with autologous ILM transplantation for optic pit disc maculopathy. Ophthalmic Surgery, Lasers and Imaging Retina. 2015;133(4):712–714. doi:10.1001/jamaophthalmol.2014.6093
47. De Oliveira PRC, Berger AR, Chow DR. Use of evicel fibrin sealant in optic disc pit-associated macular detachment. Ophthalmic Surg Lasers Imaging Retina. 2017;48(4):358–363. doi:10.3928/23258160-20170329-13
48. Almeida DRP, Chin EK, Arjmand P, Velez G, Evans LP, Mahajan VB. Fibrin glue and internal limiting membrane abrasion for optic disc pit maculopathy. Ophthalmic Surg Lasers Imaging Retina. 2018;49(12):e271–e277. doi:10.3928/23258160-20181203-18
49. Nadal J, Figueroa MS, Carreras E, Pujol P, Canut MI, Barraquer RI. Autologous platelet concentrate in surgery for macular detachment associated with congenital optic disc pit. Clin Ophthalmol. 2015;9:1965–1971. doi:10.2147/OPTH.S81976
50. Travassos AS, Regadas I, Alfaiate M, Silva ED, Proença R, Travassos A. Optic pit: novel surgical management of complicated cases. Retina. 2013;33(8):1708–1714. doi:10.1097/IAE.0b013e31828e699c
51. Deltour JB, Masse H, Lebreton O, Weber M. Successful use of a silicone lacrimal plug to treat a case of refractory macular detachment associated with a large optic disc pit. Acta Ophthalmol. 2020;98(1):e126–e127. doi:10.1111/aos.14116
52. Lei L, Li T, Ding X, et al. Gas tamponade combined with laser photocoagulation therapy for congenital optic disc pit maculopathy. Eye. 2015;29(1):106–114. doi:10.1038/eye.2014.245
53. Akiyama H, Shimoda Y, Fukuchi M, et al. Intravitreal gas injection without vitrectomy for macular detachment associated with an optic disk pit. Retina. 2014;34(2):222–227. doi:10.1097/IAE.0b013e3182993d93
54. Georgopoulos GT, Theodossiadis PG, Kollia A-CK, Vergados J, Patsea EE, Theodossiadis GP. Visual field improvement after treatment of optic disk pit maculopathy with the macular buckling procedure. Retina. 1999;19(5):370. doi:10.1097/00006982-199909000-00001
55. Theodossiadis GP, Theodossiadis PG. The macular buckling technique in the treatment of optic disk pit maculopathy. Semin Ophthalmol. 2000;15(2):108–115. doi:10.3109/08820530009040001
56. Theodossiadis GP, Theodossiadis PG. Optical coherence tomography in optic disk pit maculopathy treated by the macular buckling procedure. Am J Ophthalmol. 2001;132(2):184–190. doi:10.1016/S0002-9394(01)00997-7
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.