Back to Journals » Journal of Pain Research » Volume 13
Successful Treatment of Lumbar Radicular Pain with Selective Nerve Root Injection Using a Racz Catheter: A Case Report
Received 25 February 2020
Accepted for publication 10 April 2020
Published 28 April 2020 Volume 2020:13 Pages 843—845
DOI https://doi.org/10.2147/JPR.S251186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Donghwi Park,1 Min Cheol Chang2
1Department of Physical Medicine and Rehabilitation, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea; 2Department of Rehabilitation Medicine, College of Medicine, Yeungnam University, Daegu, Republic of Korea
Correspondence: Min Cheol Chang Email [email protected]
Purpose: Lumbar transforaminal selective nerve root injection (SNRI) is effective for controlling radicular pain. However, when a patient occasionally experiences severe foraminal stenosis, osteophytes cover the outside opening of the neural foramen, preventing clinicians from inserting a needle tip within the neural foramen.
Patients and Methods: An 81-year-old man complained of left L5 radicular pain (left thigh and calf) due to severe left L5-S1 foraminal stenosis. After failure of conventional transforaminal SNRI in the left L5 due to severe degenerative change in the lumbar spine, SNRI was performed using a Racz catheter. After inserting a 16-gauge cannula via the sacral hiatus, the Racz catheter was inserted. The tip of the catheter was positioned near the left L5 nerve root. After confirming the location of the needle tip using a contrast dye, 20 mg (40 mg/mL) of triamcinolone with 0.5 mL of 1% lidocaine and 2 mL of normal saline was injected.
Results: Immediately after the procedure, the patient’s pain completely disappeared. During the 1- and 2-month follow-ups, the patient reported only slight pain in the thigh and calf.
Conclusion: When it is not possible to perform a conventional transforaminal SNRI, SNRI using a Racz catheter can be an effective treatment option for controlling lumbar radicular pain.
Keywords: spinal stenosis, Racz catheter, selective nerve root injection
Introduction
Lumbar transforaminal selective nerve root injection (SNRI) is a highly target-oriented procedure, and its effectiveness has been well demonstrated in patients with lumbar spinal stenosis and herniated lumbar discs.1–4 In SNRI, the corticosteroid is injected near the target dorsal root ganglion and inflamed nerve root.1–4 Reducing inflammation around the nerve root is the main mechanism for alleviating radicular pain.
Lumbar transforaminal SNRI is performed under fluoroscopy guidance.5 The needle tip is positioned in the neural foramen, below the pedicle. The preferred target site for SNRI is the “safe triangle,” bordering the inferior aspect of the pedicle, the exiting nerve root, and the lateral margin of the vertebral body.5 However, patients with severe foraminal stenosis and osteophytes covering the outside opening of the neural foramen are occasionally encountered in clinical practice. In these patients, it is difficult for the pain physician to insert the needle tip within the neural foramen.
Here, we report a case of a patient with lumbar radicular pain due to severe foraminal stenosis, who was successfully treated with SNRI using a Racz catheter after a failed transforaminal SNRI.
Case Report
An 81-year-old man visited the Spine Center at our university hospital for left lumbar radicular pain since 1 month and which had been recently aggravated. He experienced a piercing pain in the left lateral thigh and calf. The numeric rating scale (NRS) score was 7 on 10. His pain was aggravated during walking. On physical examination, he had no significant motor or sensory deficits. Knee and ankle jerks were normal, bilaterally. Magnetic resonance imaging revealed severe foraminal stenosis at the left L5–S1 (Figure 1A).1 The left L5 nerve root was collapsed. An electrodiagnostic study showed left L5 radiculopathy. Considering the pain experienced by the patient and the results of the imaging and electrodiagnostic studies, we determined that the patient’s pain was induced by a left L5-S1 foraminal stenosis. Written informed consent was provided by the patient for the publication of the case report and the accompanying image. The institutional approval was required to publish the case details, and our study was approved by the institutional review board of Yeungnam University hospital.
To alleviate the patient’s pain, we attempted to perform transforaminal SNRI in the left L5 nerve root. The patient was placed in a prone position, and a C-arm fluoroscope (Siemens, Erlangen, Germany) was used to identify the needle (25-gauge, 90 mm spinal needle) insertion point. We attempted to insert the needle tip within the left L5-S1 neural foramen below the left L5 pedicle but did not succeed due to severe left L5-S1 foraminal stenosis with osteophytes covering the outside opening of the left L5-S1 neural foramen. Additionally, SNRI with infra-neural approach was attempted, but failed. Therefore, we administered oral medication (meloxicam 15 mg, pregabalin 150 mg, acetaminophen/tramadol hydrochloride 1300/150 mg) to control the radicular pain, with no success.
One month later, we performed SNRI using a Racz catheter with aseptic technique (Epimed International Inc., Gloversville, NY). After identifying the sacral hiatus under lateral fluoroscopic guidance, local infiltration anesthesia was induced at the cannula insertion site. A 16-gauge cannula was inserted into the epidural space via the sacral hiatus, and the cannula tip was advanced below the S3 neural foramen. Then, the Racz catheter was connected to the cannula. The tip of the catheter was bent at a 15-degree angle to facilitate steering. Under anteroposterior fluoroscopic guidance, the catheter tip was advanced toward the left ventral lateral epidural space. We placed the catheter tip below the left L5 pedicle, through which the left L5 nerve root passed posteriorly. Through the injection of a contrast dye via the catheter, the correct position (near the left L5 nerve root) of the needle tip was confirmed (Figure 1B). Then, 20 mg (40 mg/mL) of triamcinolone with 0.5 mL of 1% lidocaine and 2 mL of normal saline was injected. The procedure took approximately 15 minutes. Immediately after the procedure, the patient’s pain completely disappeared. At the 1-, 2-, and 3-month follow-ups after SNRI using a Racz catheter, the patient reported only slight pain in the left lateral thigh and calf (NRS score: 1).
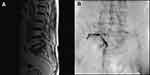 |
Figure 1 (A) T2-weighted sagittal magnetic resonance imaging showing left L5-S1 foraminal stenosis. (B) Left L5 selective nerve root injection using a Racz catheter. |
Discussion
In the current case, we successfully managed to alleviate left L5 radicular pain induced by severe foraminal stenosis with SNRI using a Racz catheter. We had to perform this procedure since we could not perform a conventional transforaminal SNRI due to osteophytes covering the left L5-S1 neural foramen. After the procedure, the patient’s pain reduced from an NRS score of 7 to 1.
The Racz catheter was developed by Racz and Holubec in 1989. Originally, it was used for percutaneous epidural adhesiolysis and neuroplasty.6 To date, many studies have shown that using a Racz catheter for percutaneous epidural adhesiolysis and neuroplasty is safe and effective for managing lumbar radicular pain in several spinal disorders, such as post laminectomy syndrome, epidural adhesions, herniated lumbar disc, and spinal stenosis.7–9 It is also known to be more effective against refractory radicular pain than conventional epidural steroid injection because it can chemically and mechanically eliminate adhesions and fibrous tissue that might hinder the spread of injected materials into the target area by placing the catheter tip near the target area.7–9 Besides this advantage of the Racz catheter, we showed that when conventional transforaminal SNRI is not possible due to severe degenerative changes, SNRI can be performed using a Racz catheter for effectively controlling lumbar radicular pain.
However, some adverse effects associated with the use of the Racz catheter have been reported.10 Bleeding in the epidural space, penetration of the dura, subdural insertion of the catheter, infection at the site of penetration, epidural abscess, headache, and hypotension can develop after the procedure.10 Moreover, direct nerve injury may occur, although it has been rarely reported.11 Therefore, particularly in patients with severe spinal stenosis, clinicians should not advance or push the Racz catheter forcibly. Similarly, the catheter should be slowly and carefully withdrawn. Radiation exposure is greater during transforaminal SNRI using a Racz catheter than during conventional transforaminal SNRI. Hence, clinicians should be cognizant of radiation exposure and try to minimize the radiation dose.
Funding
The present study was supported by a National Research Foundation of Korea grant funded by the Korean government (grant no. NRF-2019R1F1A1061348).
Disclosure
The authors have no conflicts of interest to report.
References
1. Chang MC, Lee DG. Outcome of transforaminal epidural steroid injection according to the severity of lumbar foraminal spinal stenosis. Pain Physician. 2018;21(1):67–72. doi:10.36076/ppj.1.2018.67
2. Dhakal GR, Hamal PK, Dhungana S, Kawaguchi Y. Clinical efficacy of selective nerve root block in lumbar radiculopathy due to disc prolapse. J Nepal Health Res Counc. 2019;17(2):242–246. doi:10.33314/jnhrc.v0i0.1976
3. Eckel TS, Bartynski WS. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009;12(1):11–21. doi:10.1053/j.tvir.2009.06.004
4. Ko S, Kwon J, Lee Y, Chae S, Choi W. Comparison of pain-reducing effect after selective nerve root block according to the type of lumbar foraminal stenosis. Clin Spine Surg. 2019;32(2):E60–E64. doi:10.1097/BSD.0000000000000723
5. Lee JW, Kim SH, Choi JY, et al. Transforaminal epidural steroid injection for lumbosacral radiculopathy: preganglionic versus conventional approach. Korean J Radiol. 2006;7(2):139–144. doi:10.3348/kjr.2006.7.2.139
6. Racz GB, Holubec JT. Lysis of adhesions in the epidural space. In: Racz GB, editor. Techniques of Neurolysis. Boston, MA: Springer; 1989:57–72. Current Management of Pain, vol 4.
7. Akbas M, Elawamy AR, Salem HH, Fouad AZ, Abbas NA, Dagistan G. Comparison of 3 approaches to percutaneous epidural adhesiolysis and neuroplasty in post lumbar surgery syndrome. Pain Physician. 2018;21(5):E501–E508.
8. Choi E, Nahm FS, Lee PB. Evaluation of prognostic predictors of percutaneous adhesiolysis using a Racz Catheter for post lumbar surgery syndrome or spinal stenosis. Pain Physician. 2013;16(5):E531–6.
9. Cho PG, Ji GY, Yoon YS, Shin DA. Clinical effectiveness of percutaneous epidural neuroplasty according to the type of single-level lumbar disc herniation: a 12-month follow-up study. J Korean Neurosurg Soc. 2019;62(6):681–690. doi:10.3340/jkns.2019.0070
10. Talu GK, Erdine S. Complications of epidural neuroplasty: a retrospective evaluation. Neuromodulation. 2003;6(4):237–247. doi:10.1046/j.1525-1403.2003.03031.x
11. Lim YS, Jung KT, Park CH, Wee SW, Sin SS, Kim J. Acute motor weakness of opposite lower extremity after percutaneous epidural neuroplasty. Korean J Pain. 2015;28(2):144–147. doi:10.3344/kjp.2015.28.2.144
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
