Back to Journals » Clinical Ophthalmology » Volume 14
Surgical Grade and Repeat Laser Peripheral Iridotomy Procedures with Risk Stratification and Educational Considerations
Authors Riley OF , Mamtora S , Carroll E, Luck J
Received 29 September 2020
Accepted for publication 19 November 2020
Published 8 December 2020 Volume 2020:14 Pages 4319—4323
DOI https://doi.org/10.2147/OPTH.S283370
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Oliver Francis Riley, Sunil Mamtora, Emma Carroll, Jon Luck
Ophthalmology Department, Royal United Hospital, Bath BA1 3NG, UK
Correspondence: Oliver Francis Riley
Ophthalmology Department, Royal United Hospital, Bath BA1 3NG, UK
Tel +44 1225 428-331
Email [email protected]
Background/Aims: Peripheral laser iridotomy (PLI) is a commonly performed procedure. While effective, repeat procedures (RPs) may be required for a variety of causes. We report the causes and rate of RP PLI and whether surgical grade is a risk factor.
Methods: Two years of retrospective data from 282 patients who had undergone PLI at a single UK ophthalmology department were retrieved using an electronic medical record system (Medisoft, Leeds, UK).
Results: A total of 253 patients underwent analysis with 20 requiring RPs. Our data identified a correlation between experience of the operating surgeon and an increase in RP rate, with statistical significance (p=0.036) observed between consultants and registrars. No other statistically significant risk factors were identified from our study. Prescriber preference for iopidine was observed. From our findings and the current literature, prognostic factors that appear to influence RP rate include surgical grade, patient compliance, Asian ethnicity, and anticoagulation.
Conclusion: RP rate increases in PLI when a junior surgeon is performing the procedure, and thus cases with established prognostic factors for RPs should have senior input. Formal and standardized YAG-laser training should be implemented alongside risk stratification of patients to improve both trainee education and patient care.
Keywords: iris, glaucoma, education, laser treatment
Introduction
Glaucoma is a group of conditions characterized by progressive damage to the optic nerve that occurs in an indicative pattern and results in associated changes in optic disk appearance and the visual field.1 Its pathogenesis is complex and commonly but not exclusively associated with elevated intraocular pressure (IOP) that leads to retinal ganglion necrosis and consequentially damage to both the optic nerve head and the retinal nerve–fiber layer.1 Peripheral laser iridotomy (PLI) is performed in patients with angle-closure glaucoma or narrow angles with or without the presence of glaucomatous optic disk damage. PLI is a regularly performed procedure, and is achieved by using a laser device to create an opening within the iris tissue to facilitate drainage of fluid from the posterior and anterior chambers.2,3 This equalization in eye pressure minimizes pupillary block and reduces the risk of angle-closure glaucoma.2
In medical education, there exists a well-established equipoise between the requirement of a trainee to learn and perform a medical procedure with the potential increased risk of complications.4 This phenomenon is observed throughout all medical specialities, such as endoscopy procedures, and also within ophthalmology itself, with an observed increase in posterior capsule–rupture rates during cataract surgery when performed by trainees.5,6 As such, measures to reduce complications are essential for both patient safety and to reduce the impact on the educational development of trainees.7 Such measures include simulated surgery, formal and standardized training, adequate supervision, and risk stratification of patients, such as the system developed to identify patients at high risk of posterior-capsule rupture in cataract surgery.5,8,9 Notably, UK trainees have reported a lack of exposure and variable training/teaching in laser procedures.10 PLI is agenerally well-tolerated procedure, but complications can occur, including IOP rises and repeat procedures (RPs).11
Our study sought to assess if the grade of operating surgeon impacted the likelihood of a patient requiring a RP PLI. If an association was to be observed, it may warrant a change to educational training and the need for senior input in patients identified as higher risk.
Methods
Retrospective data analysis was performed on 282 consecutive patients that had undergone PLI from 2018 to 2020 at the Ophthalmology Department of the Royal United Hospital, UK. The study was registered with the Royal United Hospital research team and received ethical and database approval (project ID 3431). Data were retrospectively gathered and anonymized with no identifiable information published, and thus patient consent was not required.12 Data gathered comprised patient age, sex, glaucoma diagnosis, if the patient had attended follow-up, if an RP had been performed, the documented reason for this if applicable, baseline and postprocedure IOP, grade of the operating surgeon, and if the patient had been prescribed iopidine. Failed patency was defined as “absence of iris transillumination in the documented location where PI had been performed.” Resistant IOP was defined as “persistently elevated IOP that failed to be reduced by performing an initial PI and was presumed to be due to a PI that was not of adequate size.”13 Preprocedural IOP was defined as the last documented IOP prior to procedure. Baseline IOP was defined as the documented IOP at 30–45 minutes postprocedure. IOP spike was defined as an increase in postprocedure IOP ≥8 mmHg.9 A non-clinical case manager scheduled PLI appointments based on chronicity, and thus patients and grades of operating surgeons were allocated randomly. Data analysis was performed to individually compare the RP rate between one grade of operating surgeon against another. This was performed on Microsoft Excel using the χ2 test to assess statistical significance, defined as p<0.05. Neither patients nor the public were involved in the design, conduct, reporting, or dissemination of our research.
In total there were 24 operating surgeons: four consultants, three associate specialists (ASpecs), 14 specialty registrars (SpRs), and two senior house officers (SHOs). As per UK medical training, defined grades of operating surgeons are 1–2 years of specialty training for SHOs and 3–7 years of specialty training for SpRs. ASpecs are middle- to senior-grade doctors who often work independently, but are attached to a clinical team led by a consultant, they are not on a formal training program nor do they hold a consultant post.14 A consultant is a senior doctor who has completed their specialty training, works independently, and has a role in delivering care services and teaching and training of junior doctors, and takes ultimate responsibility for patient care. We used grades of operating surgeon as a surrogate for surgical experience, which other studies have demonstrated to be an accurate comparator.15
Results
Of the 282 patients initially identified for the study, 253 were included and 29 excluded, due to a lack of follow-up data. Patients had a mean age of 67±11.7, 31% were male, and 81% had undergone bi-lateral PLI. Table 1 shows the demographic data. Twenty patients required RPs, due to failed patency (12), intraoperative bleeding (5), resistant IOP (2), and not tolerating prior procedure (2). The number of PLIs performed per grade of operating surgeon was 113 for consultants, 43 for ASpecs, 81 for SpRs, and seven for SHOs. Mean IOP was baseline 18.47±7.1 mmHg and postprocedure 17±4.9 mmHg. In sum, 21 IOP rises postprocedure were observed. Eight patients were prescribed iopidine postprocedure from two prescribers.
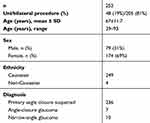 |
Table 1 Demographic Data of Patients |
Figure 1A demonstrates the rate of RPs by grade of surgeon, with an increase in RP rate observed with surgeons having less experience and seniority. When analysing RP rate per operating surgeon grade, statistical significance was found between consultants and SpRs (p=0.036, Figure 1B). No other statistically significant difference was found between grade of operating surgeon and RP rate. When comparing RP rates with other demographic data, including age, sex, baseline IOP, and ethnicity, no statistical significance was observed.
Discussion
Our data has identified a correlation between less experience of the operating surgeon and an increase in RP rate, with a statistically significant difference between SpRs and consultants observed. The difference in RP rate is also likely to be significant between consultants and SHOs, given their similar data distribution; however, it is likely that the low number of SHO PLI cases in our study failed to generate the statistical power necessary to demonstrate this. Our study’s mean baseline and postprocedure IOP values and IOP spikes were comparable to other studies.9,16 From the limited data on iopidine prescribing, a prescriber preference was observed.
Most research into prognostic factors for PLI and glaucoma has been within the acute setting, limiting its reliability in extrapolating it within our setting.17 Previous literature has found that age, sex, and baseline IOP are not independent prognostic factors for likelihood of requiring RPs, which our study’s findings also confirm.17 However, the literature has identified Asian ethnicity as an independent prognostic factor for increasing the likelihood of requiring RPs.9,18 When analyzing our data on ethnicity and RP rates, we observed no statistical significance, likely because of the small non-Caucasian population of the study (2%), which is representative of the local population, but differs from demographic data documented in other studies that have observed this difference.9 The difference in RP rate for Asian ethnicity observed in other literature is believed to be due to greater laser-energy requirement to penetrate the iris to perform an iridotomy on the thicker dark-brown irides, more common in the Asian population.9 Pretreatment argon-laser therapy has been suggested for this ethnic group when undergoing PLI in an attempt to thin and shrink the iris stoma.9
Assesment of the causes for patients requiring RPs within this study revealed that this was most commonly secondary to failed patency (60%), which may be explained by trainees performing smaller iridotomies, which are known to be at increased risk of closure.9,19 Existing literature has found trainees use significantly more laser energy when performing PLI, which is likely to cause an increase in both complications and RPs.9 Differences in laser energy when comparing iridotomy location and size have also been observed, which may contribute to the higher energy use observed in trainees, due to the lack of standardization when performing the procedure.9,20
The second–commonest cause for RPs within our study was intraoperative bleeding. While we did not investigate if patients had been taking anticoagulation periprocedurally, current literature demonstrates that patients that are anticoagulated are more likely to require RPs for PLI.21 Furthermore, pretreatment with argon laser has also been shown to reduce intraoperative bleeding in PLI; however, its significance when the patient is anticoagulated is not known.22 Another cause of RP PLI was patients not tolerating the procedure itself, which could potentially be anticipated prior to the procedure. This is an observed cause for RPs in other procedures, such as endoscopy and cataract surgery, with the patient instead receiveing a general anaesthetic.23,24 While this is not performed for PLI, senior involvement in this patient subcategory for other procedures has demonstrated an increase in patients tolerating procedures and reducing the need to proceed to general anesthesia.24
From this study’s findings and with reference to current literature, prognostic factors that appear to influence RP rate include surgical experience, patient tolerance, Asian ethnicity, and anticoagulation.9,21,23 Given that this study’s findings demonstrate that trainees have a higher RP rate, it would seem logical to implement a risk-stratification system for PLI cases, similar to systems already in place for cataract surgery. Pretreatment with argon-laser therapy may be of benefit to some of these high-risk RP patients. Additional formal teaching and standardization of laser procedures is likely to help bridge the lack of exposure to these cases reported by trainees, and may help reduce RP PLI cases, added to which there is now additional global interest in reducing hospital appointments during the COVID-19 pandemic.25
Limitations
The lack of PLI cases failed to generate enough statistical power to show a likely significant difference between other surgical grades and RP rate. Further limitations included poor documentation leading to limited conclusions concerning iopidine use and the limited diversity noted in the demographic population of our study.
Conclusion
RP-rate increases in PLI when a trainee is performing the procedure and thus cases where established risk factors have been identified should have senior input. Formal and standardzed laser training should be implemented alongside risk stratification of patients to improve both trainee education and patient care.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002;86(2):238–242. doi:10.1136/bjo.86.2.238
2. Michelessi M, Lindsley K. Peripheral iridotomy for pigmentary glaucoma. Cochrane Database Syst Rev. 2016. doi:10.1002/14651858.CD005655.pub2
3. RCOPHTH. Final commissioning guide: glaucoma (recommendations). Clinical Council for Eye Health Commissioning, NICE Accredited. 2016. Available from: www.rcophth.ac.uk/wp-content/uploads/2016/06/Glaucoma-Commissioning-Guide-Recommendations-June-2016-Final.pdf.
4. Wolf ZR, Hughes RG. Error Reporting and Disclosure. In: Hughes RG, Editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville (MD): Agency for Healthcare Research and Quality (US); April, 2008. Chapter 35. Available from: https://www.ncbi.nlm.nih.gov/books/NBK2652/.
5. Narendran N, Jaycock P, Johnston R, et al. The cataract national dataset electronic multicentre audit of 55 567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23(1):31–37. doi:10.1038/sj.eye.6703049
6. Brown C, Smith L, Watson D, Devitt P, Thompson S, Jamieson G. Outcomes for trainees vs experienced surgeons undertaking laparoscopic antireflux surgery - is equipoise achieved? J Gastrointest Surg. 2013;17(7):1173–1180. doi:10.1007/s11605-013-2211-8
7. Metcalfe J. Learning from errors. Annu Rev Psychol. 2017;68:465–489. doi:10.1146/annurev-psych-010416-044022
8. Darosa DA, Pugh CM. Error training: missing link in surgical education. Surgery. 2012;151(2):139–145. doi:10.1016/j.surg.2011.08.008
9. Kam JP, Zepeda EM, Ding L, Wen JC. Resident-performed laser peripheral iridotomy in primary angle closure, primary angle closure suspects, and primary angle closure glaucoma. Clin Ophthalmol. 2017;11:1871–1876. doi:10.2147/OPTH.S148467
10. Hoffman J, Spencer F, Ezra D, Day AC. Changes in UK ophthalmology surgical training: analysis of cumulative surgical experience 2009–2015. BMJ Open. 2017;7(10):e018526. doi:10.1136/bmjopen-2017-018526
11. Radhakrishnan S, Chen P, Junk A, Nouri-Mahdavi K, Chen T. Laser peripheral iridotomy in primary angle closure. Ophthalmology. 2018;125(7):1110–1120. doi:10.1016/j.ophtha.2018.01.015
12. World Medical Association. WMA declaration of helsinki – ethical principles for medical research involving human subjects. Current Policies. Available from: www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/.
13. Cumba R, Nagi K, Bell N, et al. Clinical outcomes of peripheral iridotomy in patients with the spectrum of chronic primary angle closure. ISRN Ophthalmol. 2013;1–9.
14. British Medical Association. A Charter for Staff and Associate Specialist and Specialty Doctors. Health Education England, NHS, 2014.
15. Maruthappu M, Gilbert BJ, El-Harasis MA, et al. The influence of volume and experience on individual surgical performance: a systematic review. Ann Surg. 2015;261(4):642–647. doi:10.1097/SLA.0000000000000852
16. Schwartz LW, Moster MR, Spaeth GL, Wilson RP, Poryzees E. Neodymium-YAG laser iridectomies in glaucoma associated with closed or occludable angles. Am J Ophthalmol. 1986;102(1):41–44. doi:10.1016/0002-9394(86)90207-2
17. Lee JW, Lee JH, Lee KW. Prognostic factors for the success of laser iridotomy for acute primary angle closure glaucoma. Korean J Ophthalmol. 2009;23(4):286–290. doi:10.3341/kjo.2009.23.4.286
18. Aung T, Ang LP, Chan SP, Chew PT. Acute primary angle-closure: long-term intraocular pressure outcome in Asian eyes. Am J Ophthalmol. 2001;131:7–12. doi:10.1016/S0002-9394(00)00621-8
19. Schiff GD, Galanter WL. Promoting more conservative prescribing. JAMA. 2009;301(8):865–867. doi:10.1001/jama.2009.195
20. Fleck BW. How large must an iridotomy be? Br J Ophthalmol. 1990;74(10):583–588. doi:10.1136/bjo.74.10.583
21. Carina T, Sanvicente M. Effect of anticoagulants and surgeon-related factors on short-term outcomes of laser peripheral iridotomy. Ophthalmol Glaucoma. 2019;2(4):204–209. doi:10.1016/j.ogla.2019.05.002
22. Kumar H, Sood NN, Kalra VK. Evaluation of argon pre-treatment for mode locked Nd- YAG laser peripheral iridotomy in angle closure glaucoma. Glaucoma. 1990;12:126.
23. Hazeldine S, Fritschi L, Forbes G. Predicting patient tolerance of endoscopy with conscious sedation. Scand J Gastroenterol. 2010;45(10):1248–1254. doi:10.3109/00365521.2010.497939
24. Ann Vann M, Ogunnaike BO, Joshi GP, Warltier DC. Sedation and anesthesia care for ophthalmologic surgery during local/regional anesthesia. Anesthesiology. 2007;107(3):502–508. doi:10.1097/01.anes.0000278996.01831.8d
25. Romano M, Montericcio A, Montalbano L, et al. Facing COVID-19 in Ophthalmology Department. Curr Eye Res. 2020;45(6):653–658. doi:10.1080/02713683.2020.1752737
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

